Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
I am a very active person, but deep fatigue must be addressed with rest. Taking a day to rest is not in my nature. It makes me feel like a sloth. Yet, when deep fatigue hits me, the best remedy is to do just that take the day off! I limit myself to one day of physical rest, very rarely two days . I also find that the mind must rest with the body. Getting the mind to a quiet place is the practice of meditation, in whatever form suits the moment. At the height of deep fatigue, meditation can be very difficult, but not impossible. At times, it has taken me four hours to quiet my mind and body to get rejuvenating rest.
But there is a caution here: Be wary of using rest as an excuse to procrastinate. In another column, Ill address the link of scenario looping to set-shifting issues and difficulty initiating new tasks. Basically, getting off the sofa can be problematic if I stay there too long. Perhaps this seems contradictory to my history as a highly active person, but that is the nature of PDs nonmotor effects. Once off the sofa, I make myself shift into a physical task, followed by a short rest and then some type of mental task. There is always some resistance to overcome to do this to get off the sofa but the rest is absolutely necessary to stop the deep fatigue.
Rem Sleep Behavioral Disorder
Rapid eye movement, or REM, sleep is a normal part of the sleep cycle when people dream. Usually the only part of the body that moves during REM is the eyes, thus the name.
- People with rapid eye movement sleep behavior disorder do not have the normal relaxation of the muscles during their dreams. Therefore, they act out their dreams during REM sleep.
- People with RBD may shout, kick their bed partner or grind their teeth. Sometimes, in moderate to severe RBD, people may have aggressive, violent behaviors, like getting out of bed and attacking their bed partner.
- About half of people with PD suffer from RBD. It may develop after or along with the disease, but in most cases, it precedes the PD diagnosis by five to 10 years.
RBD Treatment
- Consider making environmental adjustments to protect the person with RBD and bed partner from injury. This may include padding the floor, using bed rails or sleeping in separate rooms.
- Clonazepam has been shown in large case series to improve RBD in 80 to 90 percent of cases. The dose of clonazepam required is low, usually from 0.5 mg to 1.0 mg. The adverse effects of clonazepam include nocturnal confusion, daytime sedation, and exacerbation of obstructive sleep apnea, if present. It is in generic form and not expensive.
- Talk to your doctor about the over-the-counter sleep aid Melatonin. Doses up to 12 mg at night one hour before can improve RBD.
Tips For Better Sleep
- Keep a regular sleep schedule go to bed at the same time and get up at the same time.
- Choose your bedtime based on when you want to get up. Plan to spend seven to eight hours a night in bed.
- Make a bedtime routine for example, snack, bath, tooth-brushing, toileting and follow it every evening.
- Spend time outdoors and exercise every day, in the morning if possible. Avoid exercise after 8:00 p.m.
- If you cant get outdoors, consider light therapy sitting or working near a light therapy box, available at drug stores and department stores.
- If you nap, try to do so at the same time every day, for no more than an hour, and not after 3:00 p.m.
- Sleep in a cool dark place and use the bed only for sleeping and sexual activity.
- Do not read or watch television in bed.
- Use satin sheets and pajamas to make moving in bed easier.
- Minimize drinking liquids for three hours before bedtime to avoid frequent nighttime urination.
- Go to the bathroom immediately before retiring.
- Place a commode next to the bed, to minimize the effort, and light to get up during the night.
- Avoid:
- Alcohol, caffeine and other stimulants such as nicotine
- Heavy late-night meals
- Heavy exercise within six hours of bedtime
- Thoughts or discussions before bedtime about topics that cause anxiety, anger or frustration
- Clock watching
- Screen time television, phones, tablets one or two hours before bed.
Recommended Reading: Cardinal Symptoms Of Parkinson\’s Disease
Frequency And Characteristics Of Eds In Pd
Subjective and objective EDS were common in this PD population. Similar percentages were reported in previous studies , including those with unselected PD patients. As already reported in the literature , we did not find an association between EDS and age. Several studies have suggested a higher frequency of EDS in male PD patients . In our sample, however, no gender differences were found.
An association between EDS and SOREM has been reported. Healthy subjects with multiple SOREMs were sleepier than subjects with 1 or no SOREM. None of the 11 patients with MSL 5 min presented with SOREM. Because naps were terminated after 20 min , we do not report on the occurrence of SOREM in the rest of the patients.
