Other Symptoms That May Contribute To Weight Loss In Pd:
- People with difficulty swallowing associated with PD will typically slow down their eating and reduce their consumption in an attempt to eat without coughing or choking.
- PD often causes slowed transit of food through the gut which can impact absorption and cause weight loss
- Mobility issues and tremors may impede the ability to buy groceries, prepare meals, and eat, all contributing to reduced food intake.
Relative Motor Unit Activation
Surface electromyography was used to determine the magnitude of quadriceps neural activation required to perform a sit-to-stand task, which we have published previously . sEMG electrodes are placed over the muscle bellies of vastus lateralis , rectus femoris , and vastus medialis , and knee joint angle is monitored by an electrogoniometer . Raw sEMG is collected at 1,000 Hz and knee angle at 500 Hz and analyzed via Biometrics DataLink software version 2.00. Maximal voluntary knee extension isometric contraction is first assessed on a knee extension dynamometer via 3 × 5-s contractions separated by 1-min rest. The contraction yielding peak torque is used to quantify maximum voluntary quadriceps motor unit activation . The sit-to-stand is then performed from a standard bench height with arms crossed for three repetitions at a slow, controlled cadence using an audiovisual metronome.
Effects Of Clinical Variables On Core Muscle Fatty Infiltration In Pd Patients
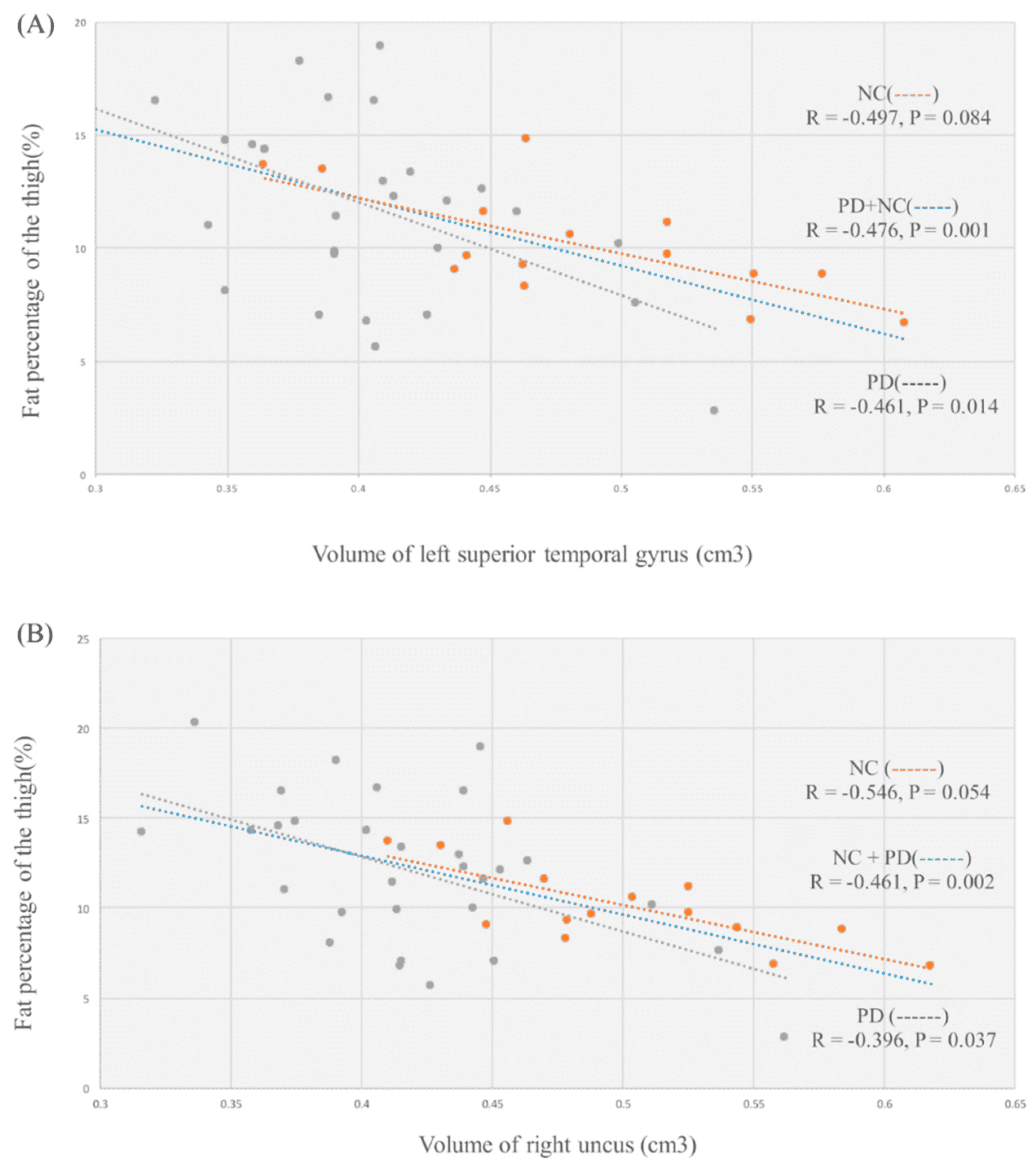
To verify the cause and predictive factor of fatty infiltration in PD patients, we used two statistical methods: partial correlation analysis and linear regression analysis. Prior to those, VBM was used to measure the total and regional brain volume difference between PD patients and healthy volunteers. The results indicate that PD patients had globally decreased gray matter volume, especially in left superior temporal gyrus, right uncus, and left inferior temporal gyrus compared to healthy controls. This is indeed consistent with previous studies reporting that physical frailty and sarcopenia are linked to brain structure changes , suggesting the role of the central nervous system in the pathophysiology of physical frailty . Partial correlation analysis revealed the gray matter volume reductions in specific regions, such as the uncus and superior temporal gyrus, were significantly associated with fatty infiltration in PD patients. Further linear regression analysis revealed that aside from volume reduction in those specific regions, female gender and longer disease duration were factors predictive of core muscle fatty infiltration in patients with PD. Of note, disease progression may affect both muscle loss and brain damage. Although this study revealed correlations between fat infiltration of core muscle and grey matter atrophy, the specific cause and effect relationship remains unclear.
Recommended Reading: What Medicine Is Used For Parkinson’s Disease
