Neuroinflammation In Pd Neurotoxin Models
Epidemiological evidence suggests there is a significant environmental component to sporadic PD. As a result, efforts to identify environmental PD toxins have yielded several chemicals that cause Parkinsonism in rodents and primates. Considerable evidence suggests that these compounds work by inducing oxidative damage in target cells. Research has also found that these PD toxins exert a robust inflammatory response and that anti-inflammatory therapies are protective in animal models. This supports the theory that DA neurons are lost in PD due to an especially high susceptibility to oxidative damage which may be the result of, at least in part, inflammatory response. We will now discuss three of these toxins in the context of neuroinflammation.
Adaptive Immunity: Activation Of Cell
The adaptive immune system shows specific responses against foreign antigens activating different T or B lymphocytes . The surveillance of homeostasis in the CNS is guaranteed by naïve and memory T cells . T cell infiltration has been discovered in post-mortem brain sections of PD patients . The analysis of T cell subsets in peripheral blood mononuclear cells of affected patients showed altered immune responses and a decrease in the overall number of lymphocytes, but not in their frequency . What is more, PD presents a particular immunological profile unseen in other neurological diseases , where increased numbers of memory T cells and a reduced quantity of naïve T cells have been registered . As well, low CD4+:CD8+ ratio and a shift to more IFN- vs. IL-4-producing T cells have suggested the presence of cytotoxic T cell responses in PD patients .
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
You May Like: Parkinson’s Awareness Ribbon
Evidence Of Neuroinflammation In Parkinsons Disease
Post-mortem, epidemiological and imaging studies from patients, and also studies with animal models have highlighted the role of neuroinflammation in PD and raised the interesting possibility that chronic inflammation may act as a stressor environment that promotes the progressive degeneration of dopaminergic neurons1010 Tansey MG, Goldberg MS. Neuroinflammation in Parkinsons disease: its role in neuronal death and implications for therapeutic intervention. Neurobiol Dis. 2010 37:510-8. http://dx.doi.org/10.1016/j.nbd.2009.11.004.
Amyloid Nature Of Parkinsons Disease Fibrin
Previously, we have shown with ThT that the fibrin protein structure in PD can become amyloid in nature, due to mis-folding of the protein . It is well known that fibrinogen levels in PD is higher compared to healthy controls . In the current paper, we include two additional amyloid markers. Our results show enhanced amyloid-fluorescence as assessed by both AmyTracker 480 and 680 and this is confirmed by enhanced ThT fluorescent in our current PD samples. Our results suggest that in PD clots, fibrinogen polymerizes into a form with a greatly increased number of ß-sheets, reflecting amyloid formation. This important finding may describe a possible mechanism underlying some of the anomalous clotting formation and coagulopathies occurring in PD. It further emphasizes the systemic nature of PD, demonstrating pathological changes beyond the brain and extending to the circulation. Amyloid fibrin has also been observed in other diseases associated with inflammation and with known hematological abnormalities, including Type 2 Diabetes and
Read Also: Parkinson Symptoms Come And Go
Scanning Electron Microscopy Of Whole Blood Smears
Whole Blood smears were prepared by placing 10 L WB of each of the samples on cover slips. Samples were washed with GibcoTM PBS, pH 7.4 before fixing with 4% paraformaldehyde for a minimum of 30 min. Once fixed, samples were washed 3 × 3 min with PBS followed by a second 30-min fixation step in 1% osmium tetroxide . A final 3 × 3 min PBS wash step was performed before samples were serially dehydrated in ethanol with a final 30-min dehydration step using hexamethyldisilazane ReagentPlus® . Samples were then carbon coated before being imaged on Zeiss MERLINTM field emission scanning microscope and micrographs were captured using the high resolution InLens capabilities at 1 kV.
Scanning Electron Microscopy Of Whole Blood
illustrates a representative SEM micrographs of platelets seen in WB smears. SEM analysis of WB smears of healthy controls usually show platelets as irregularly shaped cellular structures, with only slight pseudopodia formation due to contact activation with glass cover slips. This finding has previously been noted in various publications . In the PD sample, platelets showed substantial activation, spreading , as well as aggregation , suggesting that these results might be due to the increased inflammatory biomarkers and cytokines in circulation, that act as ligands to platelet receptors. Interactions with RBCs were also frequently noted .
Scanning electron microscopy of whole blood smears showing representative platelets from healthy individuals. Whole blood smears from PD individuals showing hyperactivated platelets. PD platelets agglutinating to RBCs PD platelet spreading and PD platelet aggregation .
