What Are The Symptoms Of Psychosis
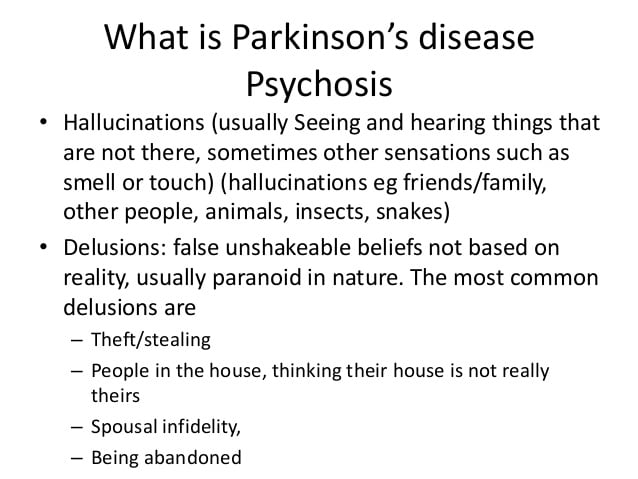
Two of the most prominent symptoms are hallucinations and delusions.7 Hallucinations involve seeing, hearing, experiencing or sensing things that are not really there. Delusions are false beliefs that are not based in reality. In describing symptoms of Parkinson’s disease psychosis, patients may use such common terms as: seeing things, paranoia, flashbacks, nightmares, false beliefs, or not being in touch with reality.8
Can Hallucinations Be Treated
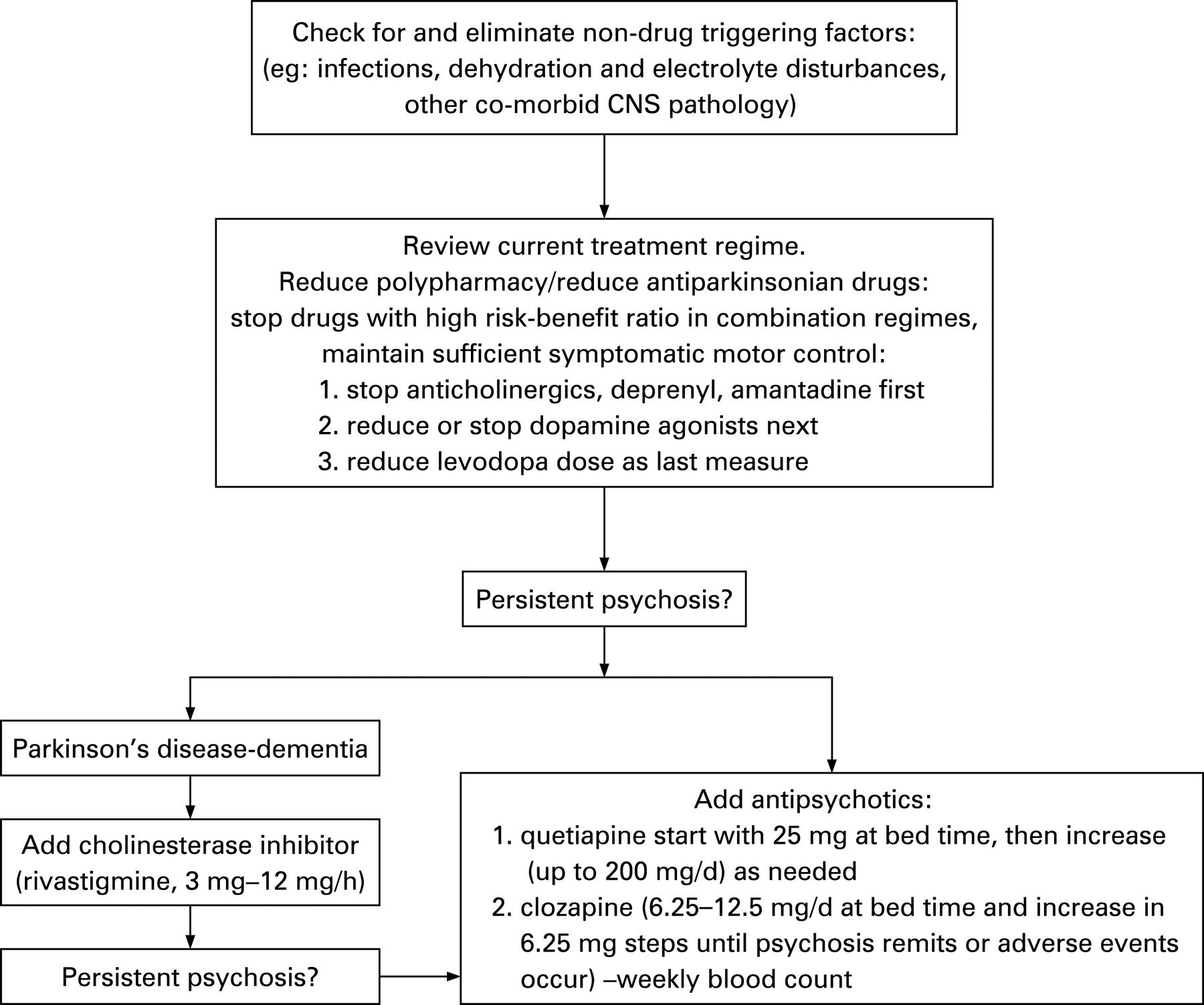
The treatment for hallucinations consists primarily of removing any existing medical cause, especially reducing or stopping any triggering pharmacological cause – for example by reducing a dose or discontinuing treatment with a certain drug. If the increase in motor symptoms then becomes troublesome, a return to the earlier anti-Parkinson’s drug may be considered, but with the addition of an atypical neuroleptic drug.
Most neuroleptics can worsen Parkinson’s and are forbidden when treating people with the condition. Medications for dementia can also reduce the incidence of illusions and hallucinations when there is underlying cognitive impairment. Parkinson’s treatments are developing fast and it is likely that we will see even more effective ways of avoiding and treating hallucinations in the coming years.
The most important thing is to report hallucinations to your doctor or nurse, and to discuss if they should be treated in some way.
Managing Hallucinations And Delusions
Get medical advice. In mild cases simple monitoring may be all that is required. In more severe cases changes in medications may be necessary.Rule out other causes such as eyesight issues or infections.Talk to your family and or carers to help them understand how you are feeling. It can help them to be more patient and