Sleep-misperception was observed in 10 patients , which is similar to previous reports in which sleep-state misperception in association with MSLT naps was reported in up to 38% of patients with PD and in 45% of patients with EDS . In healthy subjects, sleep perception depends on sleep duration after a 4-min nap, only 50% of healthy controls confirmed they had fallen asleep . In a previous study, the patients with sleep misperception tended to underestimate their sleepiness in ESS . No specific characteristics of PD with sleep misperception were found in our series.
As already shown by others , ESS correlated significantly with MSL. This supports the use of ESS as a screening tool in clinical practice for EDS in PD patients.
Sleep: A Mind Guide To Parkinsons Disease
This 36-page booklet explains normal sleep patterns, the body clock, how much sleep we should get, challenges to sleeping well, tips for good sleep hygiene, and sleep in normal aging before discussing symptoms, diagnosis and treatment of sleep disorders, including insomnia, REM sleep behavior disorder, sleep apnea, restless leg syndrome, and daytime sleepiness.
Don’t Miss: Freddie Roach Illness
Trouble Staying Asleep Or Getting Restful Sleep
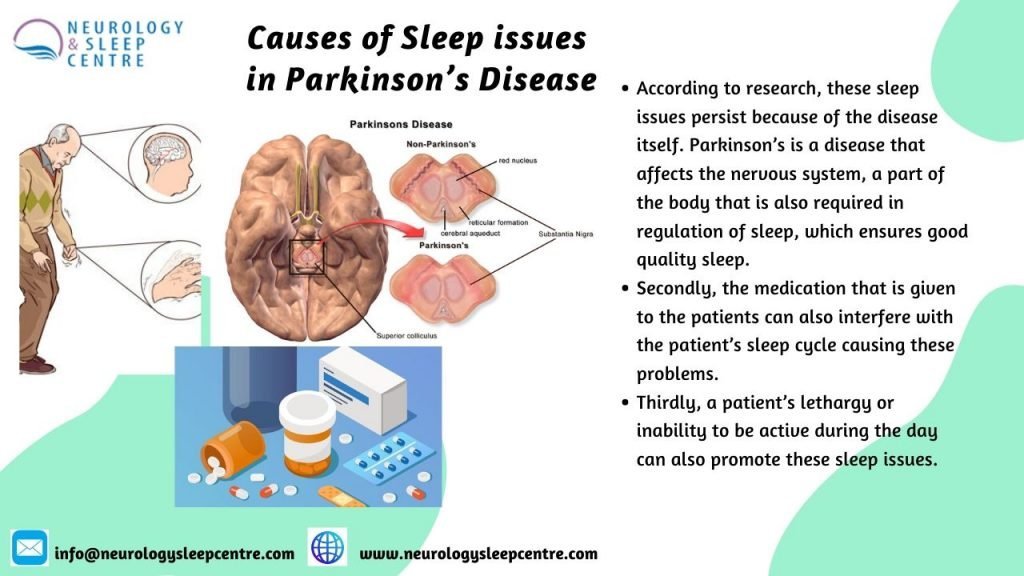
Some conditions, including Parkinsons disease, can interrupt sleep or make it less restful. Sleep fragmentation or interrupted sleep is one of the most common sleep complaints in Parkinsons patients. Poor sleep can lead to problems with attention and thinking, among other issues.
Several factors can lead to sleep interruptions in Parkinsons disease. These include the symptoms of the disease returning when medications wear off , frequent nighttime urination , hallucinations or altered dreams, and sleep apnea.
A large study of almost 3,200 patients found that sleep apnea was more common in people with Parkinsons than others.
Another study showed that women with sleep apnea may be at higher risk of getting Parkinsons disease.
Motor dysfunction of the laryngopharynx, the area where air and food pass through the throat, could also be involved in sleep apnea in Parkinsons disease patients, according to another study.
Sleep apnea can be treated with oral appliances or airway pressure devices such as a CPAP to keep the airways open. If these are unsuccessful, surgery might be an option.
REM sleep behavioral disorder, restless legs syndrome, and periodic limb movements in sleep are other issues that can lead to less restful or interrupted sleep. These disorders, which involve unwanted movements of the body, have a higher prevalence in Parkinsons patients and may have similar underlying causes.
Fatigue Sleep Difficulties And Restless Legs
Although Parkinsons is classified as a movement disorder, it can affect people in various different ways. Sometimes the non-movement symptoms can be more troublesome and can have a bigger impact on the daily life of someone living with Parkinsons.
