How To Talk To A Loved One About Parkinsons Disease
These are some strategies that can be helpful while talking to a loved one about Parkinsons disease:
- Check in regularly: Check in on the person regularly to ask them how theyre feeling and coping.
- Use empathetic language: Parkinsons disease can affect a persons ability to go about their daily life. The person might find it challenging to do things they once did easily. This can be difficult and frustrating for them. Try to be empathetic when you speak to them, so they feel supported.
- Offer assistance: As Parkinsons disease progresses, the person may not be able to drive, cook, clean, or care for themselves. Offer them your assistance and let them know they can count on you.
- Encourage them to settle their affairs: If your loved one is in a position to make important decisions, it can be helpful to encourage them to settle their affairs.
How Is Parkinson’s Disease Treated
Parkinsons disease cannot be cured, but it can be managed by movement disorder specialists at The NeuroMedical Center. Your treatment plan may include medications and regular physical and occupational therapy sessions. Your neurologist may also recommend surgery to help better control your Parkinsons symptoms.
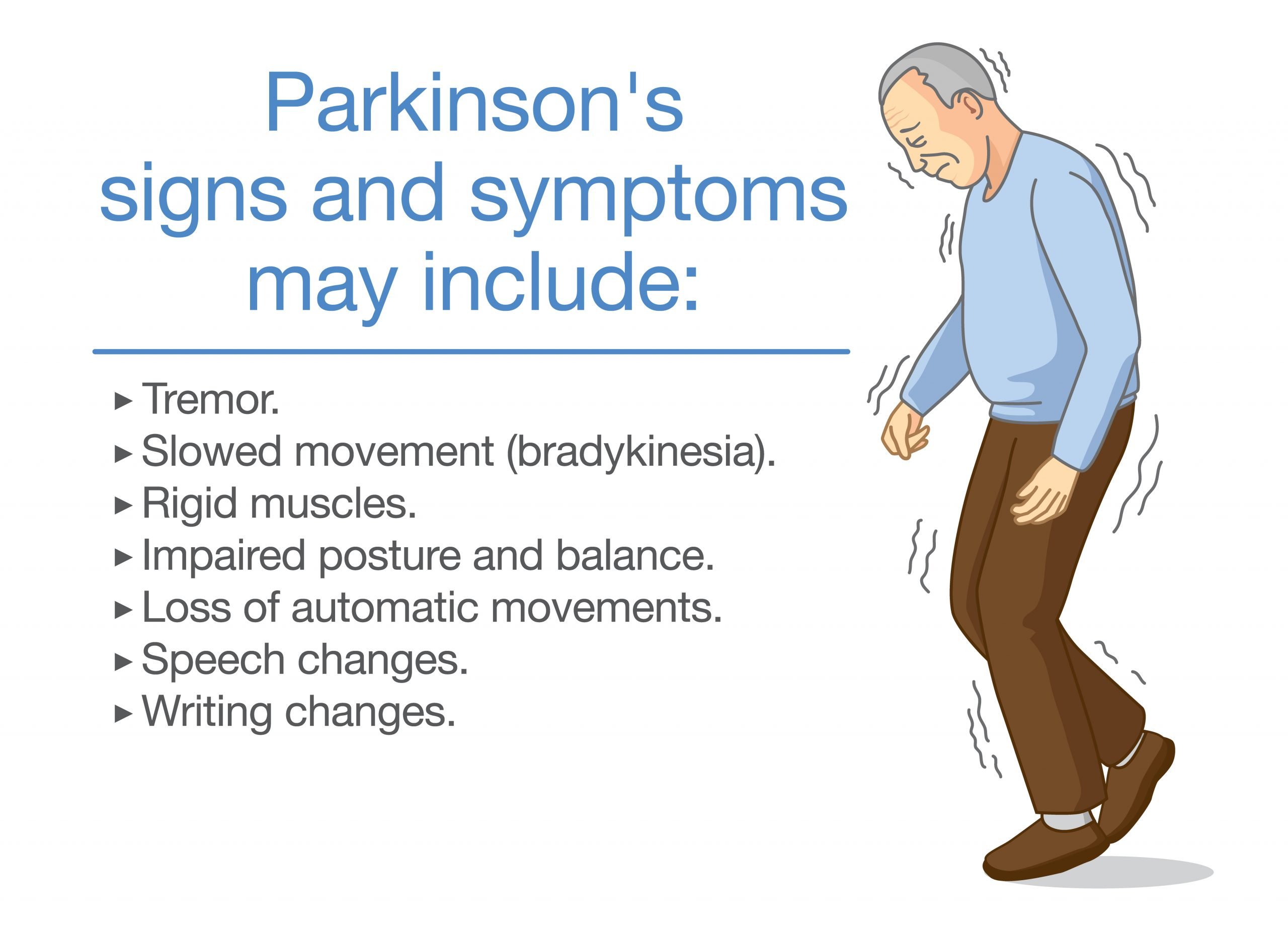
What Are Common Parkinson’s Symptoms
Parkinsons disease tends to start with subtle symptoms which get worse over time. It may begin with a slight tremor, usually in one hand or arm. Eventually it begins to affect both sides of your body. It can cause trembling, stiffness, and slow movements. It can cause loss of balance and coordination. You may develop a stooped posture. You may speak softly and in a monotone, and you may pause frequently when you speak. These symptoms vary from person to person, and they may progress slowly or quickly.
