What Is The Prognosis
Although most people still need to take medication after undergoing DBS, many people experience considerable reduction of their PD symptoms and can greatly reduce their medications. The amount of reduction varies from person to person. The reduction in dose of medication can lead to decreased risk of side effects such as dyskinesia.
There is a 1 to 3% chance of infection, stroke, bleeding in the brain, or other complications associated with anesthesia. It is best to discuss associated risks with your neurologist and neurosurgeon, as diabetes and heart and lung conditions all may influence these risks and the decision to pursue surgery.
What Is The Success Rate Of Deep Brain Stimulation
In general, deep brain stimulation is usually successful. The success rate depends on the condition involved. For conditions like epilepsy and Parkinson’s disease, DBS is very effective. More research is necessary for conditions where DBS is experimental before experts know if DBS is likely to help.
Risks And Side Effects Of Deep Brain Stimulation
Like any surgery, deep brain stimulation can have side effects, and it carries potential risks. Its also important to consider the complications and side effects of medications you take since their dosages can often be reduced following surgery.
While DBS may cause side effects, it may also reduce side effects from medications.
Recommended Reading: Cure For Parkinson’s Disease 2022
Living With A Stimulator
Once the DBS has been programmed, you are sent home with instructions for adjusting your own stimulation. The handheld controller allows you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most patients keep their DBS system turned on 24 hours day and night. Some patients with essential tremor can use it during the day and turn off the system before bedtime. Your doctor may alter the settings on follow-up visits if necessary.
If your DBS has a rechargeable battery, you will need to use a charging unit. On average charging time is 1 to 2 hours per week. You will have a choice of either a primary cell battery or a rechargeable unit and you should discuss this with you surgeon prior to surgery.
Just like a cardiac pacemaker, other devices such as cellular phones, pagers, microwaves, security doors, and anti theft sensors will not affect your stimulator. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates.
What To Expect After Dbs

Surgery to implant the leads generally entails an overnight stay, while the IPG is usually implanted as same-day surgery. During recovery, your surgeon will talk to you about caring for your wounds, when you can shower, and any activity restrictions. Its usually recommended that any heavy lifting be avoided for a few weeks.
After another two to four weeks, youll return to have your device programmed. This process will continue for several weeks to ensure the stimulation settings are optimal to control your symptoms. During these visits, you will be shown how to turn the device on and off with the handheld device and check the battery level.
Once the programming has been completed, you will have regular follow-up visits to check and adjust the stimulation to maintain the most benefit for your symptoms.
Read Also: Alzheimer’s Disease And Parkinson’s Disease
How Effective Is Dbs Therapy
Though DBS is considered an alternative, its a well-established, FDA-approved technique that has been used to treat Parkinsons and essential tremor for 30+ years.
Theres been a lot of studies over the years, said Dr. Sheth. Randomized trials have been presented in the top medical journals that show that for the appropriately chosen patient, DBS is more effective than the best medical therapy. So, in that appropriately chosen patient, DBS can be very successful at improving tremor for essential tremor and tremor stiffness, rigidity, and those other motor symptoms of Parkinsons disease.
One patient who has found success with DBS is Rudy Hardy.
Its made a profound difference in my life, said Hardy. A professional sports photographer and professor of criminal justice, Hardys life was controlled by Parkinsons. He tried medication initially, and though it seemed to work for a while, his tremors eventually worsened. Since undergoing DBS, Hardys symptoms are now almost completely undetectable. Watch Hardy talk about his experience with DBS below.
Why Is Dbs Used
There are billions of neurons in each human brain, and these cells communicate with each other using electrical and chemical signals. Several brain conditions can make neurons in different parts of your brain less active. When that happens, those parts of your brain dont work as well. Depending on the part of the brain affected, you can have disruptions in the abilities controlled in that area.
DBS uses an artificial electrical current to make those neurons more active, which can help with the symptoms of several different brain conditions. However, researchers still dont know exactly how or why this works.
You May Like: Does Exercise Help Parkinson’s Disease
What Conditions And Symptoms Can Dbs Treat
DBS can treat several conditions that affect your brain, including movement disorders, mental health conditions and epilepsy.