Some of the more common non-movement symptoms of Parkinsons are:
- Fatigue
- Restless legs
Recommended Reading: Demographics Of Parkinsons Disease
Memory Or Thinking Problems
Having issues with thinking and processing things could mean your disease is progressing. Parkinsons is more than a movement disorder. The disease has a cognitive part as well, which means it can cause changes in the way your brain works.
During the final stage of the disease, some people may develop dementia or have hallucinations. However, hallucinations can also be a side effect of certain medications.
If you or your loved ones notice that youre getting unusually forgetful or easily confused, it might be a sign of advanced-stage Parkinsons.
The Link Between Sleep & Parkinson’s
“For most people night is a time of rest and renewal, however, for many people with Parkinsons disease night all too often brings anything but.” The American Parkinson’s Disease Association discusses “Sleep Problems in Parkinson’s Disease” to include “…very detailed and often frightening visions. Delusions may occur as well.”1
My husband was diagnosed with PD ten years ago. Together, we talk about the progression of not just the physical symptoms but also the cognitive issues as well. Way back in 2008 when Dan was diagnosed, I was a busy caregiver managing the night time needs of toddler boys and a sleepwalking sister. Now, my nights have transformed to confrontations with imaginary demons, intruders, and this night, a rifle-bearing burglar.
Also Check: What Are The Four Cardinal Signs Of Parkinson’s Disease
Falling Asleep During The Day
Not getting enough restful sleep at night, some medications, and possibly the disease itself leading to neurodegeneration can lead to daytime sleepiness and even sleep attacks in people with Parkinsons disease.
Excessive daytime sleepiness is one of the most frequent sleep disorder symptoms in Parkinsons disease and can affect a patients quality of life.
Trying to get more restful sleep at night and adjusting medications can help with excessive daytime sleepiness.
A new therapy from Theranexus is also currently being investigated in a Phase 2 clinical trial to help with excessive daytime sleepiness.
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Increased Feelings Of Anxiety Or Depression
Anxiety and depression have been linked to Parkinsons. In addition to movement problems, the disease can also have an impact on your mental health. Its possible that changes in your emotional well-being can be a sign of changing physical health as well.
If you are more anxious than usual, have lost interest in things, or feel a sense of hopelessness, talk to your doctor.
Also Check: Is Parkinson’s Disease Fatal
Medication Not Working The Way It Used To
In the early stages, taking medicine works well to get rid of symptoms. But as Parkinsons progresses, your medication works for shorter periods of time, and symptoms return more easily. Your doctor will need to change your prescription.
Dr. Valerie Rundle-Gonzalez, a Texas-based neurologist, says to pay attention to how long your medicine takes to kick in and when it stops working. She says you should feel like symptoms significantly improve or are almost gone while on medication.
What Is The Link Between Parkinsons And Dreams

Sleep disturbances are very common in people with Parkinsons and can comprise the entire spectrum of sleep disorders. Studies suggest that rapid eye movement sleep behaviour disorder, or RBD, can be one of the first symptoms of Parkinsons disease occurring years before motor symptoms and clinical diagnosis.
RBD is a sleep disorder characterised by the acting out of dreams that are vivid, often intense and frightening. People with this disorder do not experience the normal temporary paralysis of limbs during REM sleep, and have been known to yell, carry out conversations or hit themselves or their bed partner while asleep. These are known as dream enactment behaviours.
Vivid dreams are typically present in people with Parkinsons and RBD. The content of dreams, namely dreams with negative emotions, seems to predict long-term cognitive decline in people with Parkinsons.
Recommended Reading: Juvenile Parkinsonism Life Expectancy
Determinants Of Eds In Pd
Levodopa equivalent dose, sleep-disordered breathing, wearing-off phenomena and REM sleep amount during polysomnography were linked to EDS in our study .
EDS and Neurodegeneration
The neurodegenerative process itself has been implicated in the pathophysiology of EDS in PD. Longer disease duration and association with UPDRS III and the HY stage have been reported. In our series, patients with advanced/severe PD did not differ from patients with light/beginning PD . However, patients with motor fluctuations a sign of advanced PD had significantly lower mean sleep latencies on MSLT. This may be related to the involvement, usually later in the course of PD, not only of the nigrostriatal dopaminergic system but also of extrastriatal dopaminergic and non-dopaminergic neurons in the lower brainstem and midbrain involved in sleep-wake regulation .
