More Research Is Needed
There are a limited number of studies that have investigated the relationship between the development of peripheral neuropathy and Parkinsons. Some small studies have found the frequency of neuropathies was significantly higher in PD patients than in controls.1
There are investigative questions that have been raised about a correlation of prolonged levodopa usage and according to some studies, there is insignificant evidence to link levodopa usage with the development of peripheral neuropathies in people with idiopathic Parkinsons.1
Therefore further investigation is required to evaluate whether PN could be another element of the disease or related to treatment medications, or some combination of the two.1
The Peripheral Nervous System And Parkinsons Disease
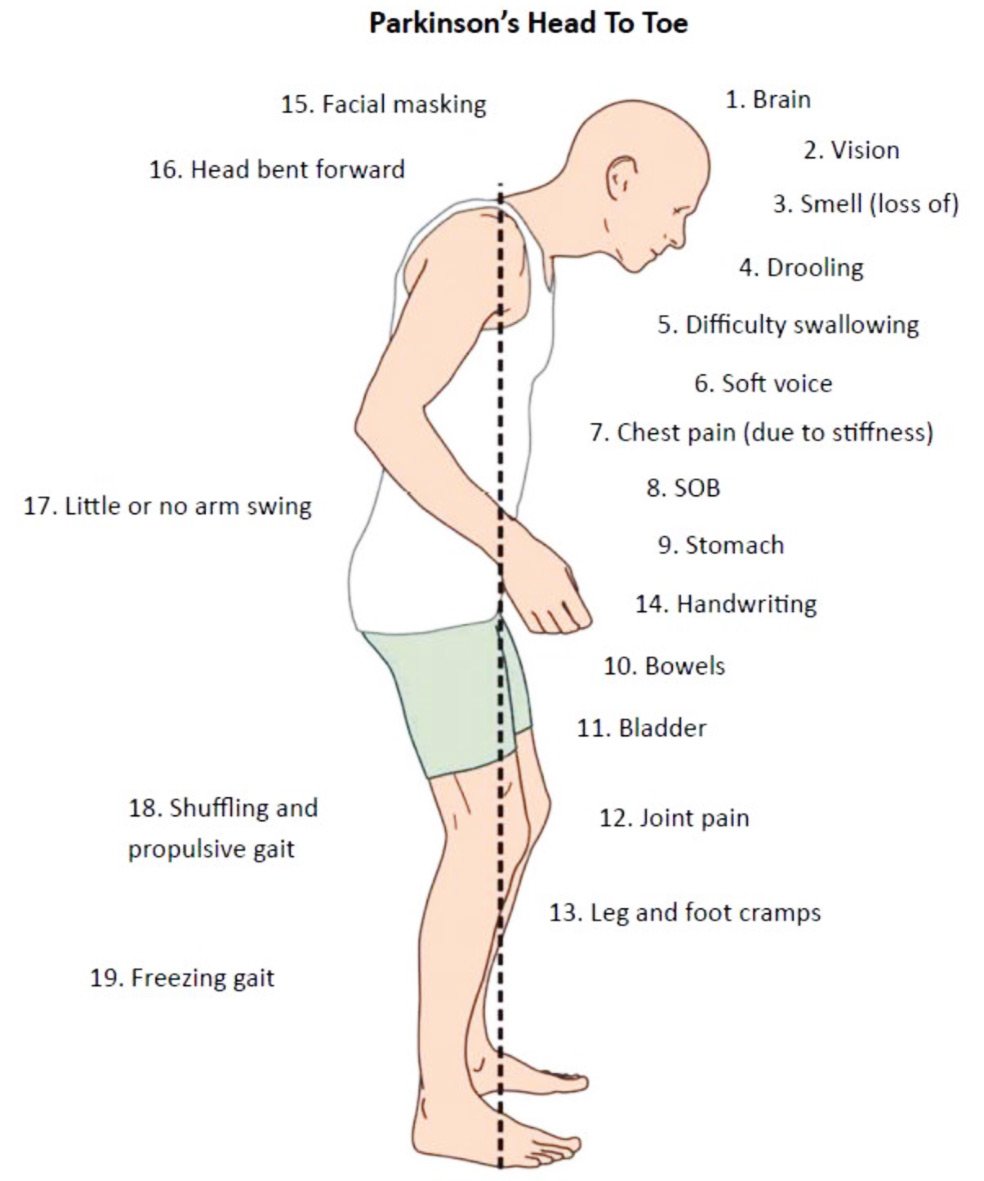
It is well-established that the autonomic nervous system can be significantly affected in PD causing symptoms such as constipation, urinary dysfunction and orthostatic hypotension. The autonomic nerves that bring signals to the gut for example, can be directly affected by Lewy body-like accumulations and neurodegeneration.