Don’t Miss: How To Treat Parkinson’s Disease
Living With Parkinsons Disease
Parkinsons disease progresses over time, often taking years before symptoms appear. Because it develops gradually, most people have many years of productive living after being diagnosed.
The following are some tips from the National Parkinson Foundation for walking, standing and other day-to-day activities:
Expert Care For Parkinsons Disease In Louisiana
If you are living with Parkinsons disease, it is recommended that you receive treatment from a neurologist who has specialized training in movement disorders. The NeuroMedical Center offers three movement disorder specialists who are highly experienced diagnosing and treating Parkinsons. Dr. Gerald J. Calegan, Dr. B. Glenn Kidder, and Dr. Rebecca E. Whiddon remain on the cutting-edge of knowledge and treatment of Parkinsons and other movement disorders. Our neurologists and DBS neurosurgeon, Dr. Paul J. Waguespack, have performed over 400 successful DBS surgeries to date. With access to advanced diagnostic services, our Parkinsons specialists are best equipped to tailor a plan of care for your specific needs.
Also Check: Is Finger Twitching A Sign Of Parkinson’s
How Is Parkinsons Disease Diagnosed
There is no test that can prove that you have PD. The diagnosis is based on you having the typical symptoms . In the early stage of the disease, when symptoms are mild, it may be difficult for a doctor to say if you definitely have PD. As the symptoms gradually become worse, the diagnosis often becomes more clear.
PD is sometimes confused with other conditions. Some conditions can give Parkinsonism features that is, symptoms similar to PD but caused by other conditions. For example, some medicines used to treat other conditions can cause side-effects which resemble symptoms of PD. Some rare brain disorders can also cause similar symptoms.
Therefore, it is normal practice in the UK to be referred to a specialist if PD is suspected. The specialist will be used to diagnosing PD and ruling out other causes of the symptoms. They will usually be either a neurologist or a doctor specialising in elderly care. If there is still doubt about the diagnosis, sometimes a scan of the brain is carried out. This helps to differentiate PD from some other conditions that can cause Parkinsonism features. Other tests sometimes needed include blood tests and tests of your sense of smell.
Read Also: Zhichan Capsule
Patient Education For Parkinson’s Drugs
Providing patients with disease and treatment related information is an important role that we can play as physical therapists in helping to improve their quality of life. While levodopa has remained the most effective treatment for improving motor function in Parkinsons patients, it comes with several dangerous side effects, as mentioned previously. The biggest problem of levodopa, however, seems to be its weakened efficacy after prolonged use, typically 3-4 years. For a patient who has experienced significant gain in their symptoms, this can be extremely devastating. With knowledge of this as a physical therapist, we can recommend them discussing with their physician on initial use of an alternative drug, specifically Monoamine Oxidase B Inhibitors. Another important piece of education to our patients is on orthostatic hypotension. Patients should avoid sudden postural changes and getting up too fast. For patients getting out of bed, it would be advisable to sit on the side of the bed for about 30 seconds before standing and then standing for 30 more seconds before walking in order to prevent falls.
References:
Recommended Reading: How Do I Know If I Have Parkinson’s Disease
Education And Training Needs Assessment
This first version was revised according to the findings of the literature review which are presented herewith and are summarised in Table .
Table 1 Summary of educational and training needs identified with the narrative literature review
The shared needs of patients and their caregivers include the availability of simple, yet comprehensive tools for future planning. Essentially, they need practical guidance to navigate the PD journey . They emphasize the personalization of the provided information and support . They are also in need of comparative information on the advantages of palliative care quality when provided as inpatient care, within palliative units in nursing homes or at home and which preferences should guide decisions for the place of death . Patients indicated that improved education, shared decision making, and communication of Advanced Care Planning in order to be able to discuss advanced directives. Further education and emotional support, particularly regarding disease progression and their expectations, as well as advanced PD management was also stressed as an important aspect.
The second version of the toolkit that was informed by the literature review was further assessed during consensus meetings with experts that led to the definition of the third version which was assessed with an online survey from independent, external experts.