DBS has approval from the U.S. Food and Drug Administration to treat the following conditions:
It’s important to keep in mind that while the above conditions might benefit from DBS, experts still don’t know if this is the case. It usually takes years of research and clinical trials to determine if a medical procedure like DBS is helpful for conditions like these. While researchers are looking into them, DBS surgery to treat these conditions is not common.
What Happens After Surgery
After surgery, you may take your regular dose of Parkinson’s medication immediately. You are kept overnight for monitoring and observation. Most patients are discharged home the next day.
During the recovery time after implanting the electrodes, you may feel better than normal. Brain swelling around the electrode tip causes a lesion effect that lasts a couple days to weeks. This temporary effect is a good predictor of your outcome once the stimulator is implanted and programmed.
About a week later, you will return to the hospital for outpatient surgery to implant the stimulator in the chest/abdomen. This surgery is performed under general anesthesia and takes about an hour. Patients go home the same day.
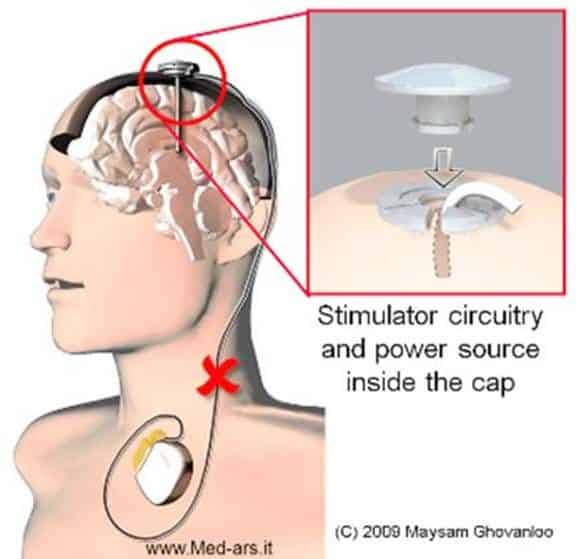
Step 7: implant the stimulator You will be taken to the OR and put to sleep with general anesthesia. A portion of the scalp incision is reopened to access the leads. A small incision is made near the collarbone and the neurostimulator is implanted under the skin. The lead is attached to an extension wire that is passed under the skin of the scalp, down the neck, to the stimulator/battery in the chest or abdomen. The device will be visible as a small bulge under the skin, but it is usually not seen under clothes.
You will have lifting and activity restrictions for 6-8 weeks while the incisions heal. Follow all discharge instructions and the neck exercises provided. Incision pain can be managed with medication.
Don’t Miss: How Do You Know When Parkinson’s Is Getting Worse
How Is Deep Brain Stimulation Used To Treat Parkinsons Disease
Deep brain stimulation delivers electrical impulses to a targeted area of the brain that is responsible for the movement symptoms caused by Parkinsons disease. The electrical impulses disrupt the abnormal activity that occurs in the brains circuitry, which is causing the symptoms.
There are three areas in the brain that can be targets for deep brain stimulation in patients with Parkinsons disease. They are the subthalamic nucleus, the globus pallidus internus, and the ventral intermediate nucleus of the thalamus. Each of these areas plays a role in the brains circuitry that is responsible for the control of movement.
The specific area in the brain to target in an individual with Parkinsons disease depends on symptoms that need to be treated. For example, deep brain stimulation of subthalamic nucleus is effective for all major movement symptoms of Parkinsons disease, such as tremor, slowness of movement , stiffness , and problems with walking and balance. Deep brain stimulation of globus pallidus is another effective target for a wide range of Parkinsons symptoms. The thalamic target is sometimes selected for patients with tremor symptoms. The recommended target for each patient is made collaboratively with the neurologist, neurosurgeon and other caregivers involved in the decision making process.
Read Also: Treating Depression In Parkinsons Disease
How Does It Work
A small device placed inside your chest sends electrical pulses to your brain. The pulses block nerve signals that cause Parkinsons symptoms.
A DBS system has four parts:
- A thin wire, called a lead, thats placed in the part of your brain causing symptoms
- A pulse generator, like a pacemaker, that sends tiny electrical signals to the lead
- A wire that connects the lead to the pulse generator
- A remote control to program the system the only part outside your body
After the system is in place and turned on, a DBS expert will adjust it so you get the best relief for your symptoms.