What remains unclear is if motor and sensory nerves are also affected in PD.
What Kinds Of Pain Can Be Part Of Parkinsons
At its simplest, pain means the body hurts. When a person feels pain, nerves in the skin, joints and organs alert the brain to the location of an injury. Researchers have found that in early PD, there are already changes in the way that the body detects and regulates pain. Pain is complex and can take many forms. In PD, pain tends to affect the side of the body where motor symptoms first appeared. If your PD started with a tremor in the right hand, youre more likely to develop pain in the right shoulder, wrist or fingers. Here are a few common types.
Musculoskeletal pain
Musculoskeletal pain is experienced by up to 75 percent of people with PD and includes pain in the muscles, bones or skeleton. It is related to rigidity and decreased movement, and to arthritis. Many people with PD experience muscle cramps and tightness in the neck, spine and arms. Muscles may feel stiff or achy. Joint pain, especially in one shoulder, is also common. Its not uncommon for people with PD to be diagnosed with frozen shoulder or rotator cuff problems, and even undergo surgery.
Dystonic pain
Neuropathic pain
Central pain
Central pain affects about 10 percent of people with PD at some point. It can be difficult to describe but may include a vague, constant boring sensation abdominal pain, reflux, shortness of breath or feeling flushed painful sensations around the mouth, genital or rectal areas or simply pain all over.
Also Check: What Type Of Doctor Treats Parkinson’s
Q Can Parkinsons Disease Affect My Sex Life
A. Reduced libido and impotence can result from physical and/or psychological factors of Parkinsons disease. In addition, some of the medicines used to treat the symptoms of Parkinsons disease can cause sexual dysfunction in men, and vaginal dryness in women. Fatigue can make matters worse.
It may help to try having sex in the morning after taking your medication. Medicines are available to help men with erectile difficulties, and vaginal lubricants may be of help to women.
You May Like: Alan Alda Parkinsons Diagnosis
How To Cope With Dystonia
I have PD. First thing in the morning as I am getting out of bed, my left foot cramps severely and my toes curl downward, making it very painful to walk. I have found that it helps if I put my feet flat on the floor immediately after sitting up in bed. Also foot massages help. If I can force the cramped foot so it turns outward, my toes uncurl. nelleford
When my dads legs cramp, massage helps relieve them. You can usually feel where the spasms are. Rub your hands together to warm them up first. Start below where the spasm is and work up towards them. With your fingers and palms, give a deep massage where the cramp is. Give your loved one mustard or pickles to relieve the cramp. I know it is weird, but it works. To prevent them, exercise is best. Try to get them to walk every day, even if it is only half a block. This will also help prevent falls. A good multivitamin every day can be beneficial. Look for one with magnesium and potassium in it. These minerals helps to prevent cramping. My dad eats bananas almost every day for this reason. kathyt1
Calcium governs muscle contraction, and magnesium governs muscle relaxation. I take a magnesium supplement if Im having leg cramps. Perhaps have your loved ones levels evaluated with a simple blood test. Potassium can be dangerous if its too high or too low, and too low can often cause muscle cramps. sherry1anne
Recommended Reading: What Medication Is Used For Parkinsons Disease
Read Also: Can Parkinson’s Start In The Legs
Types Of Parkinson’s Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
These Treatments And Interventions May Help
Interventions tend to be most successful in the earlier stages, so you should bring your symptoms to your doctors attention as you notice that youre having trouble flexing the joints of your toes, says the Cleveland Clinic.