Also Check: Parkinson’s Fatal
Parkinsons: Autoimmune Attack May Start Years Before Diagnosis
A new study adds to evidence that autoimmunity plays a role in the development of Parkinsons disease. The research also offers hope that early preventive treatment could offset the damage.
Parkinsons disease is a chronic, progressive disorder. Its characteristics tend to include tremor, rigidity, slowness of movement, and impaired balance.
Around 1 million people in the United States and 10 million people throughout the world have the disease.
Parkinsons results from a loss of nerve cells in a part of the brain called the substantia nigra. These cells produce dopamine, a chemical messenger, or neurotransmitter, involved in controlling movement.
Most people with Parkinsons are older than 50 when they receive the diagnosis, but some develop motor symptoms, involving problems with muscle control, at an earlier age.
Years before motor symptoms arise, other symptoms of Parkinsons can appear, including a reduced sense of smell, constipation, mood changes, and REM sleep behavior disorder, which involves physically acting out dreams.
The existence of these prediagnostic symptoms suggests that damage to dopamine-producing nerve cells begins long before the person experiences trouble with movement.
A new study spearheaded by researchers from the La Jolla Institute for Immunology , in California adds to evidence that the immune system may be responsible for the damage to nerve cells.
Intranigral Intrastriatal And Intraventricular Lps
In 1998, Castaño et al. reported that intranigral injection of LPS led to SN DA neuron loss at 15 and 21 days postinjection. Subsequent studies found that intranigral LPS injection resulted in microglial activation, proinflammatory cytokine production that include IL-6, IL-1 , TNF-, and NO. Interestingly, a solitary injection of LPS intranigrally caused a specific DA neuron loss with no observed effect on serotoninergic or GABAergic neurons and this loss was detected one year following injection. The specificity to DA neuron loss could be attributed to an increased susceptibility of these neurons to oxidative damage. Iravani et al. reported that 24h following intranigral LPS injection astrogliosis and heightened expression of proinflammatory cytokines that was correlated with elevated levels of glial derived neurotrophic factor was observed. The authors propose that GDNF may serve as a protective factor in a proinflammatory environment. This notion has been supported by subsequent studies showing protective effects of GDNF on DA neurons in oxidizing environments., These results suggest that robust inflammatory response induces specific loss of SN DA neurons and that intrinsic mechanisms exist to mitigate neuronal loss during these events.
You May Like: What Are The Four Cardinal Signs Of Parkinson’s Disease
Ethical Clearance And Consent
The study received ethical clearance from the Health Research Ethics Committee of Stellenbosch University, South Africa and the Health Department of Western Cape research number . Written informed consent was obtained from all participants followed by whole blood sampling. All participants received a unique number that was used to guarantee discretion throughout this study. All investigators were certified in Good Clinical Practice and ethical codes of conduct.
Antiinflammatory Therapies In Pd
While evidence strongly suggests that inflammation plays a major role in the etiology of a number of different forms of PD, emerging evidence also demonstrates that therapies used to lessen inflammation, including those directed against immune cells or inflammatory mediators, can play a positive role in halting the degeneration of DA neurons in several models of PD. Many studies suggest that inflammatory mediators such as TNF, PGE2, NO, free radicals, and other immune mediators play a role in the pathogenesis of PD and degeneration of dopamineproducing neurons, and that the use of specific reagents that target these mediators, inhibition of cellular signaling mechanisms that regulate the production of these mediators, or the use of neurotrophic factors that help protect against the neurotoxicity induced by these mediators hold significant promise as therapeutic treatments for PD. In addition, epidemiological and observational studies already suggest that use of antiinflammatory drugs lower the risk of developing PD .
LPS induced mice and mesencephalic culture
| Therapy |
|---|
7.2.2. Antiinflammatory cytokine therapies in PD
7.2.3. Regulatory Tcell therapy
7.2.4. Insulin as potent therapeutic agent for treatment in PD
7.2.5. Use of adrenergic receptor agonists as an antiinflammatory agent in the treatment of PD
7.2.6. Use of morphinanrelated antiinflammatory compounds in PD
7.2.7. Proinflammatory transcription factor, NFkB as a therapeutic target in PD
You May Like: Early Symptoms Of Parkinson’s In Adults
Connection Between Inflammatory Stimulus And Parkinson’s Disease Examined
- Date:
- American Physiological Society
- Summary:
- The precise cause of Parkinsons Disease is unknown, but there is consensus that an inflammatory event or episode is involved in the initiation of neurodegeneration. A new study has brought the understanding of inflammations role a step further.
