How Is Lewy Body Disease Diagnosed
There is no specific test for Lewy body disease. A person with symptoms of Lewy body disease will usually be examined and assessed to see what mix of symptoms they have and the timing of the appearance of the symptoms. This can help make a diagnosis of Parkinsons disease, Parkinsons disease with dementia, or dementia with Lewy bodies.
To make a diagnosis, a neurologist, geriatrician or psychiatrist will assess a persons thinking and alertness, whether they have hallucinations, Parkinsons symptoms and how they sleep.
They may want to ask the person and their family members about symptoms. They may ask a person to do a Mini-Mental State Examination a short test to check for problems with thinking and memory.
The doctor may also look at blood pressure, heart rate, body temperature and sweating. They may do blood tests to rule out other conditions.
Scans can show degeneration in the brain, but there is no particular appearance that can diagnose Lewy bodies. However, doctors may suggest an MRI or CT scan of the brain to rule out other causes of dementia.
A SPECT or PET scan may help to support a diagnosis of dementia with Lewy bodies, but at the moment Lewy bodies can only be confirmed by examining brain tissue after death.
A diagnosis of dementia with Lewy bodies is likely if, alongside dementia, a person has the characteristic symptoms of:
In Parkinsons disease dementia, the muscle and movement symptoms are often more severe than the mental problems.
Typical Timescale For Pdd
According to the Parkinsons Foundation, PDD is typically diagnosed when a person living with Parkinsons disease experiences cognitive decline after a year or more of motor symptoms. But in most cases, people experience many years of tremors, slowness of movement, and muscle cramps before showing signs of significant cognitive decline. The Weill Institute for Neurosciences estimates the average time from onset of movement problems to developing dementia is 10 years. An estimated 50% to 80% of people with Parkinsons will eventually experience Parkinsons disease dementia, says the Alzheimers Association.
You May Like: Fatigue In Parkinsons Disease And Potential Interventions
Asceneurons Innovation In Pdd And Dlb
Several symptomatic treatments addressing motoric disturbances in PD are currently available. In contrast, there is a very high unmet medical need for novel symptomatic medications to mitigate the cognitive decline in Parkinsons disease dementia patients, since available options have limited efficacy and considerable side effects. As the disease progresses, balancing the benefits of medications with their side effects becomes challenging for caregivers.
Asceneuron has generated small molecules of novel chemical classes that have the potential to deliver novel, well-tolerated and efficacious drugs to treat learning and memory deficits in dementia. Our positive allosteric modulators of the M1 muscarinic acetylcholine receptor have the potential to bring the first approved treatment for PDD to patients and a new class of molecules for the treatment of dementia in general. M1 PAMs induce a change in the shape of the receptor, enhancing binding to the neurotransmitter acetylcholine. As a result, receptor activity is potentiated so that it can still fulfill its signaling functions, critical for cognition, even in situations where acetylcholine levels are reduced as observed in Parkinsons disease dementia and other dementia in general.
Given the high unmet medical need in PDD, a symptomatic treatment for one of the more debilitating facets of PD would bring significant benefit to PD patients and their caregivers.
Read Also: Parkinson Silverware
Also Check: How Did Surgeons Deliver The Stem Cells To Parkinson’s Patients
Blurred Differences Between Pdd And Dlb
In some PD patients, cognitive impairment may be present. These cases were in the last decade separated into the newly established category of PDD. Interestingly, these patients who manifested typical signs of PD together with cognitive impairment leading to overt dementia had also a different pathological correlate. This was the typical LB pathology accompanied by the presence of A deposits in the limbic system.
It is even more interesting when DLB is also considered. Here the amount of A deposits in the brain should be much higher than in the PDD. The degree of Alzheimers pathology, its magnitude within the brain tissue, and the presence of cerebral amyloid angiopathy is probably the most significant pathological difference between these two phenotypes, PDD and DLB,,,,. Nevertheless, there is no sharp pathological border between these two pictures, it is a smooth transition from the pure PD Lewy pathology to the mixed DLB pathology.