How To Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Read Also: How Is Parkinsons Disease Associated With Headaches
To Prevent Falls Exercise
Exercise is the only intervention that significantly reduces a persons risk of falling, among older people without PD as well as people with Parkinsons. Research is beginning to show how exercise changes the brain for the better and can help people with PD gain back some of their automatic balance reflex.
In a study, Dr. Horak and her team asked participants with PD to stand on a quickly moving treadmill, until they began walking. Participants initially took too-small steps, but with one hour of practicing, they improved, taking bigger steps to stay balanced while walking.
Many kinds of exercise can improve a persons balance. Consider trying:
- Tai Chi: a moving meditation where movements involve shifting the bodys center of mass back and forth over the feet. Studies found fewer falls among people with PD who practiced Tai Chi three times a week.
- Dance: to dance tango, a person has to walk backward and sideways, take big steps and both follow and lead good ways for people with PD to practice balance control.
- Boxing: the rapid arm movements provide good balance training.
- Agility boot camp: completing different tasks in a series of stations can improve balance.
Tip: People with PD may have other medical issues that affect their ability to exercise, such as arthritis or neuropathy. Work with a physical therapist to find an exercise that suits your needs.
Read Also: Most Common Parkinsons Medications
Don’t Miss: How Do I Know I Have Parkinson’s Disease
Inclusion And Exclusion Criteria
Articles recording the EMG signal in individuals with PD during forward, straight line walking were included. Studies which focused on specific phases of walking such as turning, gait initiation and termination or a special type of walk such as backward walking or walking in the Timed Up and Go test were excluded. Studies that only analysed static standing, posture and tremor or specific gait events observed in PD such as freezing of gait were excluded. Studies involving groups with pathologies outside of PD were excluded. Dopaminergic studies and DBS studies were only included when the EMG signal during a walking task was reported. Only articles written in English were considered. Reviews, abstracts, cohort studies, case studies, editorials, commentaries, discussion papers, conference proceedings and studies lacking full text were excluded. Eligibility and inclusion were determined by three reviewers . Discrepancies were resolved through discussion resulting in a unanimous decision or a majority consensus.
Loss Of Balance And Falls In Parkinsons Disease
Losing your balance and preventing falls is part of daily life for those with Parkinsons disease. With time, almost every person suffers from postural instability, but you have some control over the severity of balance issues and the frequency of falls.