What Genes Are Linked To Parkinsons Disease
Several genes have been definitively linked to PD:
- SNCA. This gene, which makes the protein alpha-synuclein, was the first gene identified to be associated with Parkinsons. Research findings by the National Institutes of Health and other institutions prompted studies of the role of alpha-synuclein in PD, which led to the discovery that Lewy bodies seen in all cases of PD contain clumps of alpha-synuclein. This discovery revealed the link between hereditary and sporadic forms of the disease.
- LRRK2. Mutations in LRRK2 were originally identified in several English and Basque families as a cause of a late-onset PD. Subsequent studies have identified mutations of this gene in other families with PD as well as in a small percentage of people with apparently sporadic PD. LRRK2 mutations are a major cause of PD in North Africa and the Middle East.
- DJ-1. This gene normally helps regulate gene activity and protect cells from oxidative stress and can cause rare, early forms of PD.
- PRKN . The parkin gene is translated into a protein that normally helps cells break down and recycle proteins.
- PINK1. PINK1 codes for a protein active in mitochondria. Mutations in this gene appear to increase susceptibility to cellular stress. PINK1 has been linked to early forms of PD.
- GBA . Mutations in GBA cause Gaucher disease , but different changes in this gene are associated with an increased risk for Parkinsons disease as well.
Read Also: What Foods Should Be Avoided When Taking Levodopa
Don’t Miss: How Long Does It Take Parkinson’s To Progress
What Diseases And Conditions Resemble Parkinsons Disease
PD is the most common form of parkinsonism, in which disorders of other causes produce features and symptoms that closely resemble Parkinsons disease. Many disorders can cause symptoms similar to those of PD, including:
Several diseases, including MSA, CBD, and PSP, are sometimes referred to as Parkinsons-plus diseases because they have the symptoms of PD plus additional features.
In very rare cases, parkinsonian symptoms may appear in people before the age of 20. This condition is called juvenile parkinsonism. It often begins with dystonia and bradykinesia, and the symptoms often improve with levodopa medication.
What Are Common Parkinsons Symptoms
Parkinsons disease tends to start with subtle symptoms which get worse over time. It may begin with a slight tremor, usually in one hand or arm. Eventually it begins to affect both sides of your body. It can cause trembling, stiffness, and slow movements. It can cause loss of balance and coordination. You may develop a stooped posture. You may speak softly and in a monotone, and you may pause frequently when you speak. These symptoms vary from person to person, and they may progress slowly or quickly.
Don’t Miss: Is Coffee Bad For Parkinson’s Disease
Eating Drinking And Parkinsons Disease
- Dont rush your meals. Allow the extra time you need to finish your meal. Rest your elbows on the table to provide more motion at your wrist and hand.
- Sit with your knees and hips bent at a 90-degree angle in a straight-back chair.
- Use utensils with built-up, lightweight handles, or use a spork a spoon and fork in one. Use a rocker knife for cutting food.
- Use a non-skid mat to stabilize objects on the table.
- Use a plate guard or plate with a raised lip to prevent food from spilling.
- Use a long straw with a non-spill cup or use a plastic mug with a large handle.
You May Like: Pfnca Wellness Programs
Motor Circuit In Parkinson Disease
The basal ganglia motor circuit modulates the cortical output necessary for normal movement .
Signals from the cerebral cortex are processed through the basal ganglia-thalamocortical motor circuit and return to the same area via a feedback pathway. Output from the motor circuit is directed through the internal segment of the globus pallidus and the substantia nigra pars reticulata . This inhibitory output is directed to the thalamocortical pathway and suppresses movement.
Two pathways exist within the basal ganglia circuit, the direct and indirect pathways, as follows:
-
In the direct pathway, outflow from the striatum directly inhibits the GPi and SNr striatal neurons containing D1 receptors constitute the direct pathway and project to the GPi/SNr
-
The indirect pathway contains inhibitory connections between the striatum and the external segment of the globus pallidus and between the GPe and the subthalamic nucleus striatal neurons with D2 receptors are part of the indirect pathway and project to the GPe
The STN exerts an excitatory influence on the GPi and SNr. The GPi/SNr sends inhibitory output to the ventral lateral nucleus of the thalamus. Dopamine is released from nigrostriatal neurons to activate the direct pathway and inhibit the indirect pathway. In Parkinson disease, decreased striatal dopamine causes increased inhibitory output from the GPi/SNr via both the direct and indirect pathways .
Also Check: Will Parkinson’s Cause Weight Loss
Parkinsons Disease: Resources For Patients And Families
Parkinsons disease affects every patient differently. This information can help you gain a better understanding of how the disease may affect you and your caregivers.
Resources include:
- A handbook on Parkinsons disease
- Links to national Parkinsons organizations
- Exercise resources
Dont Miss: Fitflop Shoes For Parkinsons
What Is The Prognosis
The average life expectancy of a person with PD is generally the same as for people who do not have the disease. Fortunately, there are many treatment options available for people with PD. However, in the late stages, PD may no longer respond to medications and can become associated with serious complications such as choking, pneumonia, and falls.