Several treatment options may be available, which you can utilize in addition to pain management or anti-inflammatory medication, explains Scudday. For more extreme or painful cases that do not respond to conservative treatment, surgery may be recommended as an option. Both hammertoe and claw toe can be surgically reconstructed and realigned into proper position or the entire toe joint can be replaced, says the podiatrist. The patient may also consider wearing different shoes, padding their shoes, wearing arch support inserts, or practicing toe-strengthening exercises as a form of physical therapy.
And, of course, be sure to speak with your doctor about the underlying cause for the changes in your toes. If a neurological disease such as Parkinsons is responsible, timely intervention for that condition may significantly improve your quality of life.
Seated Option: Calf Stretch with Strap
Recommended Reading: When Was Muhammad Ali Diagnosed With Parkinson’s Disease
Results Of Small Fiber Neuropathy Assessment
Skin Wrinkling Test was performed in 49 patients, 33 with PD and 15 with other forms of parkinsonism. No statistical difference was observed in the percentage of patients with abnormal SWT between the 2 groups: 19 out of 33 of the PD group and 6 out of 15 of the patients with parkinsonism . Among the patients with evidence of small fiber neuropathy in the PD group, 10 % had diabetes, 5 % thyroid disease, 5 % B12 deficiency and 5 % had been treated for leprosy in the past while additional 15 % had B12 levels < 300. Among the patients with evidence of small fiber neuropathy in the parkinsonism group, 12.5 % had diabetes mellitus. Therefore, in 65 % of the PD patients and among 87.5 % of the patients with parkinsonism, no common etiology of peripheral neuropathy was identified.
Peripheral Neuropathy And Parkinsons Disease
A number of studies have tried to determine if PN is more common among people with PD as opposed to people without PD. PN is a relatively common condition in the general population, which makes it difficult to ascertain whether or not it is even more common among people with PD.
The available studies have varying results and are difficult to compare with each other as they:
- Include different types of populations of people with PD
- Assess peripheral neuropathy differently
- Assess for causes of peripheral neuropathy differently
A recent review looked at all the available data and determined that large fiber neuropathy was present in 16% of patients with PD, about double the prevalence of this condition in the general population. Skin biopsy-proven small fiber neuropathy was present in over 50% of people with PD, although this result was based on a small sample of patients.
Don’t Miss: Can Parkinson’s Cause Depression
S Of The Body Affected By Dystonia
People with Parkinson’s can experience this disease-related cramping or clenching differently. Areas impacted include:
- Arms, hands, legs and feet: Involuntary movements, spasms or twisting and “curling”
- Neck: May twist uncomfortably, causing the head to be pulled down or to the side. This is called cervical dystonia or spasmodic torticollis
- Muscles around the eyes: May squeeze involuntarily, leading to a person to blink too much or to have difficulty opening the eyes also called blepharospasm.
- Vocal cords and swallowing muscles: May cause a person’s voice to sound softened, hoarse or breathy
- Jaw: May open or close forcefully or there may be grimacing of the face
- Abdominal wall: May cause sustained contractions, involuntary, writhing movements of the abdominal wall, or grimacing of the face
General Aspects Of Pain Treatment In Pd
Despite the high prevalence of pain in PD, literature data suggest that only up to a maximum of 50% of PD patients receive at least some type of pain therapy .
Still, the fundament of pain therapy should be an optimized dopaminergic treatment which can improve pain related to insufficient dopaminergic supply such as akinesia and/or rigidity , pain due to dopaminergic over-supply such as dyskinesia and/or dystonia , or central pain that is dopamine-sensitive . This concept was reported to be effective in about 30% of PD patients . A standardized levodopa test can be helpful to decide whether the pain is dopaminergic responsive or not, but any result of this short-term effect must always be interpreted with caution so that the long-term assessment of pain under dopaminergic therapy over several weeks remains essential .
