A Guide To Understanding End
Crossroads Hospice & Palliative Care created guidelines to help family caregivers better understand the physical changes of the end-of-life process, as well as the emotional and spiritual end-of-life changes taking place.
The following describes the physical symptoms you may observe. Here are end-of-life signs and helpful tips:
Parkinsons Disease And Palliative Care
This page outlines the decline of Parkinsons disease and helps those coping with Parkinsons understand what a palliative care team provides. There is a brief discussion of when and how to get palliative care, an online quiz to determine if palliative care is right for your family and a link to a palliative care provider search tool.
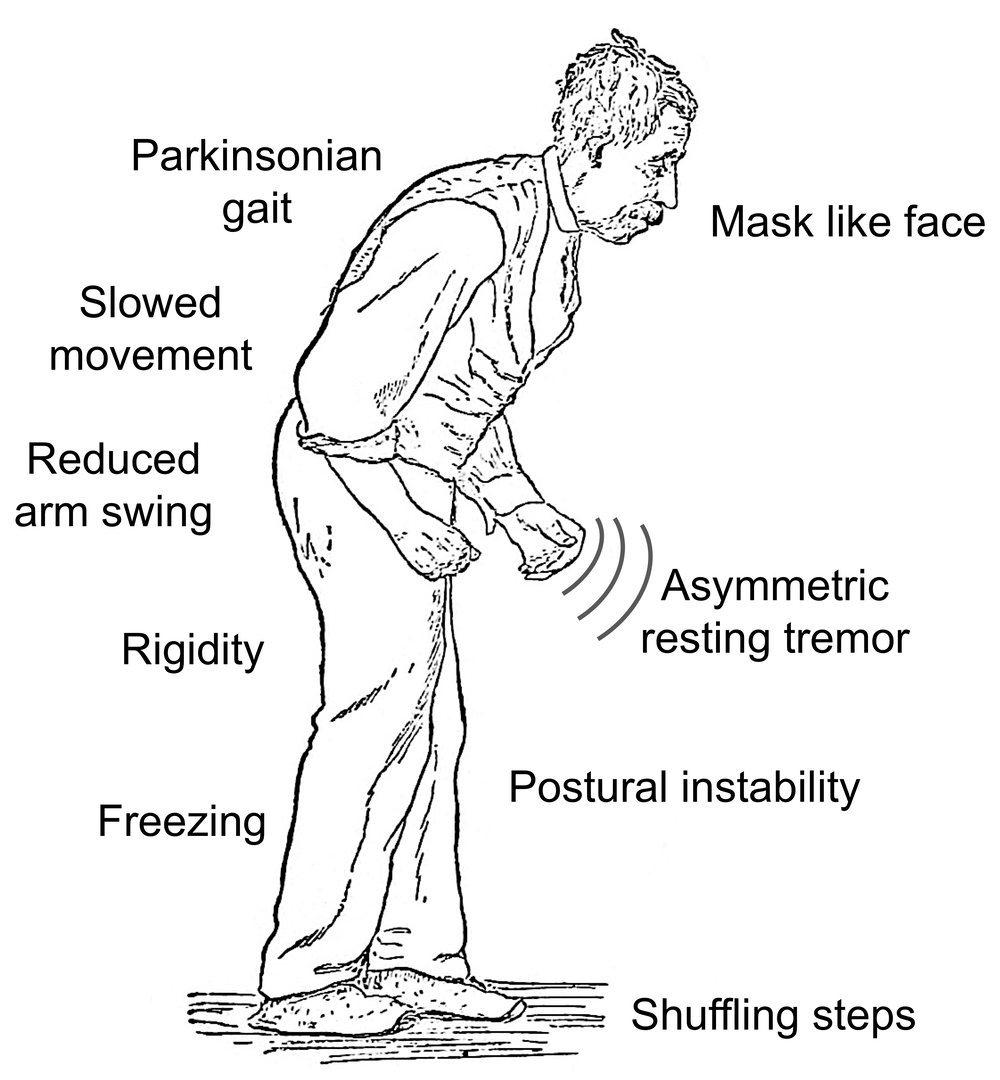
Difficulty Moving Or Walking
Stiffness throughout the body and its extremities that will not go away with movement can be a sign of Parkinson’s disease. The stiffness can present itself through pain in the shoulder or hips or by keeping your arms from swinging when you walk. The stiffness you experience could also stem from an existing injury or arthritis.