Role Of Lewy Bodies In Neurodegenerative Diseases
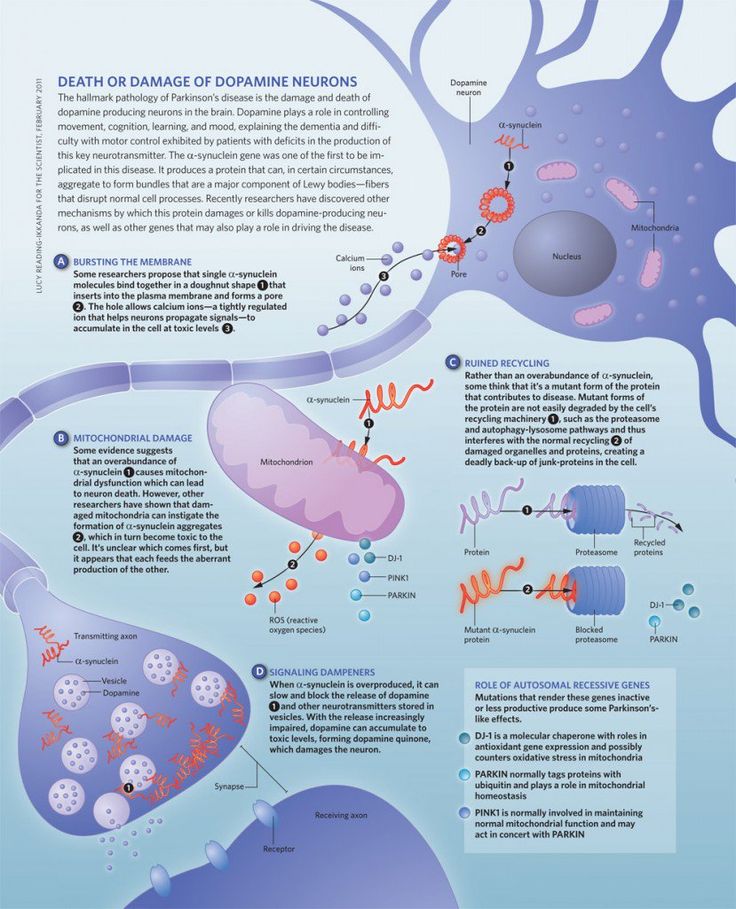
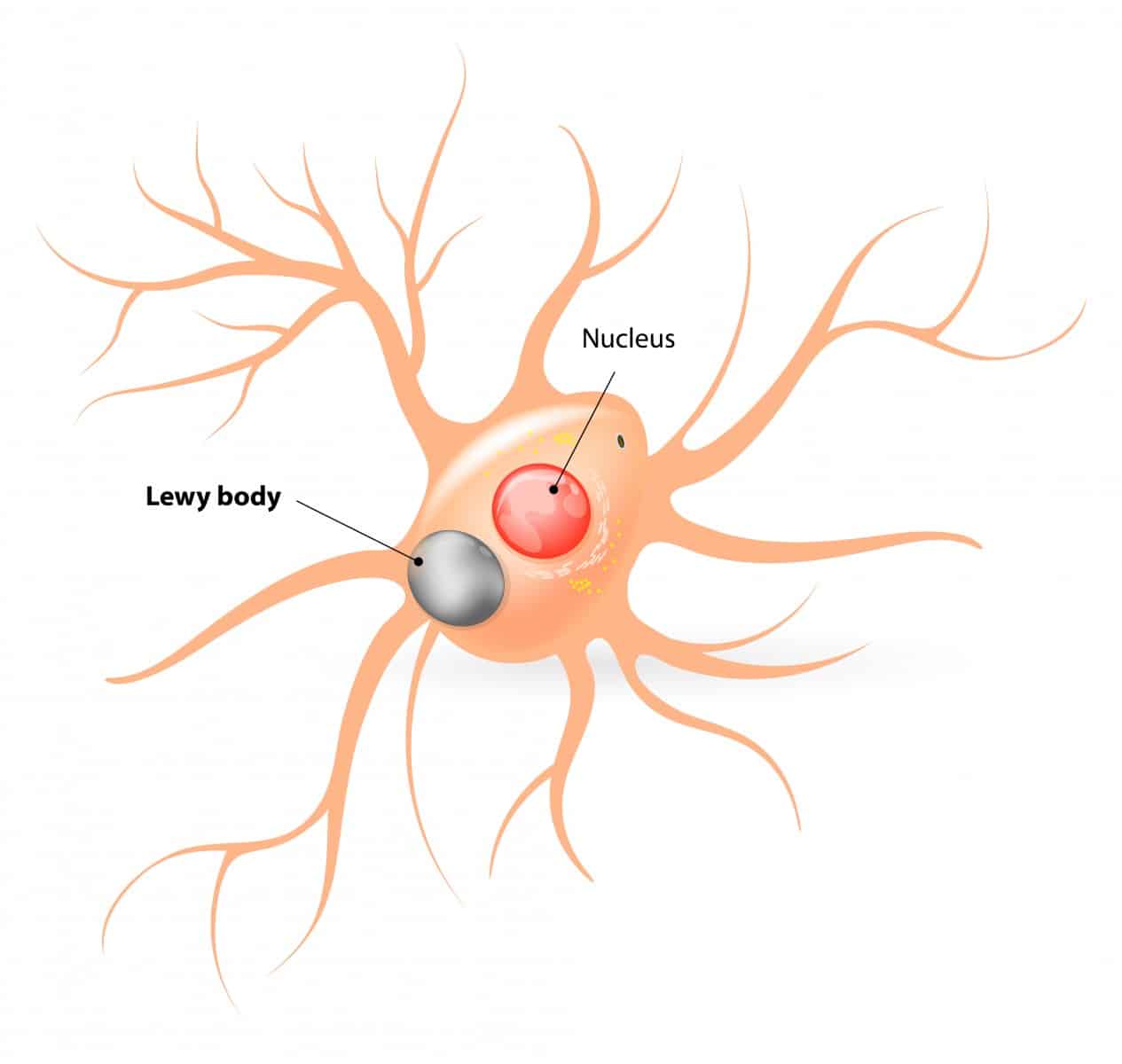
Lewy bodies represent abnormal assemblies of protein molecules inside the neurons in the brain and contribute to the pathology of Parkinson’s disease and other neurodegenerative diseases.
According to Gibb and Lees , Lewy bodies are the neuronal inclusions and are detected in substantia nigra in all cases of Parkinson’s disease. Moreover, the pattern of distribution of Lewy bodies in Parkinson’s disease is generalized. These are found in neurons in the dorsal vagal nucleus, locus coeruleus, nucleus basalis of Meynert, and hypothalamus. Additional regions of the brain including cerebral cortex, autonomic ganglia, and thalamus exhibited the presence of Lewy bodies in Parkinson’s disease . Neurodegeneration is the hallmark in most of the regions in which Lewy bodies have been detected in the brain.
Lewy bodies look like spherical aggregation inside the neurons. Lewy bodies are reported in the brain stem and cortex .
Lewy bodies have 830 m diameter and are made up of nearly 10 nm amyloidogenic fibrils like fibrillary -synuclein and neurofilaments . Lewy bodies have granular and fibrillar cores surrounded by a halo. A single neuron can have more than one Lewy body .
Two types of Lewy bodies have been described namely classical brainstem Lewy bodies and cortical Lewy bodies. The main morphological difference between the two types of Lewy bodies is that cortical Lewy bodies have diffuse outlines and are generally smaller in diameter without the presence of halo .
You May Like: What Does Benadryl Do For Parkinson’s
Parkinsons Disease Dementia And Dementia With Lewy Bodies
