Patient Story Michael’s Nibs Story
After a traumatic brain injury and a stroke, Michael was told he had reached his limit on what he could do. This was not something he and his partner, Jason, would accept. Thats when research led them to the Johns Hopkins Noninvasive Brain Stimulation program that helped set Michael on a path to recovery.
Noninvasive Brain Stimulation Program Main Menu
The noninvasive brain stimulation program at Johns Hopkins is one of the few programs of its kind in the country. Run by recognized experts in the field of neurologic rehabilitation and motor learning with more than 20 years of experience in NIBS, our program offers different forms of brain stimulation techniques paired with evidence-based rehabilitation to help treat a variety of neurological conditions and movement disorders.
Transcranial Magnetic Stimulation Safety In Parkinsons Disease Population
From 211 studies published in PubMed regarding the use of TMS in Parkinsons disease patients from 1993 to October 2017, the most common adverse events were scalp pain and headache. Most of these happened during high frequency rTMS sessions. Other less commonly reported AEs in PD include neck pain, tinnitus, and facial twitching. One study reported subclinical worsening of complex and preparatory movement as measured by spiral drawing impairment in patients after rTMS and worsening of resting tremor in one patient . Rare AEs possibly related to TMS reported were transient fatigue, mild transient visual hallucinations, and transient hypotension . One study reported a subject who experienced worsening in pre-existing lower back pain . In our neurostimulation lab, we had one report of mild transient low mood and one serious AE represented by an ischemic stroke. The ischemic stroke event was due to carotid disease and was deemed unrelated to the study, though . As an important note, to date, there are no reports of seizures induced by TMS among Parkinsons disease patients.
| Study |
|---|
Also Check: How Do You Check For Parkinson’s
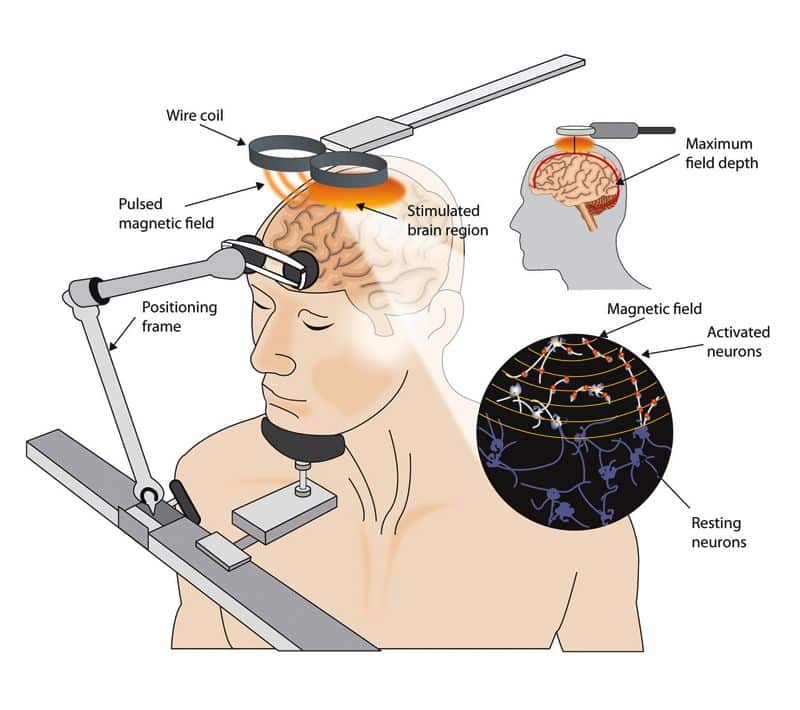
Transcranial Deep Brain Stimulation