Parkinsons disease significantly affects gait. The motor symptoms of the disease, such as rigidity, freezing and changes in posture disrupt the sense of balance and can lead to falls.
Nearly two-thirds of people living with the disease have fallen in the past year, and half of these cases resulted in injuries. Fortunately, there are many resources that can help you improve your balance and prevent these falls.
Balance is the control of body weight distribution and is a normal reflex in people without Parkinsons disease. Several factors associated with Parkinsons disease contribute to a loss of balance and falls.
Loss of balance reflex
The degeneration of the grey nuclei neurons characteristic of Parkinsons disease causes a loss of balance. Posture control then becomes managed by the cerebral cortex, or the thinking part of our brain. Balance therefore becomes a conscious and voluntary process rather than an automatic reflex.
Any external disturbance while managing your balance can cause a loss of balance.
Don’t Miss: Does Parkinson’s Cause Muscle Weakness
Why Worry About Weight Loss Associated With Pd
Weight loss has been linked to a poorer quality of life and more rapid progression of PD. The reasons for this are two-fold. On the one hand, as outlined in the list above, weight loss can be a hallmark of advancing disease as it could be a consequence of more swallowing difficulties, worsened mobility, more impaired gut function etc.
On the other hand, having weight loss can further lead to poorer health. Inadequate food intake can contribute to malnutrition and vitamin deficiencies. Malnutrition can subsequently be the cause of increased susceptibility to infection, increased fatigue and increased frailty. The situation can spiral with more fatigue and frailty causing a further decrease in activity and function.
Osteoporosis, or porous and fragile bones, is more common in under-weight people since bone structure is dependent on weight-bearing. Since osteoporotic bones are more prone to fracture during a fall, this too can be a contributor to more disability and frailty. Bottom line is that it is important for your health to maintain a healthy weight.
The Role Of Nutrition In The Treatment Of Sarcopenia In Parkinson’s Disease: A Scoping Review
Published online by Cambridge University Press: 17 August 2021
- Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
- M. Ó. Breasail
- Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
- F.E. Lithander
- Affiliation:Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UKOlder People’s Unit, Royal United Hospitals Bath NHS Foundation Trust, Bath, UK
- E.J. Henderson
- Affiliation:Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UKOlder People’s Unit, Royal United Hospitals Bath NHS Foundation Trust, Bath, UK
Don’t Miss: How Do You Find Out If You Have Parkinson Disease
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsonâs. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Read Also: Cleveland Clinic Parkinsonâs Bicycle Study 2017
How Can I Help Myself
You will need to try a variety of sensory tricks to see what works for you as dystonia affects everyone differently.
Spasms may be reduced by touching the affected part of the body either before or during any movement known to trigger dystonia. Although this may not prevent or stop a spasm, touching can distract or trick the brain and reduce the length and intensity of a muscle contraction.
Simple massage exerting pressure on the foot, or the use of a hot water bottle or heated pad can also help, as can movement and exercise â see Coping Strategiesâ Tips & Tricks.
For eye spasms, some people find lying down, singing, yawning, laughing, chewing, putting pressure on the eyebrows or just talking can help. Spasms in the vocal cords may respond to yawning or sneezing.
Simply relaxing may also help so try taking a bath, having a massage or a calming activity such as yoga.
Read Also: How Do You Know When Parkinson’s Is Getting Worse
Tips For Achieving A Healthy Weight
Whether you wish to gain weight or lose it, diet and exercise are key.
- Eat a balanced diet, with a variety of foods from all the food groups: whole grains, vegetables, fruits, dairy products and sources of protein like meat, fish and beans.
- Exercise helps keep people mobile and strong and can improve mood. Being active stimulates appetite and burns calories.
Weight Loss In Parkinson’s Disease

If you have Parkinson’s disease, you may feel that one of the few benefits of PD is weight loss, but that’s not necessarily true.
Weight loss may be a “red flag” indicating more severe disease since those who experience weight loss have been found to have a faster worsening of their disease statistically. There are many theories about the origin of weight loss for people with Parkinson’s disease. Some believe a loss of smell, which can affect appetite, leads to weight loss as well as increased energy expenditure and fat burning due to tremors and dyskinesias, which are involuntary movements induced by levodopa.