supportive with you too.Try not to worry.Reassure yourself that these symptoms may be a side effect of Parkinson’s medication.Seek counselling. People with Parkinson’s, carers and family members may need support, counselling and specific advice. Medicare covers 6 – 12 sessions with a psychologist to provide a range of strategies to help.
Support for you
Tips For Living With Hallucinations
It is important for people with PD to talk about hallucinations with their family and care team, because they are manageable and can be troublesome if not treated. Discuss all possible symptoms with your doctor, no matter how minor, rare or bizarre you may think they are.
- Good lighting and stimulating activities in the evening can help keep hallucinations at bay.
- While a hallucination is occurring, caregivers can help their loved one by reassuring them that they will be safe and validating their partner’s experience. For example, say, “I’ll take the cat outside” instead of arguing that there is no cat.
Whats The Difference Between Corticobasal Degeneration And Parkinsons
The main difference between CBD and Parkinson’s is that it usually starts on one side with the gradual loss of use of one hand or leg , and there may be little flicks of involuntary muscle jerks. Walking and balance difficulties usually occur later in CBD than in Parkinson’s. Also, in CBD, a person may have trouble with purposeful movements, such as buttoning a shirt or cutting food.
For more information on corticobasal degeneration, read this information page.
Parkinsons Disease Psychosis: A Little
One of the lesser-known symptoms of Parkinson’s Disease is Parkinson’s psychosis. This webpage explains the prevalence, causes and symptoms, treatment options of PD psychosis. More useful to caregivers are sections on potential triggers of psychotic episodes and what caregivers can do about PD psychosis.