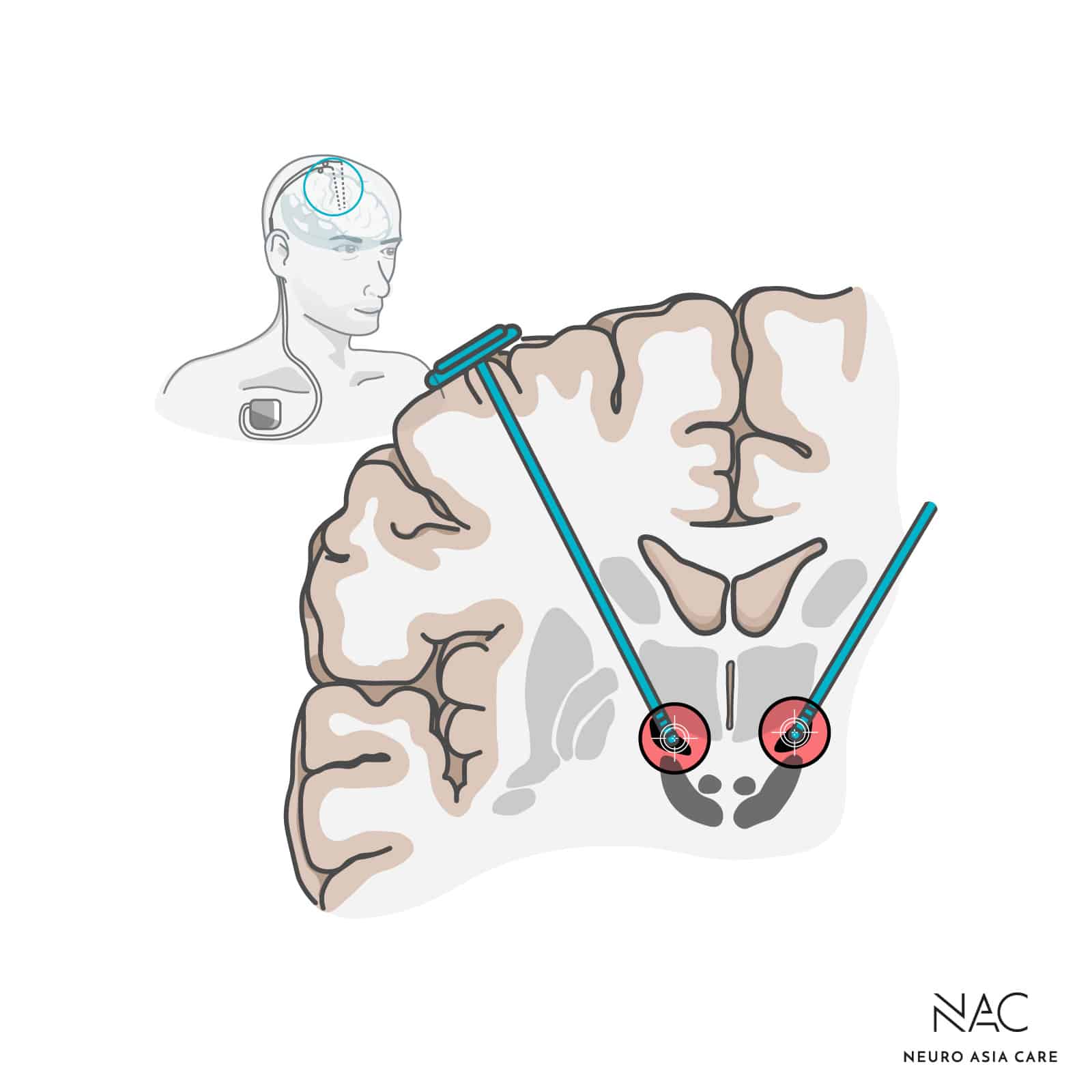
When the medication to treat Parkinsons disease symptoms like stiffness, slowness and tremors stops working, some people turn to deep brain stimulation. The procedure requires implanting electrodes deep in the basal ganglia region of the brain to deliver electrical pulses encouraging neurons to fire in a particular pattern.
Although the surgery is effective, its too risky for many older people with Parkinsons who have other serious health conditions.
At McGill University, neuroscientist Matthew Krause is studying a way to deliver electrical stimulation to the same region of the brain, without the need for surgery.
Krause, a research associate, is testing transcranial electrical stimulation. This method involves attaching electrodes to peoples scalps, through a tight-fitting cap, and creating an electrical field. A small battery-powered device then delivers the electrical charge to the electrodes. It creates a tingling feeling on the scalp and an electrical field that interacts with the brains own electrical activity.
Positioning the electrodes precisely places will be critical to the methods success, Krause says.
Over the last two years, weve shown we can change how neurons fire with this transcranial stimulation.
What were trying to figure out how to set it up correctly to hit the kind of same deep brain structures a surgeon would target, but without drilling into your head.
Understanding The Science Behind Neurobiomedicine And Our Approach To Helping You Restore Proper Function To Ultimately Help You Feel Better Look Better And Recover Your Health
Dr. Farleys Neurobiomedicine Health System can easily be understood when applied to the science of Translational Medicine, Psychosomatic Medicine and Somatopsychic Medicine as described from the National Institutes of Health. Please to learn more about Translational Medicine, Psychosomatic Medicine, Somatopsychic Medicine. Allopathic Medicine and even Integrative Medicine asks, Whats the diagnosis. Neuro-Biomedicine asks, Why you are personally having this happen?, and, What are your specific multifactorial causes?