Don’t Miss: How To Avoid Getting Parkinson’s
Limitations Of Reviewed Studies
A small selection of superficial lower limb muscles was assessed during walking in individuals with PD with certain muscle groups studied less. Information about the contribution of muscles to movement is necessary for understanding compensatory mechanisms resulting in impaired gait and dynamic postural control and for developing interventions. Only one study recorded the hip adductors, a muscle group with a cross-sectional area , which relates to muscle force, comparable to the CSA of the quadriceps group, and almost three times greater than the CSA of the hamstrings. This creates a vacuum in our knowledge of motor activity during walking in PD particularly given that mediolateral sway and instability are greater in individuals with PD. The reviewed studies reported group differences in a wide range of EMG parameters including temporal information , amplitude , coactivation indices, synergies, symmetry/variability indices and nonlinear indices. However, spectral characteristics of the EMG signals and intermuscular coherence, which may provide information about motor unit recruitment and neuronal networks controlling muscle activity, were not analysed.
Remaining In Control Over The Body
The subthemes controlling equilibrium and ability to stand, walk, and perform activities without falling tie together to form this main theme. When asked to describe how they perceived balance, participants described the concept of balance as being related to the ability to control ones equilibrium.
To keep the body in an equal weight so that you dont fall. That must be what balance is, that things are weighted equally in some way, so that you dont weigh over more to 1 side.
Figure 1
Overview of the analytical process from subthemes to overarching theme.
This control was described as a combination of automatic and voluntary processes entailing abilities such as coordination of body parts. Having equilibrium was also described in terms of being in an effortless state whereby you could carry yourself freely and not have to think ahead and prepare before challenging movements.
Balance, that to me is like being able to control your, your body, control your feet, being able to do things freely, walk normallystopping. Balance to me is a state where my symptoms are fairly perfectly alleviated, where the body is like balanced and walking works and I can lift things. Then I am in balance. Or well, hopefully.
Well, that you can do things like any normal person can do without like losing your balance. Thats the way it is. Like you can stand on 1 leg, be able to run, be able to walk, cycle.
Dont Miss: Can Parkinsons Cause Hip Pain
Read Also: Can Parkinson’s Cause Headaches
The Prevalence Of Sarcopenia In Parkinsons Disease And Related Disorders
A. Hart, F. Barker, A. Sayer, A. Granic, A. Yarnall
Category:Parkinson’s Disease: Non-Motor Symptoms
Objective: To systematically review the prevalence of sarcopenia in Parkinsons disease and atypical parkinsonian syndromes , how prevalence differs with PD stage and between PD and aPS.
Background: Sarcopenia is characterised by loss of strength and skeletal muscle mass. Like PD, its prevalence increases with age and has important health implications. There is evidence that sarcopenia is more prevalent in PD than in age matched cohorts. Shared features of pathogenesis include IL6 driven neuroinflammation and mitochondrial dysfunction. However the degree to which sarcopenia and parkinsonian disorders co-occur or the extent to which sarcopenia correlates with disease stage is unknown.
Method: Predefined literature search strategies were used on MEDLINE, EMBASE, Scopus and Web of Science. Studies conducted in people with PD or aPS reporting on the prevalence of sarcopenia or those that provided enough data to compute this using validated sarcopenia definitions were included. Risk of bias was assessed using the AXIS tool.
Sarcopenia is a prevalent and important issue in parkinsonian disorders. Probable sarcopenia, defined by muscle weakness, is especially common. Recognition of this should prompt clinical testing and provision of appropriate interventions to minimise negative clinical outcomes associated with movement disorders being compounded by muscle weakness.
Mov Disord.
What Are The Different Types Of Muscular Dystrophy
Muscular dystrophy is a group of inherited diseases characterized by weakness and wasting away of muscle tissue, with or without the breakdown of nerve tissue. There are 9 types of muscular dystrophy, with each type involving an eventual loss of strength, increasing disability, and possible deformity.
The most well known of the muscular dystrophies is Duchenne muscular dystrophy , followed by Becker muscular dystrophy .
Listed below are the 9 different types of muscular dystrophy. Each type differs in the muscles affected, the age of onset, and its rate of progression. Some types are named for the affected muscles, including the following:
Don’t Miss: What Is Parkinson’s Dementia
Loss Of Muscle Mass Symptoms
Muscles are vital to everyday function, and if you noticeably lose muscle mass especially without knowing why it can be frightening. Losing some muscle mass is expected as you age. However, losing muscle mass rapidly, or atrophy, especially in the context of other symptoms, can indicate an underlying condition.