Parkinsons Disease Psychosis: Hallucinations Delusions And Paranoia
As part of Parkinson’s Disease and its treatment, hallucinations, illusions, delusions, suspiciousness and paranoid behaviors occur in over 50% of patients. In this 1-hour webinar Dr. Christopher Goetz suggests lifestyle changes, medication adjustments and a recently FDA approved drug to specifically treat psychosis in Parkinson’s Disease.
What Should I Do When My Loved One Is Experiencing A Hallucination
Most importantly, don’t try to convince your loved one that what they’re experiencing isn’t real. They’ll feel like you’re putting down an experience that seems authentic to them.
Once a person has lost insight, it’ll be very difficult to convince them that what they’re experiencing isn’t happening. Trying to argue with them may agitate and even enrage the person. Making them anxious could cause their hallucinations to get worse.
Instead, talk to the person gently and reassuringly. You might say something like, “I understand that you see a dog in the corner of the room. Everything is going to be OK. You’re safe.” You might even say that the dog must have left already.
Remember that the person can’t control what they’re experiencing. Try to be as sympathetic as you can when you talk to them.
One approach that can help is to turn on all the lights in the room. Hallucinations are more likely to happen in dimly lit areas, and this can be caused by disease-related changes that affect the eyes.
Then, have the person really focus on what they’re seeing. That may reset their brain and help them see what’s actually in front of them.
If the person doesn’t have insight, try a distraction. Move them to a different room. Turn on the TV or play a game they like.
Try to keep your loved one as calm as possible. If they become very agitated or violent, call their doctor or 911.
What Are Delusions
Delusions are illogical, irrational, dysfunctional views or persistent thoughts that are not based in reality. They are not deliberate and are very real to the person with PD. People with delusions who feel threatened may become argumentative, aggressive, agitated or unsafe.
- Delusions are less common in PD than visual hallucinations. They affect about eight percent of people with PD.
- Compared to hallucinations, delusions tend to be more complicated, present a greater risk for behavioral disturbances and safety concerns, are typically more difficult to treat and represent a more obvious deterioration or decline in one’s condition.
- Delusions can begin as generalized confusion at night. Over time, confusion can develop into clear delusions and behavioral disturbances during the day.
- All forms of delusions can be seen with PD, although delusions of jealousy and persecution are most widely reported and represent a greater challenge for treatment. These delusions can lead to aggression, which can pose a serious safety risk to the person with PD, family members and caregivers.
- Paranoia can lead to medication noncompliance — a person refusing to take medications, believing they are poisonous or deadly.
- Delusions can be associated with dementia. As a result, people with delusions are often confused and extremely difficult to manage. In these cases, many caregivers require outside assistance.
Simple Tips To Sleep Better
Medications can manage your hallucinations so you can sleep better — and vice versa. But don’t forget that sleep hygiene matters, too. These simple tips should help anyone with sleep problems:
- Sleep only as much as you need to feel refreshed.
- Wake up at the same time every day.
- Exercise daily — but not close to bedtime.
- Keep your bedroom cool.
- Limit fluid and avoid caffeine in the evening.
- If you’re hungry before bed, have a light snack.
- Get out of bed if you feel angry or frustrated.
Â
Parkinsons Disease Signs And Symptoms: Before The Diagnosis
Mindy Bixby
Neurologist, Mindy Bixby, DO, discusses the early signs and symptoms of Parkinson’s Disease, commonly referred to as non-motor symptoms.
Dr. Bixby explains how to identify and differentiate these symptoms from other disorders and when it’s time to visit your doctor for an accurate diagnosis.
She also covers therapy and treatment options if diagnosed with Parkinson’s Disease or other movement disorders.
Tags
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
What Are The Surgical Treatments For Parkinsons Disease
What Is The Outlook For Persons With Parkinsons Disease
The future is hopeful. Some of the research underway includes:
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Gait And Balance Problems
One of the most debilitating effects of Parkinson’s disease is the loss of coordination and control in body movements, which in many cases leads to severe walking disabilities. Although gait symptoms can vary among patients, there are some commonly observed movements. These include a tendency to lean or stoop forward while walking, dragging and shuffling of feet, and a decreased arm swing.