Most doctors offices rely on outdated protocols that are 17-20 years behind the basic scientific research. The reason for this is lack of initiative by most doctors, and for medical legal reasons, they will not deviate from typical protocols even when they are outdated and produce terrible results for patients. The focus is not on the individual patient and their unique requirements, instead, the patient is literally pushed from office to office with the goal to just move the responsibility to another doctor or office . We do not treat any disease, instead we focus on your functional neuro-metabolic deficits. We will fight for you and your health! We will provide new possibilities and potential for greater healABILITY, greater depth of understanding, more compassionate listening, and ultimately, superior results aimed at restoring proper function. This, in turn, can have profound and positive improvements for the patients that qualify.
Don’t Miss: Does Parkinson’s Cause Muscle Wasting
What Is Brain Stimulation Used For
Several medical fields recognize the positive effects of brain stimulation. As rehabilitation physicians, we use this approach to help our patients improve a variety of brain functions affected by conditions such as:
- Language and communication disorders
- Movement disorders and involuntary muscle contractions
- Voice disorders
- Balance and coordination disorders
- Psychiatric conditions, including medication-resistant depression
The 8 Hidden Causes Your Doctor Will Not Tell You About Your Parkinsons Condition
The word Parkinsons can send a shiver down anyones spine with the impending fear of total neuro-degeneration and future disability, both mentally and physically.
The real question is.do you even have Parkinsons disease? Have you been told its Parkinsonian syndrome, multiple systems atrophy, essential tremor, or cerebellar ataxia? Or some other neurological problem? Either way, you need to find answers as to why your brain is deteriorating and degenerating so you can have a plan to stop this from worsening and possibly reverse some of these symptoms.
Many Parkinsons patients are diagnosed very late, when in fact early soft signs were apparent 10 to 30 years prior to the diagnosis.
Dr. Russell Blaylock, the renowned Neuro-Surgeon, states that the drug mainstay treatment that most patients will receive will almost guarantee they will get worse in 2-5 years, and it even appears to speed the deterioration! Get worse and speed the deterioration doesnot sound like great odds.
In our office we have identified 8 hidden root functional causes of trans-neuronal degeneration/brain degeneration that must be accurately measured to get a proper root functional cause diagnosis. Once we have an accurate root functional cause diagnosis, we can then design a custom treatment plan aimed at getting you lasting resultsto prevent further decline and restore function for many patients that qualify.
Read Also: Is Lewy Body Dementia The Same As Parkinson’s
Standardized Test Prep In Chicago Il
Standardized tests can be exceptionally difficult to prepare for independently. The lack of a structured test preparation plan often results in students being ill-prepared on the day of the exam and oftentimes feeling highly anxious. This can significantly hinder their ability to perform at a level commensurate with their abilities.
CSLC offers individualized test preparation plans that meet the unique needs of each student. We offer short and long-term test prep that takes into consideration the students academic and cognitive strengths and weaknesses, personal interests, and their preferred learning style. Test prep plans consist of both one-on-one sessions with an experienced test prep specialist and manageable homework assignments to be completed between sessions. This allows us to maximize the time spent during the sessions and to continually evaluate the students needs on a week by week basis. Students are explicitly taught strategies to help them tackle any and all content areas so they develop not only the requisite skills but also the confidence to perform at a high level.
Individualized test prep is available for:
MAP
How Your Support Made This Research Project Possible
Krause hopes this pilot project grant will help him launch an independent research career.
Parkinson Canadas funding for early-stage project is super helpful and really fills a gap that needs to be filled, he said.
No one is going to give us $10 million to spend on an idea we just had, but the fact Parkinson Canada was willing to look outside an established Parkinson research group was awesome. Thats going to be the key to solving these problems, is to look at people with a lot of different perspectives.
Using his pilot data from this project, Krause hopes to be able to attract other larger grants in the future.
Don’t Miss: How Does Dbs Work For Parkinson’s
Transcranial Electrical Stimulation Combined With Physical Or Cognitive Training
Motor and cognitive training can effectively ameliorate PD symptoms . Hence it might be possible to harvest the benefits of training and tES by combining these interventions.