Parkinson’s disease is a progressive degenerative disease affecting a person’s ability to coordinate and control their muscle movement. What starts out as a tremor in a finger will eventually lead to difficulty in writing and speaking, and ultimately the inability to walk without assistance. Since the 1950s research has shown that people with Parkinson’s have decreased levels of the chemical dopamine in their brains, which is involved in sending messages to the part of the brain that controls coordination and movement. Subsequent research has found that dopamine-generating cells, known as dopaminergic neurons, are also absent in a specific area of the brain in those with PD.
Methodology
Twelve male Sprague-Dawley rats were treated with intravenous LPS in saline, 12 control rats were treated with saline, and all were maintained for up to 48 hours before euthanasia and brain removal. Brains were removed from both groups at defined times, blood and other tests were conducted, and images of various sections of the brain, including the olfactory bulb, cortex and cerebellum, were taken using fluorescent microscopy.
Results and Conclusions
As a result, the researchers suggest:
Next Steps
Thromboelastography Cholesterol And Hba1c Levels And Ultrasensitive Crp
HbA1c levels were significantly increased in the PD sample with a notably dysregulated lipid profile . TEG results point to the fact that PD WB is hypercoagulable. TEG analysis exhibited significant differences in five of the groups of the assessed parameters. The PD group presented a significant increase in the initial rate of clot formation . Significant elevation in alpha angle suggests more cross-linking of fibrin fibers, and time to maximum rate of thrombus generation was decreased. These results have significance to our RgpA results that we discuss later.
Also Check: Can Parkinson’s Run In The Family
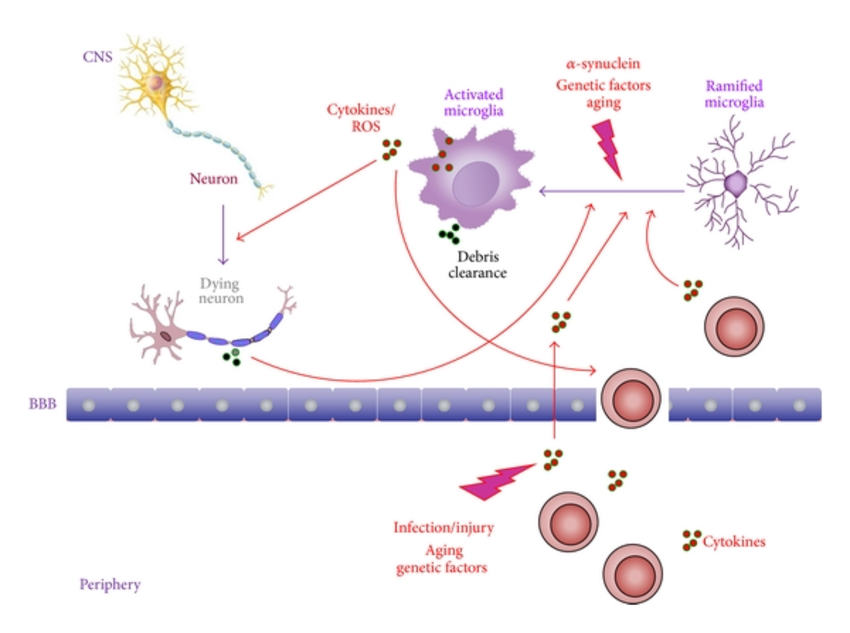
What Activates The Microglia
A key issue for understanding the role of innate inflammation in the CNS in the pathogenesis of PD is to discover what are the stimuli that lead to the activation of microglia, in particular, those that drive them to a phenotype that promotes neurodegeneration. Neuronal degeneration per se will lead to the generation of numerous molecules that may activate myeloid cells and release the inhibitory tone on microglia as discussed above. In vitro studies have shown that neuromelanin and -synuclein aggregates lead to activation of the microglia and the generation of potentially neurotoxic molecules. However, the mismatch between in vitro and in vivo experimental approaches seems to have attracted little critical appraisal despite the fact that the same issues pertain in a number of other protein misfolding diseases. The response of a cell of the macrophage lineage is critically dependent not only on the concentration of the stimulus but also the rate of change of the stimulus, any prior stimulation, and the local microenvironment. It seems very unlikely that a microglia cell will respond in the same manner to the slow accumulation of -synuclein aggregates or slow progressive release of neuromelanin as it will to the sudden addition of these agents to a culture plate, a microenvironment in which the microglia have already been acutely removed from the tonic inhibition provided by ligands expressed on the surrounding neurons in vivo.