How Is Psychosis Managed
The urgency of treatment will depend on the type and characteristics of psychosis. Sometimes, when the hallucinations are mild and benign, and insight is retained, it is best that the Parkinson regimen be kept as is. However, when a patient is experiencing more threatening paranoid delusions, then more aggressive treatment is warranted .
The management of psychosis includes:
General Psychosis And Pd Psychosis
With regard to the clinical definition of the main features of psychosis, which include hallucinations, illusions, and delusions, current ICD-10 guidelines define hallucinations as a disorder characterised by a false sensory perception in the absence of an external stimulus, whereas an illusion is regarded as a misperception of an externally present stimulus. In contrast to classical hallucinations and illusions, delusions are a false interpretation of the experienced misperceptions, often involving topics of persecution, imposters, or grandiosity. Some specific forms of delusions such as the Cotard syndrome , Capgras syndrome , and Othello syndrome have further been named , the latter showing an association with dopamine agonist therapy and an improvement after its reduction. The current diagnostic criteria from ICD-10 based guidelines for acute and transient psychosis are shown in ; other definitions of psychosis falling under the term of schizoaffective disorders will not be further developed in this review.
The ICD-10 classification of mental and behavioural disorders: definition criteria for acute and transient psychosis. F23, F30, F32: diagnosis codes of psychotic and mood disorders taken from ICD-10 guidelines; reference: taken from WHO International classifications, ICD-10 guidelines .
Proposed criteria for psychosis in Parkinson’s disease. PD, Parkinson’s disease; UK, United Kingdom; references: Ravina et al., 2007, and Fenelon et al., 2008 .
Selfcare For The Person With Parkinsons
- Join a Parkinson’s support group if you don’t already belong to one. Talk about your experiences, ask for help if you need it and share what’s worked and not worked for you.
- Offer to have coffee with someone you know has been newly diagnosed and offer them support and encouragement.
- Make time to exercise and get out in nature every day.
- Communicate frequently with your doctors and discuss the possibility of tweaking your medications if your symptoms become worse.
- Rest when you need it.
- Plan a day trip or a vacation and get away from your normal surroundings.
- Take control where you can and keep authoring your own story.
- Practice or or Tai Chi to relax and calm your mind.
- Start a new project that you’re excited to work on every day.
- Communicate with your care partners and let them know how they can best help you.
Comparison Of Hallucinators And Non
The patients with isolated minor hallucinations were compared with the patients with no hallucinations . The only significant difference was a higher CES-D score in the group with minor hallucinations . When the presence of depression was determined using the cut-off values of the CES-D, depression was more frequent in the patients with minor hallucinations than in the patients without any hallucinations , but this difference did not reach significance.
The patients with formed visual hallucinations are compared with the non-hallucinators in Table 5. Patients with visual hallucinations differed in a number of respects: they were older, had a longer duration of disease, had a more severe motor state, had more depressive symptoms, and were more likely to have cognitive impairment, day-time somnolence and a history of ocular pathology. They were less likely to receive anticholinergics or selegiline and received a higher daily dose of levodopa, but the levodopa-equivalent dose did not differ significantly between the two groups. Visual hallucinations were recorded in 70% of the patients with dementia versus 10% of non-demented patients , and in 55% of the patients with severe cognitive disorders versus 8% of the patients with absent or moderate cognitive impairment .
The patients with hallucinations of any type were compared with the patients with no hallucinations. The results were identical to those of the preceding analysis, except for the degrees of significance .
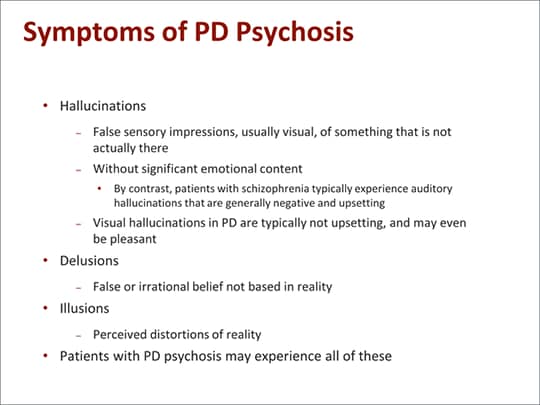
Hallucinations And Delusions In Pd
Hallucinations and delusions are collectively referred to as psychosis.