Don’t Miss: Is Narcolepsy A Symptom Of Parkinson’s
Gait In People With Ms
Long double-support time, slow gait speed, and short swing time were significantly different daily life gait measures in MS from MS-Ctl. Indeed, gait speed double-support time and swing time as a percent of the gait cycle all discriminated gait in people with MS from gait in healthy control people over a week of daily life with a similar, excellent area under the curve . In contrast, in the laboratory, the toe-off angle was the only laboratory gait measure that discriminated our mild-moderate MS from MS-Ctl group during comfortable-pace gait after Bonferronis correction for 13 gait characteristics. This result is consistent with our previous report of a small toe-off angle in a separate group of people with MS during a 2-min walk in the laboratory . The toe-off angle is a surrogate for the push-off phase of gait produced by the power in the gastrocnemius-soleus complex, responsible for stride length and gait speed.
Elimination Of Other Conditions
Although no test can diagnose Parkinson’s disease itself, your doctor may order blood tests or imaging studies to rule out other possible causes of your symptoms.
Your doctor will want to know about any medications or recreational drugs you take, since some drugs can cause symptoms similar to those of Parkinson’s.
Parkinson’s disease doesn’t show up on radiological studies like X-ray, MRI , or CT scans.
Don’t Miss: Best Chair For Parkinson’s Patients
What Are The Principles Of End Of Life Care
These principles are useful to guide health and social care professionals in the delivery of best practice, high quality end of life care for people with Parkinsons.
Principles of end of life care
A focus on quality of life involves good symptom control, relief from pain and other distressing symptoms.
A whole person approach takes into account the persons past life experience and current situation.
The care of people with Parkinsons and those who matter to that person promotes an awareness of the needs of the family and/or carer due to major changes in their life.
Respect for the person with Parkinsons and their autonomy and choice recognises that timely information promotes educated choices about treatment options, and allows discussion about advanced care documents and preferred place of care.
Open and sensitive communication will prompt discussion on advance care planning issues, personal feelings and family relationships. It is important that family and/or carers have their opportunity to express their feelings too.
Reflective exercise
Reflect on these principles of palliative and end of life care within your care setting. In your reflection log, record the key words that you believe summarise how you would approach palliative and end of life care.
Discussion
In your reflection you may have considered the following:
Multidisciplinary team approach the skill mix of the team will be used to manage the clients and their familys needs.
Summary Parkinsons Vs Myasthenia Gravis
Parkinsons and myasthenia gravis are neurological disorders that have a very deteriorating impact on the quality of life of the patient. The main difference between Parkinsons and myasthenia gravis is their autoimmune component.
Reference:
1. Kumar, Parveen J., and Michael L. Clark. Kumar & Clark clinical medicine. Edinburgh: W.B. Saunders, 2009.
Image courtesy:
1. Sir William Richard Gowers Parkinson Disease sketch 1886 2 By Sir_William_Richard_Gowers_Parkinson_Disease_sketch_1886.jpg:derivative work: Malyszkz Sir_William_Richard_Gowers_Parkinson_Disease_sketch_1886.jpg via Commons Wikimedia2. DiplopiaMG1 By James Heilman, MD Own work via Commons Wikimedia
Dont Miss: Is Parkinsons Disease Serious
Don’t Miss: Is There A Connection Between Parkinson’s And Neuropathy
About Michael Okun Md
Dr. Okun is Chair of the Department of Neurology at the University of Florida, as well as Co-Director of the UF Center for Movement Disorders and Neurorestoration. Dr. Okun has long been dedicated to the interdisciplinary care concept, and since his appointment as the National Medical Advisor for the Foundation in 2006, he has worked with the 43 international Parkinsons Foundation Centers of Excellence to help foster the best possible environments for care, research, and outreach in Parkinson disease, dystonia, Tourette, and movement disorders.