You can also control the system yourself. You can turn it off and on, check the battery, and tweak the settings.
Don’t Miss: Can A Ct Scan Detect Parkinson’s Disease
Is Deep Brain Stimulation Right For You
While deep brain stimulation is shown to offer long-term benefits, the treatment does come with some risks. According to the Parkinsons Foundation, there is a 1% to 3% chance of developing an infection, cranial bleeding, stroke, or other complications from the treatment.
Furthermore, deep brain stimulation might work better for some people than others. It might be an option worth considering if youve experienced symptoms of Parkinsons for at least five years, are struggling with side effects of Parkinsons medications, or your symptoms make it difficult to perform everyday activities, among other factors.
The decision for or against deep brain stimulation should be made by having the potential candidate evaluated by a multidisciplinary team who can together construct a risk-benefit profile for a potential candidate, explains Dr. Okun. The team commonly is made up of a neurologist, a neurosurgeon, a neuropsychologist, a psychiatrist, and rehabilitation specialists.
Talk with a neurologist if you have Parkinsons disease and youre interested in exploring deep brain stimulation.
Also Check: Cleveland Clinic Parkinsons Bicycle Study 2017
Sites Of Deep Brain Stimulation And Symptom Control

While both subthalamic nucleus and globus pallidus internus stimulation help improve the motor symptoms of Parkinsons disease, studies have found a few differences.
DBS of the third target, the ventral intermediate nucleus, can be beneficial for controlling tremors but does not work as well at addressing the other motor symptoms of Parkinsons disease.
In a Canadian study, targeting the subthalamic nucleus allowed people to reduce the doses of their medications to a greater degree, while targeting the globus pallidus internus was more effective for abnormal movements .
In another study, STN deep brain stimulation also led to a greater reduction in medication dosages. However, GPi stimulation resulted in greater improvement in quality of life, and also appeared to help with the fluency of speech and depression symptoms.
Side effects of DBS can sometimes include subtle cognitive changes . A different study compared these effects with regard to these different areas.
GPi showed smaller neurocognitive declines than STN, though the effects were small with both. On a positive note, both procedures seemed to reduce symptoms of depression following surgery.
Read Also: What Are The First Signs Of Parkinson’s Disease
Why A Doctor May Choose Deep Brain Stimulation
According to the National Parkinson Foundation, the ideal Parkinsons disease candidate for DBS surgery has:
-
PD symptoms that interfere with activities of daily living.
-
Fluctuations in mobility due to PD medications with or without dyskinesia .
-
Continued good response to PD medications, even if the medication effects may wear off sooner than they have in the past.
-
A history of several different combinations of PD medications while under the supervision of a neurologist specializing in movement disorders.
These factors* may make a person a less than ideal candidate for DBS surgery:
-
Difficulty with balance, walking, or freezing as the main disabling symptom.
-
A primary symptom of speech difficulty.
-
Continuous confusion and problems with memory and thinking.
-
A psychiatric condition such as depression or anxiety that has not improved or stabilized with other treatment.
-
Another condition that increases the risk for surgery complications.
*Some of these factors may be treatable. Having one or more does not disqualify a person for future DBS surgery, but the doctor may recommend more aggressive therapy focused on these issues before surgery takes place.
How Long Will I Be Hospitalized For
Deep brain stimulation is usually done in two steps. The first procedure consists of inserting the electrodes into the brain and usually requires you to stay in the hospital for a few days.
The second procedure, which consists of implanting the stimulator and batteries, is minor. You should be able to return home quickly. Depending on the model, the stimulator batteries may need to be recharged or replaced within three to five years.
Recommended Reading: How Can You Treat Parkinson Disease
How Deep Brain Stimulation Works
Exactly how DBS works is not completely understood, but many experts believe it regulates abnormal electrical signaling patterns in the brain. To control normal movement and other functions, brain cells communicate with each other using electrical signals. In Parkinson’s disease, these signals become irregular and uncoordinated, which leads to motor symptoms. DBS may interrupt the irregular signaling patterns so cells can communicate more smoothly and symptoms lessen.