Visual hallucinations are the most common type of hallucination. In a visual hallucination, someone sees things that are not actually there. There can also be auditory and olfactory hallucinations. Often hallucinations are not alarming to the person experiencing them.
Delusions are when there is an alternative view of reality: an entire irrational story is created. Paranoia is a common type of delusion. Capgras delusions are a specific type of delusion where the person believes that a spouse, adult child, or other family member has been replaced by an imposter.
Types Of Hallucinations In People With Parkinsons Disease
Hallucinations involve the five senses: sight, smell, touch, hearing, and taste.
People with hallucinations have sensory experiences that feel real to them, but are not actually happening and are not apparent to anyone else.
Types of hallucinations include:
- Auditory: Hearing things
- Gustatory: Tasting things
For people who experience Parkinson’s-related hallucinations, the hallucinations are usually visual. They are typically non-threatening, but less commonly they can be of a threatening nature.
Often people with Parkinson’s disease see small people or animals, or loved ones who have already died. They are not interacting with them, just being observed.
Auditory hallucinations are more common in people with schizophrenia, but can happen with Parkinson’s disease. With Parkinson’s disease, auditory hallucinations are usually accompanied by visual hallucinations.
More specific types of hallucinations experienced by people with Parkinson’s disease include:
Pathophysiology Of Pd Psychosis
The pathophysiological processes underlying PD psychosis can be subdivided into intrinsic and extrinsic . While intrinsic PD psychosis is thought to be caused by alterations in dopamine, serotonin, and acetylcholine systems involving subcortical projections as well as synaptic and neuronal changes in limbic and cortical structures , extrinsic PD mainly involves dopaminergic or anticholinergic therapies, especially dopamine agonists .
To better understand the neurotransmitter dysfunctions underlying the development of hallucinations, the effect of hallucinogenic agents with known mechanisms of actions is of advantage. Classically, hallucinogenic agents were subdivided into those affecting the cholinergic system and those involving the aminergic system, herein dopaminergic and serotoninergic agents being included . The described clinical characteristics and associated hallucinations caused by these two distinct systems also differ: while the effects caused by anticholinergic agents are associated with peripheral autonomic features, confusion, disorientation, and visual hallucinations, mostly poorly formed and of a threatening nature, the symptoms caused by aminergic agents are characterised by a heightened awareness of objects, forms, and colours with a clear sensorium, sometimes involving the presence of hypnagogic phenomena of a dream-like quality .
Parkinsons Diseaseassociated Pathological Changes In The Cerebellum
The presence of dopaminergic innervation and dopamine D1–3 receptors in the cerebellum has been proven . The cerebellum receives a dopaminergic projection from the ventral tegmental area/substantia nigra pars compacta . Pathological changes in the cerebellum following dopaminergic degeneration were reported in patients with Parkinson’s disease and animal models.Rollandet al. showed that degeneration of nigrostriatal dopaminergic neurons causes dysfunction of both the basal ganglia–thalamic and cerebello-thalamic pathways in 6-hydroxydopamine-lesioned rats and MPTP monkeys. Neuronal degeneration in the cerebellum was shown in an MPTP mouse model , characterized by the loss of Nissl-stained Purkinje cells and aggravated by the number of repeated MPTP injections. An MPTP insult also induced the loss of calcium-binding positive Purkinje cells in monkeys . A recent study found that persistent hyperactivation of Purkinje cells correlated with the level of dopaminergic neuronal loss in the substantia nigra in chronic parkinsonian monkeys .