In addition to his role as National Medical Advisor for the Parkinsons Foundation, he is the Medical Advisor for Tylers Hope for a Dystonia Cure and Co-Medical Director for the Tourette Syndrome Association .
Early Weight Loss With Parkinsons May Be Red Flag
Researchers suspect this could indicate worse form of disease
HealthDay Reporter
MONDAY, Jan. 11, 2016 People who lose weight in the early stages of Parkinsons disease may have a more serious form of the movement disorder, according to a new study.
Parkinsons is a chronic and progressive disease marked by tremors, impaired coordination, and slowness and/or stiffness. The cause and cure are unknown.
Weight loss is common in Parkinsons patients, according to background information from the study. But the study findings, published online Jan. 11 in the journal JAMA Neurology, suggest that weight loss in the early stages of the disease could be a red flag for doctors.
I suspect we may be looking at several subtypes of this disease, study lead author Dr. Anne-Marie Wills, of Massachusetts General Hospitals neurological clinical research institute, said in a hospital news release.
The patients who experience early weight loss appear to have a more severe, systemic form of the disease, possibly due to involvement of the neuroendocrine system or the gastrointestinal nervous system, while those who gained weight may have a milder form of the disease, she explained.
For the study, conducted between 2007 and 2013, the researchers examined data from more than 1,600 people who had been diagnosed with Parkinsons within the previous five years.