A systematic review and meta-analysis including databases from January 2014 until February 2018 investigated the efficacy of a variety of novel, complimentary, and conventional treatments for pain in PD and found the greatest reduction in pain for safinamide, followed by cannabinoids and opioids, multidisciplinary team care, COMT-inhibitors, and electrical and Chinese therapies, while the weakest effects were obtained for dopaminergic agonists and miscellaneous therapies . Table 1 gives an overview of larger randomized controlled trials of antiparkinsonian drugs and opioids assessing the effect on pain in PD patients.
Table 1
Fig.1
Don’t Miss: When Life Gives You Parkinson’s
Dystonia In Parkinsons Disease
Dystonia refers to a condition in which the muscles repeatedly contract or twist involuntarily, leading to movement and postural abnormalities. Dystonia can affect a single muscle, a group of muscles, or the whole body. These symptoms can occur on their own or as a symptom of another disorder, such as Parkinsons disease. Dystonia does not always indicate a person has PD, and not every person with Parkinsons will experience dystonia.
When dystonia does occur in PD, it frequently affects the feet and toes. A significant portion of people with Parkinsons disease awake with painful cramping in one or both feet. Dystonic Parkinsons disease also can cause a rare condition called cervical dystonia . Cervical dystonia causes involuntary in the neck that cause painful misalignment of the spine. Fortunately, the vast majority of people with PD will not develop this type of dystonia.
Recommended Reading: First Signs Of Parkinsons Disease Uk
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
You May Like: Adaptive Silverware For Parkinsons
Also Check: Is Ashwagandha Good For Parkinson’s
Additional Ways To Stop Foot Cramping
Aside from the strategies mentioned with each cause of foot cramping above, there are several other things you can do for foot cramps. Massaging your feet, especially in the middle of a cramp, can help. If you are in pain, try taking an over-the-counter pain reliever. Cool or hot compresses can also relieve muscle pain.
In a recent study at Brigham Young University, researchers found that pickle juice was effective at stopping exercise-induced cramps once they started.20Scientists arent sure why this worked, but they think it may have something to do with muscle fatigue.
Types Of Parkinsons Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
Read Also: Is Parkinsons A Form Of Cancer
Also Check: How Old Does Parkinson’s Start
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinsons disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physicians attention in the right direction to accurately diagnose your pain.
Leg Pain And Parkinsons
Interestingly enough, one of my early symptoms of the disease was deep searing pain in my left leg, the type of pain my grandma had complained about many times. Initially this type of pain was worst in the morning as well as at night, making me think is was some sort of fasciitis. However not only did typical anti-inflammatories and muscle relaxants not alleviate my pain but pain worsened over time to a constant burning pain that felt as if someone was tearing the muscle and pouring hot oil on it. The pain was so excruciating it was permeating into all aspects of my life. I was constantly in need of deep tissue massage asking my husband to massage my legs just as my grandmother had asked of us time and time again. This helped only temporarily.
Which brings me to the four types of leg pain in PD.
You May Like: What Is The Prognosis For Parkinsons Disease
Also Check: How To Care For Parkinson’s Disease Patient At Home
Common Skeletal & Bone Changes With Pd
- Frozen shoulder: stiffness, pain and loss of range of movement in the shoulder, many people experience this symptom before a PD diagnosis.
- Flexed fingers, toes or feet : one finger may extend, the thumb may fold inwards, fingers may clamp down onto the palm. In the leg, the foot may flex down or turn in, the big toe may flex upward while the other toes curl under.
- Stooped posture : the spine bends forward when walking, in the most severe cases by as much as 90 degrees. This posture arises because the hips and knees are flexed and will go away when lying down.
- Leaning sideways : involuntarily tilting of the trunk to one side when sitting, standing or walking always to the same side.
- Scoliosis: sideways twisting, or curvature, of the spine.
- Dropped head : the head and neck flex forward the chin may drop all the way down to the sternum or breastbone .
- Bone fractures: people with PD are at risk of broken bones from falling, especially from landing on the hip. Kneecap fractures also are common, painful and sometimes overlooked.
- Low bone density/osteoporosis: bones may become weak and at risk for osteoporosis from lack of weight-bearing exercise, like walking, and from too little calcium and vitamin D. Other risk factors for osteoporosis include older age, female sex, low body weight, and smoking. A person with PD who has osteoporosis is more likely to break a bone if they fall.
