Related: Ethics Questions Swirl Around Historic Parkinsons Experiment
They pulled into Cornells driveway two hours late. Kim grabbed the cooler and handed it to a waiting Cornell official, who carried it up to the cell facility. There, a technician loaded syringes with the brain cells. Then Kim saw the cells: They had formed very un-therapeutic-looking clumps. If this had been the day of the actual surgery, it would have been ruinous.
This, Kim thought, is why we do practice runs.
A month later, when the cells journeying from Boston to New York were to actually be transplanted, it seemed that Kims nearly decade-long project was cursed: He learned that Hanscom would be closed on Sept. 5, the day of the surgery. They had to leave from the much busier Logan Airport.
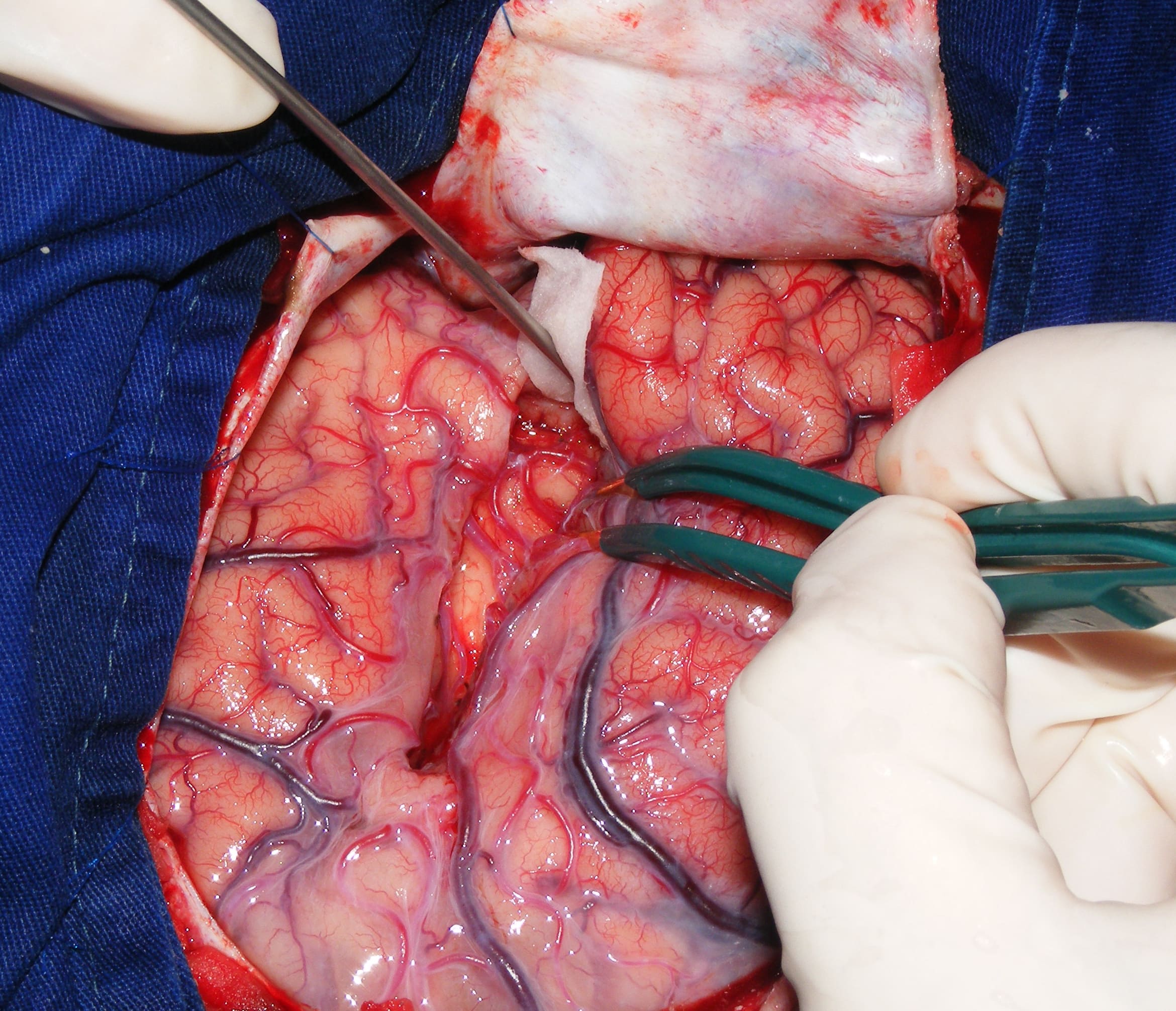
But the air ambulance was wheels up at 5 a.m. and arrived at Weill Cornell at 6:30. Technicians carefully sucked the cells into special syringes, which Song speed-walked to the surgical suite where the neurosurgeon and the patient awaited.
