Multiple System Atrophy Formerly Called Shy
As predicted by the name of this parkinsonism, multiple system atrophy affects multiple systems of the body. It affects both the motor skills movement system and the involuntary system of the body. Though the symptoms can often be treated with medications, there is no cure. In addition, there are no drugs that are able to slow the progress of MSA.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
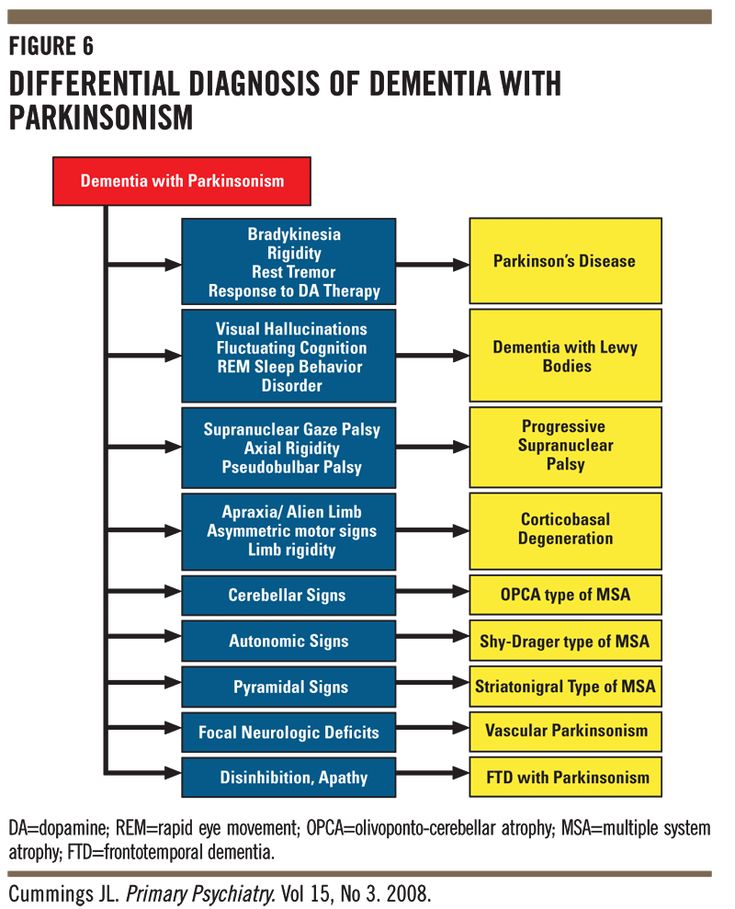
Whats The Difference Between Progressive Supranuclear Palsy And Parkinsons
People with PSP generally progress more rapidly than people with Parkinsons. A person with Parkinsons tends to lean forward while a person with PSP tends to lean backward. Tremors are common in people with Parkinsons and rare in people with PSP. Speech and swallowing abnormalities are more severe and show up sooner in those living with PSP.
For more information on progressive supranuclear palsy, read this fact sheet and insights from the CurePSP organization website.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
How Is Parkinsonism Diagnosed
You should be referred to a Parkinsons specialist for the diagnosis of any parkinsonism. They may wish to explore different things before giving you a diagnosis.
Your specialist will look at your medical history, ask you about your symptoms and do a medical examination.
Telling the difference between types of parkinsonism isnt always easy, for the following reasons:
- The first symptoms of the different forms of parkinsonism are so similar.
- In many cases, parkinsonism develops gradually. Symptoms that allow your doctor to make a specific diagnosis may only appear as your condition progresses.
- Everyone with parkinsonism is different and has different symptoms.
Find out more: see our information on symptoms of Parkinsons, and diagnosing Parkinsons.
One of the most useful tests to find out what sort of parkinsonism you may have is to see how you respond to treatment.
If your specialist thinks you have idiopathic Parkinsons, theyll expect you to have a good response to Parkinsons drugs such as levodopa . A good response means that your symptoms will improve. Sometimes, it will only be clear that youve responded to medication when the drug is reduced or stopped, and your symptoms become more obvious again.
If you dont have any response to Parkinsons medication, your specialist will have to look again at your diagnosis.
Although not routinely available, your specialist may wish to carry out some of the tests below.
Current tests available include:
You May Like: Familial Parkinson’s
Clinical Confirmation Of Parkinson Disease
The diagnosis of PD is guided by the Queen Square Brain Bank diagnostic criteria, which require two steps. Step one focuses on the definition of parkinsonism and requires the presence of bradykinesia and of either typical rest tremor, extrapyramidal rigidity, or postural instability . However, postural instability is not an early PD feature and should alert the clinician of an atypical parkinsonian disorder. Step two focuses on features typical of the parkinsonism of PD, such as unilateral onset, excellent response to levodopa therapy, and development of dyskinesia. Exclusion criteria include pyramidal signs, stepwise deterioration of parkinsonism , repeated head injury, history of encephalitis or oculogyric crisis, neuroleptic treatment at the onset of symptoms, strictly unilateral features after 3 years, supranuclear gaze palsy, cerebellar signs, early severe autonomic dysfunction, early severe cognitive dysfunction, negative response to levodopa, and imaging evidence of communicating hydrocephalus.