In PD-MCI patients, tDCS combined with physical training showed steady cognitive improvements, but no significant additional effects of tDCS was found . In line with this finding, Fernández-Lago et al. found that after a single 20 min session of active tDCS stimulation with treadmill walking training, there was no enhancement of tDCS toward sole treadmill walking training .
In contrast, in another sham-controlled, double-blind crossover study, Kaski et al. applied tDCS at M1 and the premotor cortex, and together with physical training, PD patients were found to have improved gait and balance performance . Another study that combined 30 min of aerobic exercise with anodal tDCS targeted at the prefrontal cortex revealed a positive impact of this combination on PFC activity, gait, and cognition .
Outlook For Closed Loop Transcranial Electrical Stimulation
Although closed-loop tES studies toward PD are few, adaptive stimulation schemes have gained vast attention since they can deliver individual- or circumstance-specific modulation. Self-adaptive individualized closed-loop scheme can achieve higher efficacy and closed-loop tES schemes in the future might also be able to automatically switch on when symptoms occur, like closed-loop DBS.
Another serious technical problem for closed loop tES is the time delay between detection of changes in brain conditions and the response to stimulus. For symptoms with a short provoking duration, the time delay in response might just miss the period of symptoms and become ineffective. Future studies might employ machine learning to predict the occurrence of symptoms so that more precise stimulation could be provided. In addition, using a brain machine interface can provide a quicker stimulation response. For example, in a chronic pain study that used BMI in mice to monitor and stimulate the brain, the time delay between characteristics detected and stimulation response was minimized thus, the pain could be released even when recognizing acute pain signals .
Many studies have proposed numerous novel adaptive tACS and tDCS systems that proved to be safe and tolerable in healthy people . Building on these results, investigators could adopt those technologies in future closed loop tES studies in clinical PD populations.
Don’t Miss: Can You Prevent Parkinson’s
An Overview Of Noninvasive Brain Stimulation: Basic Principles And Clinical Applications
Published online by Cambridge University Press: 09 July 2021
- Department of Neurology, National Institute of Mental Health and Neurosciences, Bengaluru, India
- Kambhampati Mrudula
- Department of Neurophysiology, National Institute of Mental Health and Neurosciences, Bengaluru, India
- Sai Sreevalli Sreepada
- Department of Neurophysiology, National Institute of Mental Health and Neurosciences, Bengaluru, India
- Talakad Narsappa Sathyaprabha
- Department of Neurophysiology, National Institute of Mental Health and Neurosciences, Bengaluru, India
- Pramod Kumar Pal
- Department of Neurology, National Institute of Mental Health and Neurosciences, Bengaluru, India
- Robert Chen
- Affiliation:Division of Neurology, Department of Medicine, Division of Brain, Imaging and Behaviour, Krembil Research Institute, University of Toronto, University Health Network, Toronto, Ontario, Canada
- Kaviraja Udupa*
- Department of Neurophysiology, National Institute of Mental Health and Neurosciences, Bengaluru, India
- *
- Correspondence to: Kaviraja Udupa, Department of Neurophysiology, National Institute of Mental Health and Neuro Sciences , Hosur Road, Bengaluru, 560 029, India. Emails:
Transcranial Magnetic Stimulation General Safety
Different side effects resulting from the application of TMS have been reported in the literature. The international safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research have listed them according to their respective frequency. Common side effects include transient headache, local pain, neck pain, toothache, and paresthesia. Pain duration is usually limited, lasting up to few hours after the session, and it can be commonly relieved with acetaminophen or other over-the-counter medications. Less common adverse effects include transient hearing changes, transient cognitive/neuropsychological changes, syncope , and transient acute hypomania . Rare adverse effects reported include changes in blood levels of thyroid stimulating hormone and lactate, and seizures. Seizure activity has been reported mostly with high-frequency rTMS. TMS-induced seizures are self-limited and are not reported to have permanent sequelae. High frequency TMS has 1.4% crude risk estimate of inducing seizures in epileptic patients and less than 1% in non-epileptic subjects . There is a theoretical risk of inducing currents in electrical circuits when TMS is delivered in close proximity of electric devices which can cause malfunction of these devices.