The key pathological hallmark found in brains of Parkinsons disease and Parkinsons disease dementia patients are abnormal microscopic deposits composed of -synuclein. This protein is found widely in the brain and its normal function is not yet well understood. The deposits are called Lewy bodies. Lewy bodies are also found in several other neurodegenerative brain disorders, including dementia with Lewy bodies . Evidence suggests that Parkinsons disease and Parkinsons disease dementia, and dementia with Lewy bodies, may be linked to the same underlying abnormalities in caused by the deposition of -synuclein.
Also Check: Is Dementia And Parkinsons The Same
What Are The Symptoms Of Lewy Body Dementia
Lewy body dementia symptoms may resemble those of other neurological disorders, like Alzheimers disease and Parkinsons disease. Symptoms fluctuate over time and vary from person to person.
There are several possible symptoms of LBD, which can be grouped into the following categories:
- Movement issues.
- Smaller handwriting than whats normal for the person.
Cognitive symptoms of Lewy body dementia
Fluctuating cognitive function is a relatively specific feature of Lewy body dementia. A person with LBD may experience periods of being alert and coherent in between periods of being confused and unresponsive to questions. This can change from day to day or within the same day.
Other cognitive symptoms include a decline in:
- Planning abilities.
- Ability to focus.
- Understanding information in visual form.
Visual hallucinations, or seeing things that arent there occur in up to 80% of people with LBD and often early on in the condition. Other types of hallucinations, such as hearing or smelling things that arent there, are less common than visual ones but may also occur.