EDS and Treatment
EDS and Polysomnographic Findings
In our series, 3 polysomnographic parameters were linked to EDS.
Sleep latencies are markers of sleep propensity. Patients with shorter sleep latency at night also had shorter MSL during the day and higher ESS scores, as partially shown by others .
EDS and CSF Hypocretin-1 Levels
CSF hypocretin-1 level was measured in 3 of our patients and was in the normal range, confirming that EDS in PD may be severe even in the absence of a detectable hypocretin deficiency .
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Read Also: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Why Are Some Dreams Particularly Vivid Or Negative For People With Parkinsons
REM sleep plays a pivotal role in processing emotional events, and several studies have shown that the consolidation of emotional memories occurs in this sleep stage. Vivid dreams tend to be more frequent when awakening from REM sleep, the stage disrupted by Parkinsons. Some drugs used to treat Parkinsons can also accentuate dream vividness.
Many people with the condition describe the content of their dreams as negative. The vividness and emotional description of dream reports correlate with the limbic system an area of the brain associated with our emotional life. Although the reasons why people with Parkinsons often experience negative dreams have not been fully explained, this is likely due to damage in a particular area of the brain.
Dr Daniele Urso.
Are You A Carer
Sleep and night-time problems are almost twice as common among carers of people with Parkinsons than in the general population.
If you are caring for someone with Parkinsons, these sleep disturbances may lead to an increased risk of depression and stress.
It may be difficult sometimes, but if youre a carer its important to have good sleeping habits. This will help improve your health, wellbeing and general quality of life.
Much of the advice on this page applies to you as a carer as well as the person you care for.
You May Like: Parkinsonian Syndrome Life Expectancy
Sleep And Depression In Parkinson’s Disease
Depression is seen in approximately 40% of PD patients in the course of their disease. Most persons with depression, including PD patients, also will experience problems with sleep. In depression, sleep does not refresh you like it used to, or you wake up too early in the morning. Dreams for depressed people are different, too–they are rare and often depict a single image.
Parkinsons Sleep Problems: Diagnosis And Treatment
Parkinsons disease is chronic and progressive, meaning it tends to get worse over time. However, there are treatment options that can help manage symptoms and allow patients to get more restful sleep.
The simplest way to start sleeping better with Parkinsons disease is by adopting healthy sleep habits. Sleep hygiene tips for Parkinsons disease sufferers include:
- Sticking to regular bedtimes
- Following a consistent bedtime routine with soothing activities such as listening to music or reading a calming book
- Getting regular exercise, preferably early in the day
- Getting adequate exposure to light, whether outdoors or through light therapy
- Avoiding long naps and naps late in the day
- Creating a cool, dark, and comfortable sleeping environment
- Restricting bedtime activities to sex and sleep only
- Turning off screens an hour before bedtime
- Reducing liquid intake before bedtime
- Avoiding caffeine, alcohol, and tobacco
- Eating a healthy diet and avoiding large meals at night
Light therapy, exercise, and deep brain stimulation have been successfully used to improve overall sleep quality and to treat specific conditions, such as REM sleep behavior disorder, in patients with Parkinsons disease. Cognitive behavioral therapy for insomnia has proven effective at reducing insomnia in healthy adults, although further research is needed on the effects of CBT in patients with Parkinsons disease.
- Was this article helpful?
Recommended Reading: Parkinson Disease Lifespan
What Treatment Options Exist For Those Experiencing Sleep Disturbance And Bad Dreams
Bad dreams are a perfectly normal occurrence and can be triggered by many factors, including stress, anxiety, sleep deprivation and medication. However, when bad and vivid dreams are accompanied by dream-enacting behaviour, people with Parkinsons can take some simple steps to minimise injury.
A safe sleeping environment is essential, so modifying sleeping arrangements should be the first step to treat REM behaviour disorders. Placing a mattress on the floor, padding corners of furniture, protecting windows and removing potentially dangerous objects from the bedroom are all simple and practical steps. Its also best to avoid alcohol intake, as this can trigger or aggravate RBD.
Two medications commonly prescribed to treat RBD are clonazepam and melatonin. Clonazepam should be used with caution in patients with dementia and gait disorders. Melatonin may have the advantage of fewer side effects and a longer-acting version, but in certain cases, only higher doses of melatonin will work.