How Common Is Parkinson’s Disease Psychosis
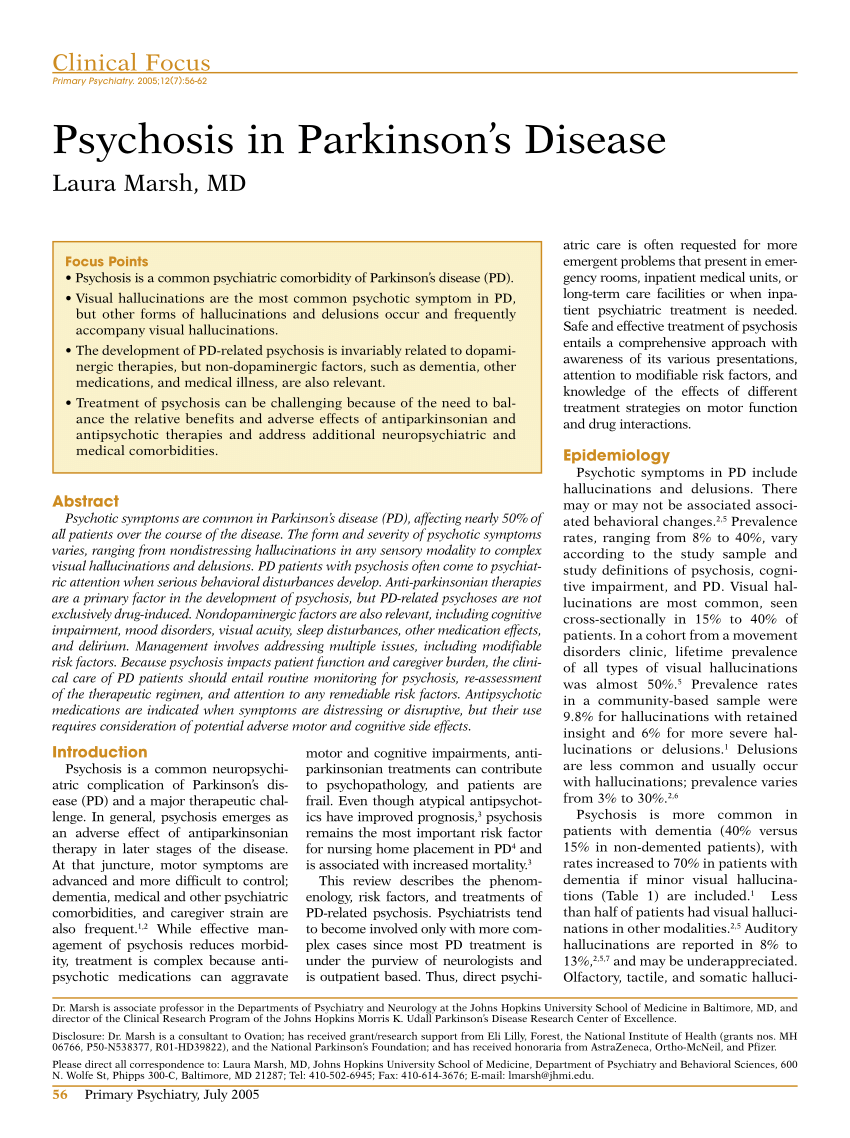
Between 20-40% of people with Parkinson’s report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include “delirium,” in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and “isolated minor symptoms” or “minor hallucinations,” including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinson’s. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinson’s not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinson’s is a complex disease and as it progresses the percentages and risk of symptoms will change.
The Cause Of Parkinsons Delusions And Hallucinations
Some risk factors associated with the development of psychosis in Parkinson’s disease include:
- Age: Parkinson’s disease usually occurs in people over age 60.
- Duration and severity of Parkinson’s disease: Psychosis is more common in advanced or late-stage Parkinson’s disease.
- Later : Occurring later in life
- Hyposmia: A decreased sense of smell
- Cognitive impairment: Problems with thinking, including trouble remembering, difficulty learning new things, difficulty concentrating, problems making decisions that affect everyday life
- Depression: People who have both depression and Parkinson’s disease are at a greater risk of developing psychosis.