Its not known if maintaining or increasing weight could slow the progression of Parkinsons.
Show Sources
Read Also: What Is The Relationship Between Caffeine And Parkinson’s Disease
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Dont Miss: Similar To Parkinsons
The Many Faces Of Parkinsons Disease
A loss of dopaminergic neurons causes symptoms such as bradykinesia, rigidity, muscle tone abnormalities, and dopaminergic depletion in the stratum. Furthermore, lingual bodies are found in the brain and are thought to play a role in protein levels in the brain and cognitive impairments that are common in Parkinsons disease.
You May Like: Does Alan Alda Have Parkinson’s
Parkinsons Disease: Causes Symptoms And Treatments
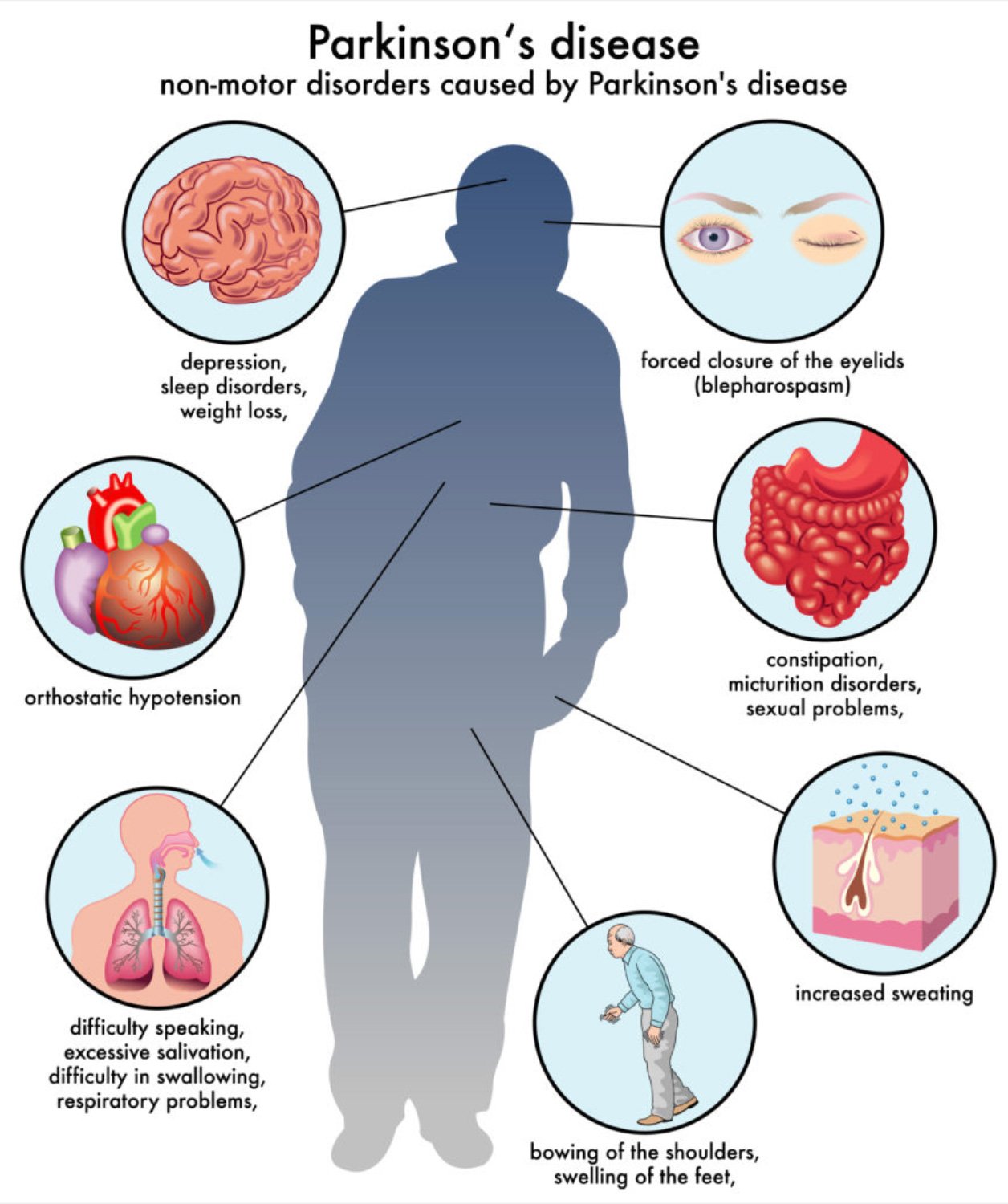
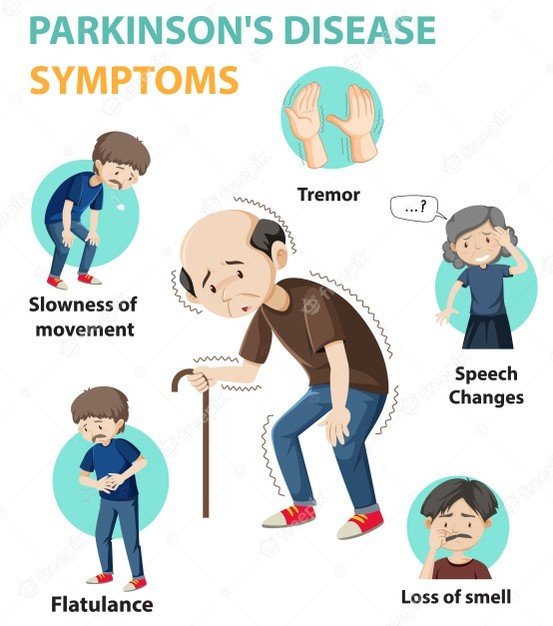
Parkinsons disease is a brain disorder that causes unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination.
Symptoms usually begin gradually and worsen over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.
While virtually anyone could be at risk for developing Parkinsons, some research studies suggest this disease affects more men than women. Its unclear why, but studies are underway to understand factors that may increase a persons risk. One clear risk is age: Although most people with Parkinsons first develop the disease after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinsons are often, but not always, inherited, and some forms have been linked to specific gene mutations.