Inflammation And Pd Models
There are several models of PD, both toxin based and gene based, used to study disease progression and/or therapeutic development. In many of these models, inflammatory mechanisms are reported to play roles in the pathogenesis and manifestation of the disease in various animal models. In the remainder of this chapter, we will focus on characterizing the inflammatory response seen in the various models.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
List Of Inflammatory Diseases
There is no cure for the coronavirus… But there is a defence.
It is well established that the death rate from the coronavirus is highest amongst the already sick, weak and elderly. In other words those with an already compromised immune system. So although there is no known current cure there certainly is a defence… strengthen your own immune system! Click here to learn more.
A comprehensive list of inflammatory diseases would run to over 100, each of which have high levels of inflammation in the connective tissues, or degeneration of these tissues. These include…
- Alzheimer’s
- arthritis , psoriatic arthritis)
- asthma
- Parkinson’s disease
- ulcerative colitis
Inflammation is the end result of long term oxidative stress. The stress can be caused by emotional or physical trauma, and nutritional or environmental pollutants. In most cases it is something of everything.
Interestingly the incidence of atherosclerosis, heart attack and stroke is greatly increased in RA, these are also due to oxidative stress.
The question is what has caused the oxidative stress. Food is a major culprit, sugar being the number one culprit as it causes glycation. Sugar in any form, ie starchy carbohydrates like potatoes, legumes, sweet fruit or root vegetables, sugar in drinks, sauces, tinned food etc., and in particular grains and anything made from them such as bread, cakes, biscuits, pasta etc. These all convert to glucose.
Physical or mental stress also causes oxidation.
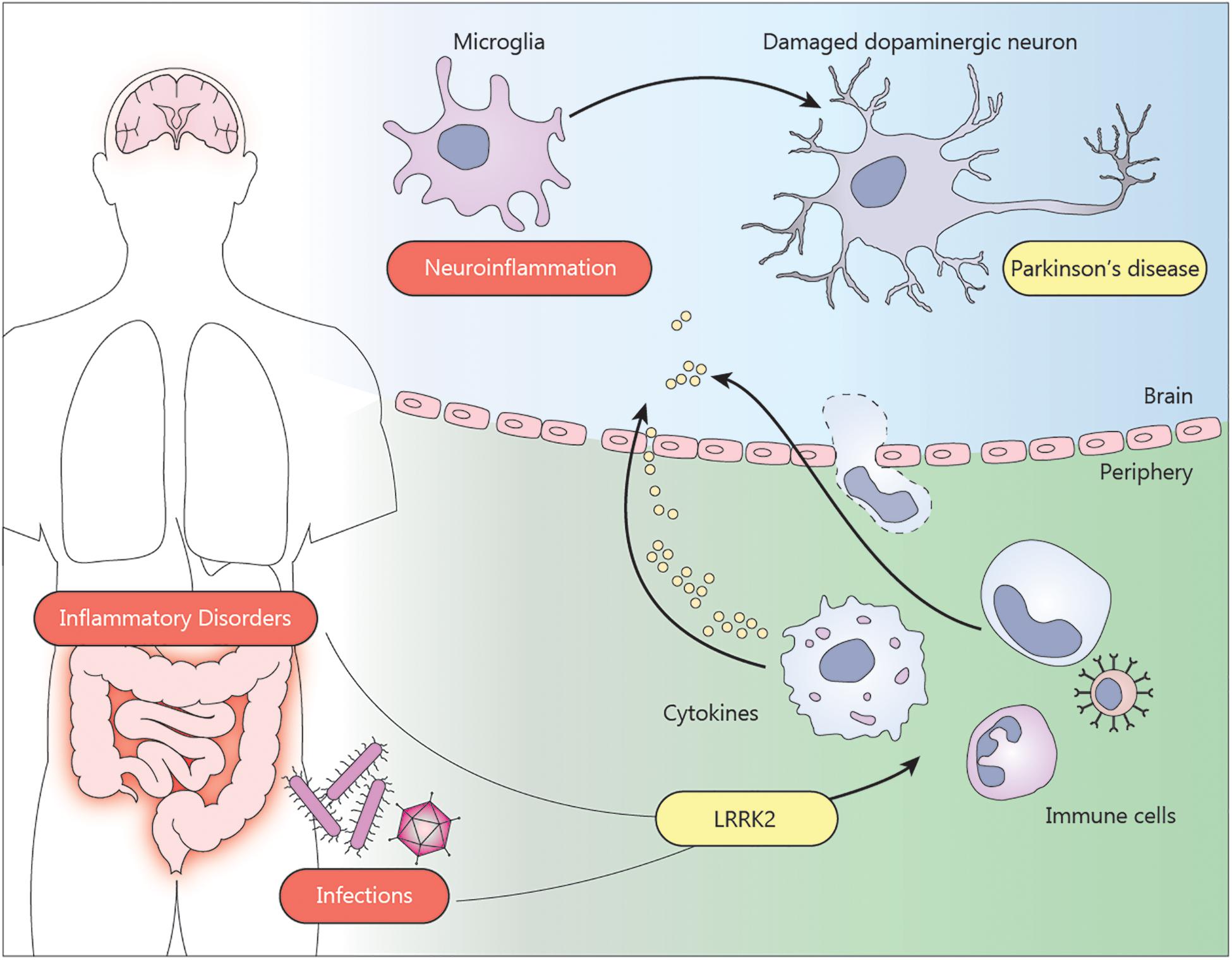
Inflammatory Bowel Diseases And Parkinsons Disease
Issue title: Special Issue: The Gut-Brain Axis in Parkinsons Disease Revisited
Guest editors: Teus van Laar
Article type: Review Article
Authors: Brudek, Tomasza b *
Affiliations: Research Laboratory for Stereology and Neuroscience, Copenhagen University Hospital, Bispebjerg-Frederiksberg Hospital, Copenhagen, Denmark | Copenhagen Center for Translational Research, Copenhagen University Hospital, Bispebjerg and Frederiksberg Hospital, Copenhagen, Denmark
Correspondence: Correspondence to: Tomasz Brudek, Research Laboratory for Stereology and Neuroscience, Copenhagen University Hospital, Bispebjerg-Frederiksberg Hospital, Nielsine Nielsens Vej 6B, building 11B, 2nd floor, DK-2400 Copenhagen NV, Denmark. Tel.: +45 38635600 E-mail: .
Keywords: Parkinsons disease, inflammatory bowel disease, Crohns disease, ulcerative colitis, enteric nervous system, brain-gut axis, gastrointestinal track inflammation, inflammation
DOI: 10.3233/JPD-191729
Journal: Journal of Parkinson’s Disease, vol. 9, no. s2, pp. S331-S344, 2019
