A Study To Evaluate The Efficacy And Safety Of Intravenous Prasinezumab In Participants With Early Parkinsons Disease
open to eligible people ages 50-85
This is a multicenter, randomized, double-blind, placebo-controlled study that will evaluate the efficacy and safety of intravenous prasinezumab versus placebo in participants with Early Parkinsons Disease who are on stable symptomatic PD medication.
San Francisco, California
Using Machine Learning In Research
The available treatments for Parkinsons disease to date are only partially effective and fail to markedly delay disease progression. Thus, there is growing interest in repurposing existing medications as an accelerated method of therapeutic development.
Such approved treatments, having already been rigorously tested in clinical trials, generally have established safety profiles.
Studies have suggested that people treated with certain medications, including immunosuppressants or those that widen the airways, called bronchodilators, have a lower risk of developing Parkinsons.
These findings prompted researchers based at the Université Paris-Saclay, in France, to use machine learning tools to automatically screen a large database of marketed therapies to detect those related to a lower risk of Parkinsons.
This study is part of a research effort aimed at identifying already-developed compounds associated with reduced risk, the researchers noted.
Data were collected from the French national health data system. A total of 40,760 incident Parkinsons patients were identified based on the details of at least one claim for an anti-Parkinsons medication from 2016 to 2018. A control group of 176,395 individuals of similar age, sex, and area of residence were included as a comparison.
Given that, the team assessed therapeutic exposure and related factors during the two years before the lag period to find associations to a reduced risk of developing Parkinsons disease.
Oxidative Stress May Have Key Role In Parkinsons Dementia Study Finds
A team led by researchers in Denmark, Spain, and Sweden analyzed data from the Swedish Neuro Registries/Parkinsons Disease Swedish PD Registry , a large register that contains clinical and patient-reported data outcomes from about 9,650 Parkinsons patients.
Specifically, they analyzed data collected in April 2020 from 1,581 patients with Parkinsons in Scania, the southernmost region of Sweden. Patients data were age- and sex-matched with people randomly selected from the general population of Scania without Parkinsons who served as the control group.
Time to dementia was defined as the time from Parkinsons diagnosis to the first health care visit where a dementia event was registered. These included unspecified dementia, Alzheimers dementia, vascular dementia, or dementia linked with other diseases.
In a first analysis, a real case of dementia was registered when a person had at least two dementia-related health care visits. In a second analysis, dementia was defined when a prescription for an anti-dementia medication was given.
The risk of dementia was higher among people with Parkinsons when compared to controls, with the difference between both groups accentuating over time, a statistical analysis over 25 years of follow-up showed. The risk was always higher for people with Parkinsons ranging from 3.5 to 6.1 times higher when compared to controls depending on the criterium used for defining dementia.
Don’t Miss: How To Stop Dyskinesia In Parkinson’s
Survival In Parkinson’s Disease Psychosis
LaFaver: Let’s switch gears a little bit with our next abstract here, which is titled, “Survival Differences Among Patients with Parkinson’s Disease and Parkinson’s Disease Psychosis: a Population-based Study .” This comes from Dr Rodolfo Savica, who is at the Mayo Clinic and is a friend of mine, and his colleagues. They’ve done amazing epidemiologic studies based on the Rochester Epidemiology Project.
I found this study very interesting, because it’s something that hasn’t been looked at specifically. Patients will always ask, how does Parkinson’s disease affect my long-term prognosis and so on. We know that in general, there’s not a large difference in life expectancy. But this study looked at how patients who experience psychosis do using this amazing database. They looked at 69 patients out of 225 with Parkinson’s disease over a 10-year time span.
They found that patients who had met criteria for Parkinson’s disease psychosis showed higher rates of cognitive impairment . That’s probably not too surprising. They also had higher rates of orthostatic hypotension and a significantly higher rate of all-cause mortality.
We know that Parkinson’s disease is not one disease, but it’s really a spectrum. Knowing which patients we really need to pay a lot of attention to and who might be frailer and higher-risk is important.