In late 2018, news reports said surgeons in Japan had, that October, performed an experimental procedure that had been on neurologists wish list for more than a decade: transplanting into the brain of a Parkinsons patient replacement cells created from the patients own skin cells using a Nobel-winning protocol. It was, claimed the reports, a first.
It wasnt.
Believe They May Cure A Disease Like Parkinsons
Sometimes I find it difficult to explain stem cells to patients and family members. One simple explanation that resonates is comparing the stem cell to child development. Early in development, parents can influence the child to differentiate into one area of life or another and develop a skill set for success in adulthood. Stem cells are a potentially self-renewing resource that can be influenced by scientists to differentiate into a needed tissue .
Now close your eyes and imagine this scenario. You travel to a far away clinic and upon arrival they describe these amazing cells drop them into the brain and cure Parkinsons. They use catch phrases like self renewing. They tell you, we can make dopamine cells and give them back to you. Sign me up right? Not so fast.
Future Prospects For Neural Transplantation
To fully evaluate the effectiveness of dopamine cell transplants for Parkinsons disease, a uniform source of dopamine neurons must be developed. Differentiation of embryonic stem cells or induced pluripotent stem cells to dopamine neurons may produce an unlimited number of dopamine neurons for transplant. We have found that allografts of human fetal mesencephalon are not rejected, unlike most somatic tissue transplants. Therefore, donor-specific embryonic stem cells will probably not be required, although the immunogenicity of stem cell-derived dopamine neurons could be different from fetal mesencephalon. Because of the enormous immunologic differences between species, successful xenografts are improbable.
Because dyskinesias in patients with Parkinsons disease may be a consequence of secondary anatomical and physiological changes in the basal ganglia after a long period of dopamine denervation and L-DOPA treatment, a clinical trial of transplantation early in Parkinsons disease may show that transplantation prevents the development of L-DOPA-induced dyskinesias. We proposed such a study to the NIH in 2003, but the idea was rejected at that time.
You May Like: Weed Killer Causes Parkinson’s
Studies Show Promising Results
“Considering the ability of MSCs to secrete neurotrophic factors, modulate inflammation, and possibly even act as mitochondria âdonorâ, it comes as no surprise that there is a lot of interest in the use of MSCs in the treatment of Parkinsons Disease, and a multitude of animal studies has shown promise. Treatments have resulted in improvement of motor function, protection of the nigrostriatal system, and improved striatal dopamine release in several studies using toxic lesion rodent models of Parkinsons Disease. Similar effects were reported with umbilical cord-derived MSCs with or without prior differentiation. For example, a recent study reported improvement of motor function, reduced microglial activation, and decreased loss of TH immunoreactivity, associated with local production of trophic factors.
Learn more about DVC Stem’s protocol for Parkinson’s Disease here:
References:
Venkataramana, N. K., Kumar, S. K. V., Balaraju, S., Radhakrishnan, R. C., Bansal, A., Dixit, A., ⦠Totey, S. M. . Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease. Retrieved from https://www.sciencedirect.com/science/article/pii/S1931524409002205#!