Abstract
You May Like: Propranolol Increased Total Peripheral Resistance
The Presence Of Bacterial Inflammagens In Parkinsons Disease
P gingivalis has long been implicated in PD and periodontitis, and recently its protease was interrogated as a causative agent in AD, where the gingipain proteases was found in brain tissue from patients with AD . These researchers also correlated these gingipain quantities within the brain tissue to the extent of tau and amyloid- pathology. Furthermore, P. gingivalis has been found within atherosclerotic tissue of cardiovascular disease patients . Periodontal diseases are a well-known accompaniment to PD , however, the direct identification of P. gingivalis or its molecular signatures in circulation and/or brain tissue of PD patients has not previously been made.
These results are of particular importance when it is noted that bacterial involvement might play a role in both the development and even progression of PD, and specifically, circulating bacterial inflammagens such as LPS have been implicated . We have also suggested that LPS may both maintain systemic inflammation, as well as the disease etiology itself in PD . Indeed in 2018, we showed that LPS from E. coli could be identified with fluorescent LPS E. coli antibodies in clots of PD, type 2 diabetes and AD . There is therefore mounting evidence that PD might have a bacterial involvement, that in part drives the etiology of the condition through endotoxins as potent bacterial inducers of cytokines .
Brain Inflammation And Microglia Activation
Pivotal to the inflammatory cascades putatively leading to death of dopamine neurons in PD is microglia activation. Under physiological conditions microglia are resting or surveillant. In the rodent brain it has been shown that they are finely ramified and quite evenly distributed throughout the brain parenchyma, where they continually survey their microenvironment with mobile processes and protrusions . Microglia can move around because they contain high levels of the contractile protein actin and by doing so, at a given time, their tiny delicate processes contact about 3% of excitatory synapses in the brain . As a part of the innate immune system, microglia are able to sense neuron derived danger-associated molecular patterns resulting in microglia activation . Upon activation microglia become larger and thicker, showing a spheric shape . Activated microglia exists in several phenotypes, which probably represent a continuum from neuroprotective to neurotoxic phenotypes . When microglia are protective they usually take on phagocytotic properties, eating cellular debris and they secrete anti-inflammatory substances, e.g., interleukin- 10 and transforming growth factor . Toxic microglia secrete pro-inflammatory cytokines, such as IL-1, IL-6, interferon- , and tumor necrosis factor- , and they produce pro-inflammatory enzymes, such as nitrogen monoxide synthase and release nitrogen monoxide .
-Synuclein Can Activate Microglia
Read Also: Life Expectancy After Parkinson’s Diagnosis