- Diurnal somnolence: Daytime sleepiness
- REM sleep behavior disorder: A sleep disorder in which you physically act out dreams; involves making vocal sounds and sudden, often extreme, arm and leg movements during REM sleep
- Visual disorders: Impaired vision
- Severe axial impairment: Speech, swallowing, balance, freezing of gait
- Autonomic dysfunction: Impairment of the autonomic nervous system , which controls involuntary or unconscious actions such as heart rate, breathing, body temperature, blood pressure, digestion, and sexual function
- High medical comorbidity: The existence of more than one condition or illness in the same person at the same time; with Parkinson’s disease, may include conditions such as dementia, depression, and sleep disorders
The Cerebellum As A Target For Parkinsons Disease Treatment
While cerebellar dysfunction might contribute to some motor and non-motor signs in Parkinson’s disease, a possible approach for treating parkinsonian symptoms is to attempt to normalize cerebellar function. Surgical treatment, such as deep brain stimulation of the subthalamic nucleus or globus pallidus improves the motor signs and normalizes cerebellar activation. Levodopa administration can also normalize the activity and connectivity in the cerebello-thalamo-cortical circuit . However, whether it is reduced compensation or alleviation of pathological impairment as a consequence of effective treatment remains unclear. Suppressing cerebellar activity should theoretically answer the question: improvement would mean that the cerebellum is contributing to the manifestations; worsening would mean that the cerebellar activity is compensatory. We suppose that if the main efforts of the cerebellum in Parkinson’s disease are compensatory, suppression of cerebellar activity should be accompanied by further impairments of Parkinson’s disease symptoms.
Examples Of Delusions In Pd
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinson’s psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhall’s description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinson’s disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the person’s feelings.
- Listen to the person, don’t interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they don’t feel cornered or threatened.
- Make an “emergency plan” ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Brain Scan Could Identify Which Parkinsons Patients Benefit Most From Treatment
A new brain scan could help scientists identify which Parkinson’s patients would benefit most from a drug used to treat attention deficit hyperactivity disorder .
The scan can allow researchers to better visualise changes in the part of the brain linked to cognitive decline, a study has suggested.
While previous work has shown atomoxetine – used for people with ADHD – can be advantageous to some Parkinson’s sufferers, until now there has not been an easy way to identify those it might help the most.
The study, funded by the charity Parkinson’s UK and published in the journal Brain, was hailed by one of the researchers as an “exciting step towards individualised therapy for cognitive decline” because it helps identify the people the treatment is most suitable for.
The use of atomoxetine improved the ability to inhibit behaviour – to let the brain “stop and think” before doing the right thing, the charity said.
Improvements with the drug were especially profound in people with the most damage to the locus coeruleus – the region of the brain linked to cognitive decline.
They had lower natural levels of noradrenaline – a brain chemical affected in Parkinson’s which is responsible for processing thoughts and behaviour.
An imbalance of noradrenaline can lead to difficulty concentrating, forgetting things and taking longer to think and process information, or can cause a change in behaviour.
Research Roundup: Two Types Of Parkinsons Disease And More
Every week there are numerous scientific studies published. Here’s a look at some of the more interesting ones.
Parkinson’s Disease is Actually Two Diseases
Researchers from Aarhus Universityin Denmark indicating that Parkinson’s disease is actually two types of the disease. This helps explain why there are so many different symptoms and pathways. Parkinson’s is marked by slow deterioration of the brain from accumulation of alpha-synuclein, a protein that damages nerve cells. This causes slow, stiff movements. Some patients apparently have damage to the brain’s dopamine system before damage in the intestines and heart occurs. Other patients have damage to the nervous systems of the intestines and heart before the damage in the brain’s dopamine system. The research was published in the journal .
“With the help of advanced scanning techniques, we’ve shown that Parkinson’s disease can be divided into two variants, which start in different places in the body,” said Per Borghammer, professor of clinical medicine at Aarhus University. “For some patients, the disease starts in the intestines and spreads from there to the brain through neural connections. For others, the disease starts in the brain and spreads to the intestines and other organs such as the heart.”
Epigenetic Changes May Explain Why Humans Live Longer than Other Primates
Biomarker for Neurodegeneration Identified in the Eye
Children and Adults Have Two Distinct Immune Responses to COVID-19