What Is Parkinsons Disease
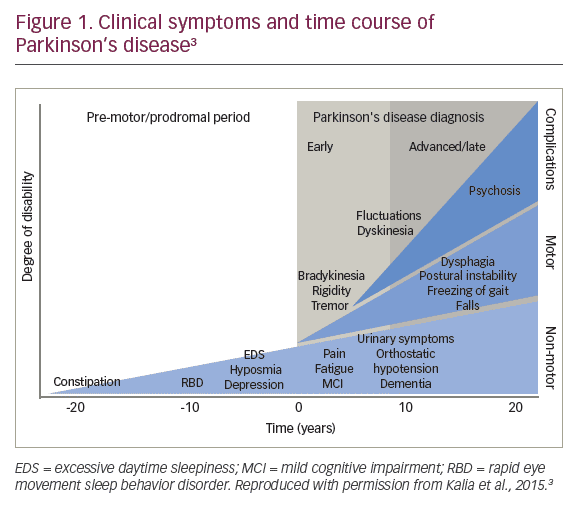
Parkinsons disease is a progressive brain disorder that causes shaking and muscle stiffness, and slows movement. It develops when neurons in a particular part of the brain stop working properly and are lost over time. These neurons produce an important chemical called dopamine. Dopamine is used by the brain to send messages across brain areas to help control movement. Eventually, the brain cannot make enough dopamine to control the movement properly.1,2
Dont Miss: Parkinsons Disease Dementia Prognosis
Read Also: Boxing Therapy For Parkinson’s Disease
Why Scientists Believe Theyve Made New Breakthrough In Parkinsons Disease Treatment By Building On Gdnf Research
The Finnish researchers are now working to improve the properties of BT13 to make it more effective as a potential treatment that could benefit many people living with the disease.
The study, which was published online yesterday in the journal Movement Disorders, builds on previous research on another molecule that targets the same receptors in the brain.
GDNF or glial cell line-derived neurotrophic factor is an experimental treatment for Parkinsons discovered in 1993 that has been shown to bring dying brain cells back to life and particularly effective in dopamine neurons.
It was the subject of a BBC documentary in February 2019 that followed a phase two trial in Bristol involving 42 patients. While the results werent clear cut, GDNF has shown promise to restore damaged cells in people with Parkinsons.
However, the GDNF protein requires complex robot-assisted surgery to deliver the treatment to the brain because its a large molecule that cant cross the blood-brain barrier a protective wall that prevents some drugs from getting into the brain.
BT13 is a smaller molecule that is able to cross the blood-brain barrier and therefore could be more easily administered as a treatment if shown to be beneficial in further clinical trials.
Dr Yulia Sidorova, lead researcher on the study, said: We are constantly working on improving the effectiveness of BT13.
Our ultimate goal is to progress these compounds to clinical trials in a few coming years.
Related Article
What Will A Cure For Parkinson’s Look Like
Parkinson’s varies so much from person to person. There are over 40 symptoms of Parkinsons. Tremor. Pain. Hallucinations. Everyones experience is different.
Because of this, there may not be a single ‘cure’.
Instead, we may need a range of different therapies to meet the needs of the individual and their specific form of the condition.
This mix may include treatments, therapies and strategies that can:
- slow or stop the progression of the condition
- replace or repair lost or damaged brain cells
- control and manage particular symptoms
- diagnose Parkinson’s at the earliest possible stage.
And this could involve medical treatments, such as drugs and surgical approaches, as well as lifestyle changes, for example to diet and exercise.
You May Like: Can Parkinsons Be Slowed Down
Can Parkinsons Patients Live A Normal Life
Velma West | Answered June 27, 2020
Parkinsons disease does not directly cause people to die, but the condition can place great strain on the body, and can make some people more vulnerable to serious and life-threatening infections. But with advances in treatment, most people with Parkinsons disease now have a normal or near-normal life expectancy.
What Will The Next Generation Of Clinical Trials Focus On
There are many symptoms of Parkinsons disease. Theyre often rated using the Unified Parkinsons Disease Rating Scale or the Movement Disorder Societys updated revision of that scale, the MDS-UPDRS.
Clinical trials today are generally looking to significantly improve UPDRS or MDS-UPDRS scores for people with Parkinsons disease.
Some trials are testing new delivery methods, such as intravenous infusion or topical applications. Others are looking to determine the safest number of effective doses. And other trials are measuring overall safety while using new medical devices in stem cell therapy.
This is an active area of research. Future trials will help narrow down the most safe and effective approach to stem cell therapy for Parkinsons disease.
Each phase adds more participants, with the first phase usually limited to a few dozen people and several thousand in the third phase. The purpose is to test the treatments safety and effectiveness.