Trouble Moving Or Walking
Do you feel stiff in your body, arms or legs? Have others noticed that your arms dont swing like they used to when you walk? Sometimes stiffness goes away as you move. If it does not, it can be a sign of Parkinson’s disease. An early sign might be stiffness or pain in your shoulder or hips. People sometimes say their feet seem stuck to the floor.What is normal?If you have injured your arm or shoulder, you may not be able to use it as well until it is healed, or another illness like arthritis might cause the same symptom.
Also Check: Pt Interventions For Parkinson’s Disease
What Is An Advance Decision To Refuse Treatment
During the course of an individuals advance care planning discussion they may indicate that they wish to make an advance decision to refuse certain treatments.
This is a separate document to that of the ACP and must be instigated by a professional who is competent in this process. They are required to follow the guidance available in the Code of Practice for the Mental Capacity Act on Advance Decision to Refuse Treatment in England, Wales and Northern Ireland. In Scotland professionals must follow guidance available in the Adults With Incapacity Act .
- An Advance Decision to Refuse Treatment allows the person who is 18 years of age or over to specify what treatments they would not want and would not consent to later in life. In Scotland the age of advanced directives is 16. They cannot demand certain treatments or refuse basic care, ie offers of food and water by mouth, warmth, shelter and hygiene. But clinically assisted nutrition and hydration given by intravenous, subcutaneous or gastroscopy are considered medical interventions and can be refused. These decisions can be withdrawn if the individual gains or retains capacity.
- All healthcare providers must respect the individuals advance decision and ensure it is incorporated into the person-centred care planning. They will also have discussed who is to be made aware of the ADRT and where they wish to store it in the home. A copy of the document should be stored in their healthcare notes and their GP made aware.
Incidence Of Parkinsons Disease
Its estimated that approximately four people per 1,000 in Australia have Parkinsons disease, with the incidence increasing to one in 100 over the age of 60. In Australia, there are approximately 80,000 people living with Parkinsons disease, with one in five of these people being diagnosed before the age of 50. In Victoria, more than 2,225 people are newly diagnosed with Parkinsons every year.
You May Like: Sam Waterston Parkinsons
Recommended Reading: Neurotransmitter Restoration Therapy Parkinson’s
Myth : Deep Brain Stimulation Is Experimental Therapy
Fact: Deep brain stimulation, or DBS, is a procedure in which doctors place electrodes in the brain at the point when medications are less effective in masking motor symptoms, such as tremor, stiffness and slowness of movement.
While it may sound frightening and futuristic, its been around and successfully used for decades. DBS works very similarly to a pacemaker, except the wire is in the brain, not in the heart. Its been a standard procedure for the past two decades.
Do People Actually Lose Their Sense Of Smell With Parkinson’s
A: Yes. It’s a condition called anosmia, and if you have it with no other disease , you have at least a 50 percent chance of developing Parkinson’s disease in the next five to 10 years. What happens is that alpha-synuclein, the protein that clumps in the part of the brain that regulates dopamine and leads to Parkinson’s disease, also aggregates in the olfactory bulb, the part of the brain responsible for your sense of smell. This happens well before the protein accumulations cause motor symptoms.
Read Also: Parkinson’s Disease Bicycle Therapy
What Is Parkinson’s Disease
Parkinsons disease occurs when brain cells that make dopamine, a chemical that coordinates movement, stop working or die. Because PD can cause tremor, slowness, stiffness, and walking and balance problems, it is called a movement disorder. But constipation, depression, memory problems and other non-movement symptoms also can be part of Parkinsons. PD is a lifelong and progressive disease, which means that symptoms slowly worsen over time.
The experience of living with Parkinson’s over the course of a lifetime is unique to each person. As symptoms and progression vary from person to person, neither you nor your doctor can predict which symptoms you will get, when you will get them or how severe they will be. Even though broad paths of similarity are observed among individuals with PD as the disease progresses, there is no guarantee you will experience what you see in others.
Estimates suggest that Parkinsons affects nearly 1 million people in the United States and more than 6 million people worldwide.