Unified Parkinson’s Disease Rating Scale. . Retrieved from https://www.sciencedirect.com/topics/medicine-and-dentistry/unified-parkinsons-disease-rating-scale
About the author
Subjective Primary Outcome Variables Should Not Be Used For Evaluating Long
Our double-blind trial has provided the only evidence of improved clinical outcome in a controlled neurosurgical trial of fetal dopamine cell transplantation. Despite these positive results, our study was formally deemed negative because of the unfortunate choice of a primary outcome variable. Our Columbia colleagues had insisted that the primary outcome variable be the subjective statement by each patient as to how they felt 1 year after the surgery compared to before the surgery. This variable proved to be meaningless because patients could not recall what their condition had been before the surgery. We conclude that subjective variables have no value for measuring outcome in a long-term study of Parkinsons disease.
You May Like: Possible Causes Of Parkinson’s Disease
A Sniff Test For Alzheimers Checks For The Ability To Identify Odors
Henchcliffe and Tabar joined several other prominent scientists to describe plans to revive brain cell transplants during a session Tuesday at the International Society for Stem Cell Research meeting in Boston.
Their upbeat message marks a dramatic turnaround for the approach.
During the 1980s and 1990s, researchers used cells taken directly from the brains of aborted fetuses to treat hundreds of Parkinsons patients. The goal was to halt the disease.
Parkinsons destroys brain cells that make a substance called dopamine. Without enough dopamine, nerve cells cant communicate with muscles, and people can develop tremors, have difficulty walking and other symptoms.
Drugs can temporarily raise dopamine levels, easing symptoms. But their effectiveness tends to wane over time.
So researchers thought a better approach would be to simply replace the cells that produce dopamine. The rationale is that if those cells are lost, and we know they make dopamine, and we know that dopamine is important for good coordination, good automatic movement, why could we not replace those cells, Henchcliffe says.
For some patients, the transplanted fetal cells produced dramatic improvements. But rigorous studies eventually showed that many other patients were not helped. And some developed an unwelcome side effect: uncontrolled movements.
That took a while. But its clear now that over the long term, some patients really were helped by the procedure.
Preoperative Response To L
Because all subjects are now more than 10 years post-transplant, long-term analysis is possible. 18F-FDOPA PET scans have shown that transplants develop during a 2-year period and are stable at 4 years after transplant . As previously noted, the most important predictor of response to transplant was the magnitude of the preoperative response to L-DOPA. Patients who had less than 50% improvement after the first morning dose of L-DOPA did not respond to transplant. In our group of subjects, L-DOPA had a much broader range of effects in those who were older than 60 years of age compared to younger. Some older patients had only the minimal 30% improvement in UPDRS scores required to enter the study, whereas others had as much as a 90% improvement. Preoperatively, subjects who were less than 60 years of age had an average of 79% improvement after L-DOPA, whereas those who were older than 60 years of age had only 54% improvement. That difference in the preoperative response to L-DOPA fully accounts for the difference in transplant outcome for the two age groups. We have found that only subjects who have excellent clinical improvement preoperatively with L-DOPA will have a positive response after dopamine neurotransplantation.
Don’t Miss: Can You Have Parkinson’s Without Shaking
Dyskinesias Seen In Some Transplant Subjects In The Off State
Olanow et al. did note dyskinesias were present in the off state in a large proportion of their transplant subjects and in none of the sham surgery patients. Although the dyskinesias were of minor significance in most, some patients required the placement of deep brain stimulating electrodes in the subthalamic nucleus to control excess movements. Therefore, Olanow et al. replicated our earlier observation that transplants could reproduce dyskinesias in patients with an earlier history of drug-induced dyskinesias.
What Is Parkinson’s Disease
Parkinson’s Disease is a degenerative nervous system condition that affects one’s movement. Symptoms often start quite gradually, with minor issues such as small tremors within the extremities . Currently, there is no cure for Parkinson’s Disease but certain medications do have the capacity to help manage symptoms. Some doctors may also recommend surgery to address certain symptoms, which involves regulating certain areas of the brain.
Also Check: Does David Brooks Have Parkinson’s
A Stroll To Times Square
Lopez had barely settled back into his hospital bed after the four-hour operation when he felt his muscles strengthening and the tremors dissipating. He threatened to arm-wrestle the surgeon who came to check on him. And he told his personal assistant that he wanted to get the heck out of the hospital and take a walk. I said, this is what it feels like to be normal, Lopez recalled.