Clinical trials testing stem cell therapy for Parkinsons disease are still in the early phases. If the current trials are successful, it will likely still be 4 to 8 years before this treatment is widely available.
Recommended Reading: Death Due To Parkinson’s Disease
Common Scale Of Motor Symptom Severity May Have Flaws: Study
A commonly used measure of how motor symptoms are affecting daily life could also for people in early stages of Parkinsons disease be taking into account the contribution of their non-motor symptoms, a study suggests. This is a likely reason for the discrepancies seen in evaluations made by patients
Adaptive Deep Brain Stimulation To Improve Motor And Gait Functions In Parkinson’s Disease
Sorry, accepting new patients by invitation only
This is a single-center phase I clinical study aiming to improve gait functions in patients with Parkinson’s disease by using adaptive neurostimulation to the pallidum. The investigators will use a bidirectional deep brain stimulation device with sensing and stimulation capabilities to 1) decode the physiological signatures of gait and gait adaptation by recording neural activities from the motor cortical areas and the globus pallidus during natural walking and a gait adaptation task, and 2) develop an adaptive deep brain stimulation paradigm to selectively stimulate the pallidum during different phases of the gait cycle and measure improvements in gait parameters. This is the first exploration of network dynamics of gait in PD using chronically implanted cortical and subcortical electrodes. In addition to providing insights into a fundamental process, the proposed therapy will deliver personalized neurostimulation based on individual physiological biomarkers to enhance locomotor skills in patients with PD. Ten patients with idiopathic Parkinson’s disease undergoing evaluation for DBS implantation will be enrolled in this single treatment arm study.
San Francisco, California
Sorry, in progress, not accepting new patients
This study will investigate cortical stimulation to treat mood and behavioral symptoms in Parkinson’s disease patients.
San Francisco, California
You May Like: What Are The Very Early Symptoms Of Parkinson’s Disease
Scientists Homing In On A Cure For Parkinsons Disease Scitechdaily
The new peptide shows promise as a drug precursor to treat Parkinsons disease, often known for its distinctive hand tremors.
A peptide known to prevent the protein error that gives rise to Parkinsons disease has been optimized by scientists, making it a strong candidate for future development into a cure.
A molecule that shows promise in preventing Parkinsons disease has been refined by scientists at the University of Bath and has the potential to be developed into a drug to treat the incurable neurodegenerative disease.Professor Jody Mason, who led the research from the Department of Biology and Biochemistry, said: A lot of work still needs to happen, but this molecule has the potential to be a precursor to a drug. Today there are only medicines to treat the symptoms of Parkinsons we hope to develop a drug that can return people to good health even before symptoms develop.
Read more at:
Studies Show Promising Results
“Considering the ability of MSCs to secrete neurotrophic factors, modulate inflammation, and possibly even act as mitochondria âdonorâ, it comes as no surprise that there is a lot of interest in the use of MSCs in the treatment of Parkinsons Disease, and a multitude of animal studies has shown promise. Treatments have resulted in improvement of motor function, protection of the nigrostriatal system, and improved striatal dopamine release in several studies using toxic lesion rodent models of Parkinsons Disease. Similar effects were reported with umbilical cord-derived MSCs with or without prior differentiation. For example, a recent study reported improvement of motor function, reduced microglial activation, and decreased loss of TH immunoreactivity, associated with local production of trophic factors.
Learn more about DVC Stem’s protocol for Parkinson’s Disease here:
References:
Venkataramana, N. K., Kumar, S. K. V., Balaraju, S., Radhakrishnan, R. C., Bansal, A., Dixit, A., ⦠Totey, S. M. . Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease. Retrieved from https://www.sciencedirect.com/science/article/pii/S1931524409002205#!
Unified Parkinson’s Disease Rating Scale. . Retrieved from https://www.sciencedirect.com/topics/medicine-and-dentistry/unified-parkinsons-disease-rating-scale
About the author
Recommended Reading: Is Parkinson’s Disease Genetic Or Hereditary
Diet And Lifestyle Changes
Additional therapies for Parkinsons disease treatment include eating a healthy diet and engaging in regular exercise.
Some individuals may benefit from participating in physical and occupational therapy. These therapies often focus on balance, improving your gait, or tactics to allow you to complete your work.