Also Check: Does Parkinson’s Affect Balance
Closed Loop Transcranial Electrical Stimulation
It is generally accepted that discrepancies in effects can emerge between individuals when receiving identical stimulation. Similarly, several studies have witnessed deviations in neuronal feedback between different circumstances undergone by the same subject. To date, most tES research on PD has focused on open-loop schemes, providing constant predefined stimulation during the whole experimental process. However, due to these irremovable inter- and intra-subject variabilities, side effects, and low effect sizes may occur during clinical applications . Therefore, closed loop tES, which is self-adaptive toward changes in brain activity, Therefore, closed loop tES has become a hot topic.
Closed loop tES can provide self-adaptive stimulation according to the feedback of brain activity, forming a feedback-control close loop between input and output signals. To be more specific, when a predefined signal is detected by the sensor, closed loop system should immediately receive the feedback from the sensor and select the corresponding stimulation parameters, then pass to the stimulator to provide real-time control.
Ideally, optimized closed-loop tES should be able to recognize diverse circumstances and select symptom-specific tES parameters, in which case the specificity of stimulation would be improved, like methodology discussed above against rest tremor.
Transcranial Alternating Current Stimulation
Transcranial alternating current stimulation provides a sinusoidal external current stimulation that could either synchronize or desynchronize with the internal cortical rhythm . Dissimilar to tDCS, tACS has more viable parameters, such as amplitude, frequency, and phase. Hence, tACS is capable of specifically correcting natural brain oscillations back to normal.
Parkinsonâs disease patients suffer from pathological changes in internal brain oscillation frequency ranges. Higher theta , delta activities and lower alpha , beta activities in the basal ganglia were detected in PD patients . Additionally, PD patients also exhibit a reduced power of gamma band oscillation as well as deviated task-specific neuronal oscillation activity .
Additionally, tACS can be applied to probe and detect the causal relationship between behavior and neuron activity. In a randomized crossover tACS study, the associations between bradykinesia and abnormally altered beta/gamma oscillations in primary motor cortex were exposed when 1 mA tACS at 20 Hz or 7 Hz was delivered to patients. The stimulation electrode was centered over the first dorsal interosseous hotspot, while the return electrode was centered over the PZ according to the EEG 10â20 system. As a result, the increased beta power led to aggravated bradykinesia, while gamma synchronization entrained by tACS mitigated these symptoms .
Don’t Miss: Parkinson’s Disease Self Care
Potential Applications And Therapeutic Effects Of Nibs In Pd
There has been cumulative evidence supporting beneficial effects of TMS and tDCS in PD. However, several limitations have obscured the evidence-based generalizability of these results. Main limitations are wide methodological heterogeneity in study designs and exploratory designs with small sample sizes in the majority of the studies. As TMS research is significantly more advanced in terms of number of studies and Class I multicenter initiatives, TMS and tDCS therapeutic evidence will be revised separately.
Transcranial Pulsed Current Stimulation
Different from conventional tDCS, tPCS provides discontinuous direct current interrupted by either short or long periodical inter-pulse intervals , thus adding two additional parameters: inter-pulse intervals and pulse durations. Although phosphene might also be induced by tPCS, the overall tolerability toward tPCS is better than tDCS in healthy subjects, with a significantly reduced feeling of itching, tingling, and eye flashing .
In a Parkinsonian study, a combined tPCS and treadmill strategy was applied for 10 PD freezing of gait patients, with both pulse duration and inter-pulse interval of tPCS being 33.3 μs. The tPCS targeted M1 provided 20 min of stimulation with or without concurrent treadmill training. The gait speed and gait amplitude, however, were found to be improved after a single tPCS session but not in the combined group or treadmill alone group . However, this study did not include sham tPCS as a placebo control, and the reliability of its results was therefore dented. Further studies should take place to further assess the efficacy of tPCS toward PD.
There was a study toward healthy population implicated that the duration of tPCS was not aligned with the lasting time of aftereffects . Thus, the non-linear effects of tPCS together with its unclear mechanisms complicate the process of selecting proper tPCS parameters. Consequently, few PD studies have focused on tPCS.
Also Check: What Are The Five Stages Of Parkinson’s
Demographics Of Studies Using Rtms
Participant characteristics
Of the 33 included studies, 24 studies used rTMS . The mean age of participants in these studies was 64±3.8 years. Sample sizes ranged from eight to 98 participants and 58% of the total sample was male. The average disease duration for all 24 studies was 8±3.7 years and included disease severity that ranged from mild to moderate . Additionally, 13 out of the 24 rTMS studies included participants that were classified as severe ,,,,,,,,,,,,. The rTMS intervention was primarily performed ON medication,,,,,,,,,,,,,,,,,, with 5 studies applying rTMS OFF medication,,,,.