Lopez, his son, and the assistant walked the 2 miles to Times Square under a nearly cloudless sky, in a balmy 70 degrees with only a light wind fluttering the awnings along Broadway. Lopez had had his new dopamine-producing neurons only a few hours, but it already felt like Lourdes had slipped through a wormhole in the space-time continuum and landed in Manhattan.
It was the sort of description that made his physicians squirm. As Lopez and his doctors recounted the saga a year later, Carter brought the discussion crashing back down to reality. He didnt dispute that Lopez felt and moved much better in the immediate aftermath of the cell implants. But that did not mean they worked.
Weve seen this sort of immediate I feel better before, said Carter, who is now chief of neurosurgery at Mass. General. It takes much longer, on the order of months, for dopamine-neuron progenitor cells like those Lopez received to form synapses with existing neurons and thereby start to restore lost motor functions.
Related: It Started As A Weird Idea But A New Study Shows The Appendix Can Initiate Parkinsons
Kim knew it would take tens of millions of dopamine neurons to have a prayer of helping a Parkinsons patient. The recipe for turning undifferentiated iPS cells into dopamine neurons wasnt perfect, however, which presented a problem: The remaining iPS cells can seed tumors.
Even after two or three weeks of differentiation, there can remain undifferentiated cells, Kim said. If he turned 99.9% of iPS cells into dopamine neurons, that would leave 10,000 iPS cells. Hitting 99.99% would leave 1,000. How efficient was efficient enough? We realized we needed to remove all of them, Kim said.
That meant looking for a killer. Kim and colleagues in South Korea pored over a database of compounds, searching for any that target a gene called survivin, which is abundant in iPS cells. They got a hit: quercetin. Testing the Chinese herbal compound on his iPS cells, Kim found, if you treat the cells once, for 12 hours, while theyre differentiating, quercetin completely removes the undifferentiated cells.
It was time to start thinking about putting the cells in someones brain.
Recommended Reading: Does Magnesium Help Parkinson’s
Age As A Predictor Of Transplant Outcome
Although Parkinsons disease is primarily a disease of elderly people, some researchers have been hesitant to perform transplantation in older patients. Our double-blind study specifically addressed the issue of age with half of the recruited patients who were 60 years of age or older and with half of the patients who were younger than 60 years of age. As previously noted, it was not age per se, but the preoperative response to L-DOPA that correlated with transplant outcome. In the aging brain, the symptoms of Parkinsons disease are likely to be a manifestation of a more global neuropathologic process.
What Have Clinical Trials Found
Until the discovery of the process of creating iPSCs, the only stem cell therapies for Parkinsons disease required the use of embryonic stem cells. This came with ethical and practical challenges, making research more difficult.
After iPSCs became available, stem cells have been used in clinical trials for many conditions involving neural damage with overall mixed results.
The first clinical trial using iPSCs to treat Parkinsons disease was in 2018 in Japan. It was a very small trial with only seven participants. Other trials have been completed using animal models.
So far, trials have shown improvement to symptoms affecting movement as well as nonmotor symptoms such as .
Some challenges do arise from the source of the stem cells.
Stem cell therapy can be thought of as being similar to an organ transplant. If the iPSCs are derived from a donor, you may need to use immunosuppressant drugs to prevent your body from rejecting the cells.
If the iPSCs are derived from your own cells, your body might be less likely to reject them. But experts believe that this will delay stem cell therapy while the iPSCs are made in a lab. This will probably be more costly than using an established line of tested iPSCs from a donor.
You May Like: What Does Dbs Do For Parkinson’s
Transplantation Of Human Fetal Mesencephalic Tissue
Despite three decades of experimental and clinical work, transplantation of human fetal mesencephalic tissue has not yet been developed into a clinically competitive treatment for PD patients. However, these studies have provided valuable insight into the basic principles of cell therapy in PD. Implantation of human fetal DA-rich mesencephalic tissue is, therefore, regarded as a gold standard when moving dopaminergic neurons derived from other sources towards clinical application.