Whats The Difference Between Vascular Parkinsonism And Parkinsons
As the name implies, vascular parkinsonism is caused by cerebrovascular disease which affects the blood supply to the brain. Vascular parkinsonism is caused by one or more small strokes, while Parkinsons is caused by a gradual loss of nerve cells. One major difference from Parkinsons is that its not progressive, while Parkinsons becomes worse with time. Another difference is that there are no tremors in vascular parkinsonism.
For more information on vascular parkinsonism, read this journal article.
Read Also: What Are The Four Cardinal Signs Of Parkinson’s Disease
Dementia With Lewy Bodies
- Dementia with Lewy bodies is a progressive, neurodegenerative disorder in which abnormal deposits of a protein called alpha-synuclein build up in multiple areas of the brain.
- Dementia with Lewy bodies is second to Alzheimers as the most common cause of degenerative dementia that first causes progressive problems with memory and fluctuations in thinking, as well as hallucinations. These symptoms are joined later in the course of the disease by parkinsonism with slowness, stiffness and other symptoms similar to PD.
- While the same abnormal protein is found in the brains of those with PD, when individuals with PD develop memory and thinking problems it tends to occur later in the course of the disease.
- There are no specific treatments for DLB. Treatment focuses on symptoms.
From Subtypes To Better Treatments
With the identification of different subtypes of Parkinsons progressing, researchers at UCL wanted to find out if they could use donated tissue from the Parkinsons UK Brian Bank to retrospectively subtype Parkinsons. They wanted to look at the early symptoms of Parkinson’s to see if it could predict how Parkinsons would progress.
The team analysed the medical records from 111 patients whose brains arrived at the Brain Bank between 2009 and 2017. They discovered that separating people into three subtypes could predict how the condition progressed.
The subtypes they used were:
Talking about the study to Neurology Today, Thomas T. Warner, MD, PhD, director of the Reta Lila Weston Institute at UCL Institute of Neurology, said:
This analysis suggests that we may be able to use this type of classification to help guide treatment, as well as help patients better understand their disease course.
Recommended Reading: Can Parkinson’s Run In The Family
Further Support From A Us Based Study
In 2019, data from 446 newly diagnosed people with Parkinsons participating in the Parkinsons Progression Markers Initiative was published.
The study identified 3 subtypes of Parkinsons with some similarities to the previous example.
Subtype I: Mild baseline, moderate motor progression 43.1% of the participants. Characterised by moderate progression of motor symptoms but less likely to experience memory and thinking problems.
Subtype II: Moderate baseline, mild progression 22.9% of the participants. Characterised by slow progression of motor and non-motor symptoms.
Subtype III: Severe baseline, rapid progression 33.9% of the participants. Characterised by rapid progression of both motor and non-motor symptoms.
Adapted from Data-Driven Subtyping of Parkinsons Disease Using Longitudinal Clinical Records: A Cohort Study
The main conclusion from this paper was that the progression rates in this study did not necessarily associate with how severe a persons symptoms were on entering the study. They also suggested that the progression rate of non-motor symptoms is not necessarily correlated with the progression rate of motor symptoms.
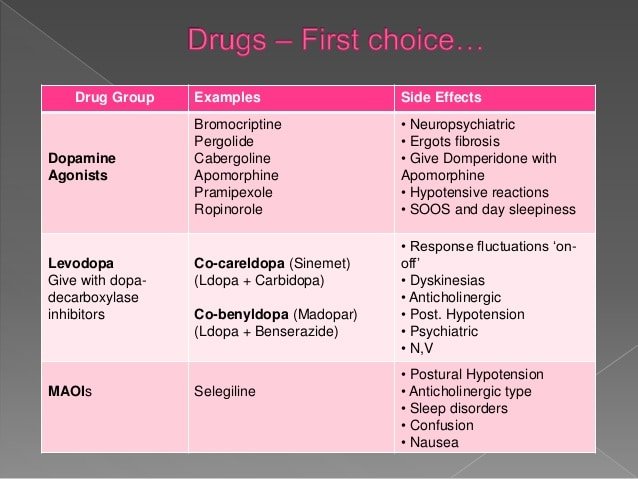
Medicines For Parkinson’s Disease
Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapysuch as nausea, vomiting, low blood pressure, and restlessnessand reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinsons symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Recommended Reading: Does Sam Waterston Have Parkinson
Whats The Difference Between Multiple System Atrophy And Parkinsons
Parkinsons and MSA both affect the movement control system and the involuntary autonomic control system and early symptoms can make a differential diagnosis a challenge. MSA, however, tends to progress faster than Parkinsons balance problems and a stooped posture happen earlier and get worse more quickly with MSA and autonomic functions such as blood pressure, heart rate, breathing, sweating, bladder function, and sexual problems are more severe in people with MSA.