Deep Brain Stimulation For The Treatment Of Parkinsons Disease And Other Movement Disorders
Parkinson’s disease is a neurodegenerative disorder that leads to resting tremor, rigidity, slowness of movement, and postural instability. These symptoms are caused by degeneration of neurons in the substantia nigra pars compacta , one of a group of brain structures known as the basal ganglia and part of a circuit crucial for coordinating purposeful movement. This circuit relies on the chemical messenger dopamine, which is produced by SNc neurons. As PD progresses and these neurons are lost, reduced dopamine results in abnormal circuit activity and motor symptoms.
The molecular precursor to dopamine, L-DOPA , is used to treat PD. However, people in later stages of the disease experience off periods when this medication does not work well, and L-DOPA treatment can also trigger uncontrolled involuntary movement, a condition called dyskinesia. deep brain stimulation can offer symptomatic relief in later stages of PD and may reduce requirements for L-DOPA treatment and exposure to its side effects. DBS is also used to treat other movement disorders, including essential tremor, which causes involuntary shaking that worsens during movement, and dystonia, which causes involuntary muscle contractions and slow, repetitive movements or abnormal postures.
Also Check: How Often Does Parkinson’s Disease Occur In The Population
Which Brain Targets Should Be Used To Implant The Dbs Lead
- There are three brain targets that the FDA has approved for use in Parkinsons: the subthalamic nucleus and the globus pallidus interna are the most common.
- The target choice should be tailored to a persons individual needs.
- There are many ongoing studies that will help refine target choice for individual people.
- Although the picture is not yet clear on the issue of target choice, the STN seems to provide more medication reduction, while GPi may be slightly safer for language and cognition.
Dbs Therapy Benefits & Risks
- Less medication, more reliefMedtronic DBS Therapy may reduce Parkinsons medication.1 This may reduce medication-related side effects like unintended movements , while simplifying your medication routine, with fewer pills or less frequent doses.
- Better morningsDBS delivers therapy 24 hours a day it doesnt wear off while you sleep. Its already working the moment you wake up.
- Lifestyle improvementsUnlike some other Parkinsons therapies, the DBS system requires no daily cleaning or refilling.
- More good hours of movement controlEach day, DBS provides additional hours of good movement control without unintended movements , compared to medication alone.1
- A better quality of lifeIn combination with medication, DBS Therapy has helped people with Parkinsons enjoy an improved quality of daily life, compared to those taking medication alone.1
- Keep your options openUnlike some surgeries for Parkinsons, DBS is reversible. The system can be turned off or removed, in most cases, and wont limit your future treatment options.
Patients should always discuss the potential risks and benefits of the therapy with a physician. A prescription is required. DBS Therapy requires brain surgery. Risks of brain surgery may include serious complications such as coma, bleeding inside the brain, stroke, seizures and infection. DBS Therapy may cause worsening of some symptoms. See Important Safety Information.
You May Like: Can You Reverse Parkinson Disease
What Is Deep Brain Stimulation And How Does It Work
DBS is a therapy that we have for various neurological conditions, said Dr. Sheth. It’s a system that you can think of like a pacemaker. But rather than being a pacemaker for the heart, it’s for the brain.
Dr. Sheth describes the brain as having many circuits that govern everything we do, including how we move.
If the movement circuit is not working properly, we may have a movement disorder like Parkinson’s, he said. If we can identify the circuit within the brain that is not working properly, we can use this device to reset the rhythms in the brain and restore the balance so that our movements can be better controlled or without a tremor.
Awake Vs Asleep Surgery
Standard DBS surgery is performed while you are awake and requires that you stop taking the medicines that control your Parkinson’s symptoms. During surgery, you are asked to perform tasks to help guide the electrode to the precise location in the brain.
Being awake during brain surgery, or being off medicine, is unsettling for some people. Asleep DBS is an alternative option at some centers.
Asleep DBS surgery is performed while you are unconscious and under anesthesia. Surgery takes place in an MRI or CT scanner to target and verify accurate placement of your DBS electrodes. Ask your surgeon if asleep DBS is an option for you.
| Must hold medications the morning of surgery | Don’t have to hold medications |
Read Also: Is There Any Medication For Parkinson’s Disease