Visuospatial difficulties, including decreased depth perception, trouble recognizing familiar objects and impaired hand-eye coordination, are also common in people with LBD.
Sleeping problems in Lewy body dementia
Other sleep issues associated with LBD include:
- Excessive daytime drowsiness.
Dysautonomia in Lewy body dementia
- Changes in body temperature.
Dont Miss: Can Head Injury Cause Parkinsons
Read Also: What Are The Early Signs Of Parkinson’s Disease
Treating Movement Symptoms In Lewy Body Dementia
LBD-related movement symptoms may be treated with medications used for Parkinson’s disease, called carbidopa-levodopa. These drugs can help make it easier to walk, get out of bed, and move around. However, they cannot stop or reverse the disease itself. Side effects of this medication can include hallucinations and other psychiatric or behavioral problems. Because of this risk, physicians may recommend not treating mild movement symptoms with medication. Other Parkinson’s medications are less commonly used in people with LBD due to a higher frequency of side effects.
People with LBD may benefit from physical therapy and exercise. Talk with your doctor about what physical activities are best.
Treatment Of Behavior And Mood Problems In Lewy Body Dementia
Behavioral and mood problems in people with LBD can arise from hallucinations, delusions, pain, illness, stress, or anxiety. They may also be the result of frustration, fear, or feeling overwhelmed. The person may resist care or lash out verbally or physically.
Medications are appropriate if the behavior interferes with the person’s care or the safety of the person or others. If medication is used, then the lowest possible dose for the shortest period of time is recommended.
The first step is to visit a doctor to see if a medical condition unrelated to LBD is causing the problem. Injuries, fever, urinary tract or pulmonary infections, pressure ulcers , and constipation can worsen behavioral problems and increase confusion.
Certain medications, such as anticholinergics and antihistamines may also cause behavioral problems. For example, some medications for sleep problems, pain, bladder control, and LBD-related movement symptoms can cause confusion, agitation, hallucinations, and delusions. Similarly, some anti-anxiety medicines can actually increase anxiety in people with LBD. Review your medications with your doctor to determine if any changes are needed.
Antidepressants can be used to treat depression and anxiety, which are common in LBD. Many of them are often well tolerated by people with LBD.
Also Check: Parkinson’s Disease Deep Brain Stimulation Success Rate
Advice For People Living With Lewy Body Dementia
Coping with a diagnosis of LBD and all that follows can be challenging. Getting support from family, friends, and professionals is critical to ensuring the best possible quality of life. Creating a safe environment and preparing for the future are important, too. Take time to focus on your strengths, enjoy each day, and make the most of your time with family and friends. Here are some ways to live with LBD day to day.
Getting Help
Your family and close friends are likely aware of changes in your thinking, movement, or behavior. You may want to tell others about your diagnosis so they can better understand the reason for these changes and learn more about LBD. For example, you could say that you have been diagnosed with a brain disorder called Lewy body dementia, which can affect thinking, movement, and behavior. You can say that you will need more help over time. By sharing your diagnosis with those closest to you, you can build a support team to help you manage LBD.
As LBD progresses, you will likely have more trouble managing everyday tasks such as taking medication, paying bills, and driving. You will gradually need more assistance from family members, friends, and perhaps professional caregivers. Although you may be reluctant to get help, try to let others partner with you so you can manage responsibilities together. Remember, LBD affects your loved ones, too. You can help reduce their stress when you accept their assistance.
Consider Safety
Plan for Your Future
Different Conformational Properties Of
Another aspect supporting the fact that LBs are not the key players in neurodegeneration is the description of different Syn strains differing in conformational properties. These strains exhibit different cell toxicity and differences in the ability to induce tau protein aggregation. This is again a situation where pathological processes preceding the formation of LBs may affect the course and progression of the disease. Thus, different Syn strains may also be the factor involved in the phenotypic variability of this group of diseases,. It is probable that as yet unknown genetic factors will apply here.
Also Check: How Does A Person Get Parkinson’s
What Causes Lewy Body Disease
Lewy body disease is caused by abnormal clumps of protein, called Lewy bodies, developing inside nerve cells in the brain. This leads to the degeneration and death of the nerve cells.
It is not known why Lewy bodies develop. No risk factors have been clearly identified so far, but dementia with Lewy bodies does seem to have a genetic component.