For more information on multiple symptom atrophy, read this fact sheet.
Italian Researchers Also Find Subtypes Are Linked To Progression
In the same year, another smaller study was published that identified three main subtypes of Parkinsons based on the main motor symptom that people experienced.
Subtype I: Predominant tremor.
Subtype II: Mixed motor symptoms, with no prevailing motor features.
Subtype II: Stiffness or inflexibility of the muscles, or balance or walking difficulties as their main symptoms.
Adapted from Psychiatric profile of motor subtypes of de novo drugnaïve Parkinsons disease patients
The team also linked the subtypes with different progression rates, with those in subtype III usually showing a faster progression and were more likely to develop memory problems and dementia. While those in subtype I, the progression was slower and people were less likely to develop memory problems, visual hallucinations, and depression.
Don’t Miss: Parkinson’s Disease Survival Rate
More Data = More Success
With researchers seeing the potential of these subtypes to change the way to treat and manage Parkinsons, it is clear why this is a growing area of research. But, we do not yet have a definitive set of subtypes for Parkinsons. One of the reasons for this, is the complexity of the condition and the way it fluctuates hour to hour, and day to day.
Even back in 2015, it was clear that simply collecting detailed information when people visited the clinic wasnt going to be good enough to truly understand Parkinsons.
Parkinsons is a fluctuating condition, so how can I really know how it affects the individual throughout the day and between visits? And how can I really know how if the treatment I prescribe is right for that individual?
Were going to be asking some participants in the Discovery study to take one of our mobile phones home with them and complete the tests at different times over the course of a week. This will give us vital information about how their Parkinsons affects them from day-to-day which weve never really had access to before.
Dr Michele Hu, University of Oxford
Over the last few years, researchers have attempted to come up with a classification system for Parkinsons based on the types and severity of motor symptoms and the presence of other non-motor symptoms at diagnosis. There are now a handful of classification systems that have been proposed but few neurologists rely on them in discussions about what their patients may expect.
Tracking Parkinsons Joins Forces With The Oxford Parkinsons Disease Centre
In 2018, Tracking Parkinsons was the largest, in-depth study of the condition ever attempted, a title it still holds to this date. The project had been running for 5 years and had data from 2,600 participants across 70 hospitals in the UK.
Using sophisticated data analysis on the types of motor and non-motor symptoms people had when joining the research studies, the teams identified 4 possible subtypes of Parkinsons:
Subtype I:Prominent tremor on one side, an average level of non-motor symptoms and responding poorly to levodopa.
Subtype II: Mild motor and non-motor symptoms.
Subtype III: Severe movement symptoms, poor psychological well-being and poor sleep.
Subtype IIII: Symmetrical motor symptoms , poor sense of smell, low blood pressure, memory problems and responding poorly to levodopa .
Adapted from Developing and validating Parkinsons disease subtypes and their motor and cognitive progression
And for the first time, researchers linked these subtypes to progression rates. Those in the last subtype were likely to experience the fastest progression of their symptoms, while the middle two progressed at an average rate, and those in the first seemed to have the slowest progressing form of the condition.
Read Also: How Does Parkinson\’s Disease Affect The Mind
Living With Parkinsons Disease
Depending on severity, life can look very different for a person coping with Parkinsons Disease. As a loved one, your top priority will be their comfort, peace of mind and safety. Dr. Shprecher offered some advice, regardless of the diseases progression. Besides movement issues Parkinsons Disease can cause a wide variety of symptoms including drooling, constipation, low blood pressure when standing up, voice problems, depression, anxiety, sleep problems, hallucinations and dementia. Therefore, regular visits with a neurologist experienced with Parkinsons are important to make sure the diagnosis is on target, and the symptoms are monitored and addressed. Because changes in your other medications can affect your Parkinsons symptoms, you should remind each member of your healthcare team to send a copy of your clinic note after every appointment.
Dr. Shprecher also added that maintaining a healthy diet and getting regular exercise can help improve quality of life. Physical and speech therapists are welcome additions to any caregiving team.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
The Nervous System & Dopamine
To understand Parkinson’s, it is helpful to understand how neurons work and how PD affects the brain .
Nerve cells, or neurons, are responsible for sending and receiving nerve impulses or messages between the body and the brain. Try to picture electrical wiring in your home. An electrical circuit is made up of numerous wires connected in such a way that when a light switch is turned on, a light bulb will beam. Similarly, a neuron that is excited will transmit its energy to neurons that are next to it.
Neurons have a cell body with branching arms, called dendrites, which act like antennae and pick up messages. Axons carry messages away from the cell body. Impulses travel from neuron to neuron, from the axon of one cell to the dendrites of another, by crossing over a tiny gap between the two nerve cells called a synapse. Chemical messengers called neurotransmitters allow the electrical impulse to cross the gap.
Neurons talk to each other in the following manner :
Don’t Miss: Parkinson’s Stages Life Expectancy