Other alternative options center on promoting holistic well-being while living with Parkinsons disease. These are not shown to stop the diseases progression but can help you manage symptoms and stay hopeful:
Genau Charity Rally San Francisco Ca
Date: October 22, 2022
All Makes | DTAC Day
This time we are heading to the famous backroads and coast of the Peninsula and South Bay. Oh boy, do we have some treats for you! We will meet at 8am at scenic Thomas Fogarty Winery in Woodside before heading out on a great 3 hour drive with time for a break in the middle and winding up at Canepa!
Recommended Reading: How To Deal With Parkinson’s Delusions
What Age Does Parkinsons Usually Start
Maxine Wolfe | Answered April 8, 2021
One clear risk is age: Although most people with Parkinsons first develop the disease after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinsons are often, but not always, inherited, and some forms have been linked to specific gene mutations.Oct 6, 2022
Stem Cell Therapy For Parkinson’s Disease
Stem cell therapy may have the benefit of replacing and repairing damaged dopamine-producing nerve cells within the brain. This has already been found in a study conducted by Neelam K.Venkataramana and colleagues. Seven PD patients aged 22 to 62 years with a mean duration of disease 14.7 ± 7.56 years were enrolled to participate in the prospective, uncontrolled, pilot study of single-dose, unilateral transplantation of autologous bone-marrow-derived mesenchymal stem cells . Patients were followed up for 36 months post-transplant, 3 of the 7 patients showed significant improvement in their Unified Parkinson’s Disease Rating Scale of 38%.
According to Medical News Today “Currently, the most common therapy uses the drug levodopa to stimulate dopamine production in certain neurons associated with motor skills. These dopaminergic neurons are situated in the nigrostriatal pathway which is a brain circuit that connects neurons in the substantia nigra pars compacta with the dorsal striatum. However, levodopa has a wide array of side effects, from physiological to psychological ones. Also, in the long-term, the benefits of such dopamine-regulating drugs are limited. So, scientists must come up with more effective strategies for repairing the brain damage that Parkinson’s disease causes.”
Recommended Reading: Is Forgetfulness A Symptom Of Parkinson’s Disease
How Could Stem Cells Help People With Parkinsons
Stem cells are the parent cells of all tissues in the body. This means they can turn into any type of cell. The hope is that they will eventually be able to make these cells into specific types of cells, like dopamine-producing neurons, that can be used to treat Parkinsons disease. However, there are concerns that patients may have the same risk of increased involuntary movements as those who undergo fetal cell transplantation. And, like fetal cell transplantation, stem cell therapy is surrounded by moral and ethical controversy.
Current Parkinsons Treatments Cant Slow Down Onset Of Disease
Parkinsons is a long-term degenerative disorder of the central nervous system, which mainly the area of the brain that controls movement leading to a slow onset of symptoms including tremors, rigidity and slow movement.
More than 10 million people worldwide are estimated to be living with Parkinsons disease, according to the US-based Parkinsons Foundation, with the Parkinsons News Today website saying it affects 1,900 per 100,000 among those aged over 80,
Typically, by the time people are diagnosed with the condition, they have already lost between 70% and 80% of their dopamine-producing cells, which are involved in co-ordinating movement.
While current treatments mask the symptoms, there is nothing that can slow down its progression or prevent more brain cells from being lost.
As dopamine levels continue to fall, symptoms get worse and new symptoms can appear.
Also Check: What Triggers Parkinson’s Disease
Important Points About The New Medications
With multiple new medications available for the treatment of PD, there is more hope than ever that Parkinsons symptoms can be successfully managed for many years. A few things to consider:
- For people whose symptoms are difficult to control, these new treatments are welcome additions to what was previously available and many people with PD have been using these new medications with significant benefit.
- On the other hand, many of the newly-approved medications have the same mechanisms of action as older medications so they are not breaking new ground in treating symptoms.
- In addition, for some people, the effect on symptoms may be mild or not substantial.
These caveats may mean that your physician has not suggested a medication change for you. It is also important to note that despite all the new medications, carbidopa/levodopa remains the most potent medication to treat the motor symptoms of PD.
If your doctor does choose to try one of the new options, there may be multiple paths that your doctor can take when contemplating a medication adjustment. Often trial and error is the only way to determine the best medication regimen for you, so you may need to practice some patience as you work together with your doctor to determine what works or doesnt work.
This research also has implications for Alzheimers disease, Type 2 diabetes and other serious human diseases where symptoms are triggered by protein misfolding.
Explore further