It is well established, from a large number of studies, that the fetal dopaminergic neurons can survive and grow after intrastriatal transplantation into the PD patient’s brain. Positron emission tomography has demonstrated increased 18F-DOPA uptake in the grafted putamen , and histopathological studies have shown survival of implanted dopaminergic neurons and reinnervation of the striatum . Four patients with major clinical improvement, in whom 18F-DOPA uptake was normalized in the grafted putamen from 10 to 16 years post-surgery, showed normal DA release, as assessed by 11C-raclopride binding, at 710 years after transplantation . Providing evidence for their functional integration into host neuronal circuitry, the fetal mesencephalic grafts reversed the deficits in movement-related cortical activation with a time course paralleling that of the clinical improvement .
Dopaminergic Grafts Derived From Human Embryonic Stem Cells
Graft survival and behavioural improvements following intrastriatal transplantation of human ES cell-derived dopaminergic neurons in a rat PD model were first reported almost a decade ago . The grafts showed large numbers of dopaminergic neurons of substantia nigra phenotype but also contained potentially tumourigenic, mitotic undifferentiated neuroepithelial cells. There was a breakthrough in the field in 2011 when Kriks and co-workers described a new protocol, guided by developmental principles, which efficiently converts human ES cells to dopaminergic neurons. Floor plate cells are derived in vitro using dual inhibition of SMAD signalling and high levels of Sonic Hedgehog. A midbrain floor plate identity is then induced by activation of Wnt signalling, and cells are differentiated to dopaminergic precursors. After intrastriatal transplantation of these precursors in rodents, high numbers of substantia nigra dopaminergic neurons survived long-term. No tumours were observed. The grafts could reinnervate a major portion of striatum also in a larger brain, and improved functional deficits in rodents relevant for the clinical condition. In parallel, a very similar protocol was developed by Kirkeby and co-workers .
Read Also: How Many People In Us Have Parkinsons
Individualized Brain Cell Grafts Reverse Parkinsons Symptoms In Monkeys
Grafting neurons grown from monkeys own cells into their brains relieved the debilitating movement and depression symptoms associated with Parkinsons disease, researchers at the University of WisconsinMadison reported today.
In a study , the UW team describes its success with neurons made from induced pluripotent stem cells from the monkeys own bodies. This approach avoided complications with the primates immune systems and takes an important step toward a treatment for millions of human Parkinsons patients.
This result in primates is extremely powerful, particularly for translating our discoveries to the clinic, says UWMadison neuroscientist Su-Chun Zhang, whose Waisman Center lab grew the brain cells.
Parkinsons disease damages neurons in the brain that produce dopamine, a brain chemical that transmits signals between nerve cells. The disrupted signals make it progressively harder to coordinate muscles for even simple movements and cause rigidity, slowness and tremors that are the diseases hallmark symptoms. Patients especially those in earlier stages of Parkinsons are typically treated with drugs like L-DOPA to increase dopamine production.
Su-Chun Zhang
The idea is very simple, Zhang says. When you have stem cells, you can generate the right type of target cells in a consistent manner. And when they come from the individual you want to graft them into, the body recognizes and welcomes them as their own.
Cell Therapy For Parkinsons
The first idea to be clear on is that stem cells are not a FDA approved therapy for Parkinsons disease. A number of years ago, several of us at the Parkinsons Foundation, came up with a list of considerations for anyone considering a stem cell transplant.
1- you should never be charged for stem cell therapy for Parkinsons.
2- ask for the institutional review board approval letter, protocol and informed consent and bring it to your doctor to examine for authenticity. A true research study will have an approved and monitored protocol and stringent measures for patient safety.
3- if they point to a listing on clinicaltrials.gov as the reason their therapy is legit, please keep in mind almost anyone can access this system and it does not prove legitimacy.
4- if they promise a cure or alternatively the same treatment is offered for multiple diseases this should raise suspicion.
5- the Parkinsons Foundation put together some helpful tips if you are considering stem cell therapy. Also they have a free 18004PDINFO helpline with professionals who can help to address your questions.
Don’t Miss: Icd 10 Code Parkinson’s Disease