PD is a slowly progressive disorder. It is not possible to predict what course the disease will take for an individual person.
One commonly used scale neurologists use for describing how the symptoms of PD have progressed in a patient is the Hoehn and Yahr scale.
Read Also: What Areas Of The Brain Are Affected By Parkinson’s Disease
Resources For Patients With Parkinson’s Disease
In addition to emphasizing counseling and education at each outpatient visit, the Parkinson’s Disease and Movement Disorders Center provides a wealth of education, support and resources to our patients, their families and caregivers, as well as the community.
Sign up for our monthly e-newsletter to stay up to date on our programs, and check out our upcoming events.
Come hear from experts on a variety of topics relating to the symptoms, treatments or breakthroughs associated with Parkinson’s Disease. Attending a speaker series event is free however, space is limited.
The 24th Annual Parkinson’s Disease Patient and Carepartner Symposium will be live-streamed and virtual. The theme for the 2022 Symposium is Familiar Problems, Fresh Approaches: Further Thoughts and Strategies for Managing Parkinson’s. To register and learn more about the event, please select the Event Details button below. Recordings from the 2021 Symposium, as well as prior years, are available on YouTube at the link below.
Some research suggests that many patients with movement disorders benefit greatly from practicing what is so difficult for them movement. Over the past five years, we have developed specialized classes with instructors trained in the needs of PD to bring high-level exercise programs to both patients and their partners.
- Women’s Coffee and Conversation
Tips For Yourself As A Caregiver
While caring for someone with Parkinsons disease, its also important to care for yourself. These are some tips that can be helpful:
- Allow yourself time to process your emotions: Your loved one may not be the only person struggling to accept their diagnosis and prognosis. You may feel like youre in an alternate reality, where your whole world has turned upside down. Take the time you need to process your emotions so that you can stabilize yourself and be a source of support for them.
- Set realistic goals:Caregiving can be stressful and take a lot of work. It can be helpful to set realistic goals for yourself and determine your limits.
- Forgive imperfections: There may be times when youre unable to do everything you planned to or as well as you hoped to. Be kind to yourself accept that youre human and everything may not always be perfect.
- Explore community resources: It can be helpful to locate medical services, support groups, and other community services for your loved one as well as yourself in advance before you need them.
Also Check: How Is Parkinson’s Inherited
Expert Care For Parkinson’s Disease In Louisiana
If you are living with Parkinsons disease, it is recommended that you receive treatment from a neurologist who has specialized training in movement disorders. The NeuroMedical Center offers three movement disorder specialists who are highly experienced diagnosing and treating Parkinsons. Dr. Gerald J. Calegan, Dr. B. Glenn Kidder, and Dr. Rebecca E. Whiddon remain on the cutting-edge of knowledge and treatment of Parkinsons and other movement disorders. Our neurologists and DBS neurosurgeon, Dr. Paul J. Waguespack, have performed over 400 successful DBS surgeries to date. With access to advanced diagnostic services, our Parkinsons specialists are best equipped to tailor a plan of care for your specific needs.
Some Other General Points
Stay as active as possible. Exercise regularly as much as you are able. This may not be possible when the condition is more advanced. However, it is something to consider when symptoms are not too bad. You may walk more slowly than before but a daily walk is good exercise and may help to loosen up stiff muscles. Well-meaning relatives or friends may tell you to rest and take things easy. However, as much as possible and for as long as possible, resist the temptation for others to do things for you just because it may be quicker.
Constipation is common in people with PD. Help to reduce the chance of this by having lots to drink and eat plenty of vegetables, fruit, and foods high in fibre. Exercise can also improve constipation. Sometimes laxatives may be needed to treat constipation.
Some medicines taken for other conditions can interfere with dopamine and make PD worse. These may be prescribed for such things as mental illness, sickness, vertigo and dizziness. Check with your doctor if you are unsure about any medicines that you take.
Driving. If you are a driver you should tell the DVLA and your insurance company if you develop PD. Your insurance may be invalid if you do not. Depending on the severity of symptoms and the medicines that you are taking, you may still be allowed to drive following a medical assessment.
Don’t Miss: Does Magnesium Help Parkinson’s
Movement Disorders Patient Education Resources
The Rush Parkinsons Disease and Movement Disorders Program team is committed to helping people with movement disorders live their best lives. This includes providing comprehensive education to empower patients, families and caregivers to navigate the challenges of a movement disorder diagnosis.
Were pleased to offer the following expert resources, created by or featuring our internationally recognized providers. These videos can help you learn about symptom management, exciting new treatment options, promising research, and strategies for improving your overall health and well-being.