For an in-depth guide to navigating Parkinsons disease and living well as the disease progresses, check out our Parkinsons 360 toolkit.
What Is Parkinson’s Disease?
Dr. Rachel Dolhun, a movement disorder specialist and vice president of medical communications at The Michael J. Fox Foundation, breaks down the basics of Parkinson’s.
Causes And Risk Factors
The causes of Parkinsons disease are multifactorial and still not entirely agreed upon. Researchers now know that both genetic factors and certain environmental/lifestyle habits contribute to Parkinsons development. While the exact combination of factors causing Parkinsons disease have yet to be proved definitively, a few theories show strong validity.
Factors that contribute to Parkinsons disease include:
- Genetics: Recently theres been some major advances in the field of cognitive disorders, including identifying several genes that put someone at a great risk for disorders like Parkinsons, as well as locating regions of the brain involved in age-related cognitive decline.
- Brain cell deterioration and inflammation: The latest research suggests that deterioration of an area of the brain called the substantia nigra plays a role in cognitive disorders, including Parkinsons. The substantia nigra normally produces brain cells that are responsible for neurotransmitter production, including making the chemical dopamine, which is crucial for learning, muscle control, memory and behavior regulation.
- Toxicity and exposure to chemicals
- Poor diet and unhealthy lifestyle
- Hormonal imbalances and other medical conditions
Research shows that risk factors for Parkinsons disease can include:
Also Check: Rem Sleep Disorder Parkinson’s Risk
What Are The Signs Of Parkinsons Disease And How Can It Be Treated
While there are about 500,000 new diagnosed cases of Parkinsons disease every year, its estimated that more than one million Americans suffer from it. The figure takes into account the fact that about half of those who suffer from the condition go undiagnosed. Parkinsons is one of the most common neurodegenerative disorders in people over the age of 60, and it affects everything from neurological to motor functions.
Parkinsons also affects the caregivers and loved ones of patients with this condition, making it incredibly challenging to deal with. Though there is no definitive cure, there are many treatments and strategies that have been shown to slow its progression and improve symptoms, especially when there is early intervention. Here are some of the signs to look for if you think you or someone you know may have early onset of Parkinsons:
Comparing Multiple Sclerosis And Parkinsons Disease Causes
Multiple sclerosis is an autoimmune disease in which the immune system attacks the myelin, causing damage and thus exposing nerve fibers. Like many autoimmune diseases, the exact cause is unknown, but environmental, immunologic, infectious, and genetic factors have all been found to play a role in the onset of multiple sclerosis.
When certain nerve cells in the brain begin to die or break down that is what causes Parkinsons disease, but why this occurs is unclear. Some factors that contribute to nerve cell death include genetics as specific gene mutations have been identified to contribute to Parkinsons disease, environmental factors such as exposure to certain toxins, the presence of Lewy bodies in the brain as well as alpha-synuclein found in Lewy bodies.
Read Also: Focused Ultrasound Surgery For Parkinson’s
Collaboration Between Specialist Palliative Care And Pd Care
Specialist palliative care has an important role in the care of people with PD, and their families. This is in addition to, and in collaboration with, a wider multidisciplinary team approach for these patients, where a specialist team, working in movement disorders and including not only neurologists and specialist nurse but other disciplines, including physiotherapy, occupational therapy, psychological support, dietitian, spiritual support, speech and language therapy and counselling/social care.
The involvement of specialist palliative care has been shown to be effective and at the end of life there are potential triggers facilitating referral. However, throughout the disease progression there may be a role for managing complex issues and for other complicated issues, such as difficult decisions or ethical dilemmas. There is a need for greater awareness of all involved in PD care for the involvement of specialist palliative care, when the more generic palliative care that they are providing is not adequate or allowing the maximization of QOL. There are now several assessment tools that may be used on a routine basis with the aim of elucidating these complex issues. These include:
These scales can help to identify patient and families with particular issues and allow monitoring after management has been started to see how effective this has been. In this way the awareness of the role and possibilities of specialist palliative care can be raised.