Deficiency Of Parkinsons Disease Society Brain Bank Criteria
The clinical diagnosis of PD has been established in the past 30 years mainly based on the UK-PDSBB, first proposed in 1988. These were later validated in two clinico-pathological studies carried out at Queen Square, in Hughes original study in 1992 and its replication published in 2001 and 2002,,. The criteria were created using the clinical notes and data retrieved from general practitioner files and their retrospective correlation with pathological findings. From todays point of view, it is therefore questionable, whether these criteria will resist the light of todays molecular genetics and molecular biology state of the art.
The key players in this field are currently the numbers of gene variants, causal or associated with the manifestation of typical PD, combined with epigenetic factors, and Braaks concept formulated almost 20 years ago,,. Nevertheless, thehotspot should be the observations that the pathological neurodegenerative process might manifest in a quite different way than usually described and known ,,,,,.
Table 2 Arguments against the current concept of Lewy body diseases.
Read Also: Parkinson’s Walk Central Park
Analysis Of The Overall Composition Of Gut Microbiota
We performed PERMANOVA to examine the overall composition of gut microbiota in controls and DLB . The overall composition of gut microbiota between controls and DLB was statistically different by all three distance metrics . We also found that age, sex, and PPI affected the overall composition of gut microbiota . Donepezil and memantine, both of which were used to treat dementia, did not affect the overall composition of gut microbiota in DLB patients . PERMANOVA analyses between controls and PD and between controls and iRBD were performed previously using almost the same samples, and were not repeated in this communication.
Table 2 PERMANOVA to examine the effect of each factor on the overall bacterial composition.
Caring For A Person With Lewy Body Dementia
On this page:
As someone caring for a person with Lewy body dementia , you will take on many different responsibilities over time. You do not have to face these responsibilities alone. Many sources of help are available, from adult day centers and respite care to online and in-person support groups.
Below are some actions you can take to adjust to your new roles, be realistic about your situation, and care for yourself.
Don’t Miss: Can Drugs Cause Parkinson’s Disease
Common Symptoms Of Lewy Body Dementia
The disease of Lewy Body Dementia affects cognitive response, changes physical and sleep pattern along with changing behavioral features. Some people may start developing the disorder in movement in the initial stage that further leads to dementia. This is often termed as Parkinsons disease dementia.
Another group of people may start developing cognitive disorder with two or more distinctive features of dementia. There are very few people that come up with neuropsychiatric symptoms. These include hallucinations, behavioral problems, and complex mental activities.
Generic symptoms of Lewy Body Dementia include:
- Impaired thinking like loss of execution, planning, processing and/or ability to understand visual information
- Fluctuation in alertness, attention, and cognition
- Sudden tremors, stiffness, and difficulty in walking
- Changes in bodily functions like blood pressure, temperature regulation bowel and bladder function.
What Is Dementia With Lewy Body Disease
Dementia with Lewy body disease is a condition that causes changes in thinking, behavior, and movement. DLB usually starts with thinking and behavior changes that are followed by problems with movement. The movement problems in DLB are similar to those seen in people with more classical Parkinsons disease.
Recommended Reading: Does Parkinson’s Disease Make You Shake
Pathogenic Mechanisms Beyond Lbs Or Lbs As An Indirect Indicator Of This Disease Spectrum
As follows from the previous consideration, the current concept behind classification within this disease spectrum is still based on retrospective clinicopathological studies, which focused exclusively on the presence of LBs and their clinicopathological relevance. However, since the initial description of LBs as a pathological hallmark of PD and the formulation of Braaks concept of the specific spread of LB pathology, evidence has been accumulating that not only LBs are key players in this group of diseases. So, what is the true significance of LBs in the pathogenesis of this disease spectrum, and what are the other biological relationships between the entities for which LBs are a common link?
Tips For Communicating With A Person With Pdd
PD-related mood and motor changes can impact communication cognitive changes and Parkinsons disease dementia can further these difficulties.
- Stay calm and be patient. It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- Acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior. Can your loved one be hungry, thirsty, tired, in pain, frustrated, lonely or bored?
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- Its okay to use humor to diffuse stressful situations but avoid negative humor or sarcasm these can be misunderstood.
Page reviewed by Dr. Chauncey Spears, Clinical Assistant Professor and Dr. Sydney M. Spagna, Clinical Fellow at the University of Michigan.
You May Like: What Happens When Parkinson’s Medication Stops Working
