Cell Type Gene Specificity Defined By Gene Regulation
based on current methodologies that rely on absolute gene expression levels, Gene 1 is not defined as cell type-specific while Gene 2 is defined as cell type A specific showing higher gene expression in cell type A than in cell type B. based on methods that look at variation in gene regulation mechanisms, such as expression quantitative trait loci or eQTLs, across cell types, Gene 1 is defined as cell type A specific while Gene 2 is defined as cell type B specific. These genetic effects on gene regulation can be more informative in deciphering the functional role of disease-associated variants at cell type resolution.
Understanding And Manipulating Cellular And Circuit
Study Rationale: Many people with Parkinsons disease develop untreatable cognitive symptoms, including problems with attention, decision-making, and dementia at late stages of the disease, due to changes in a crucial part of the brain, the cerebral cortex. Evidence suggests that aggregation of the protein alpha-synuclein in vulnerable nerve cells interferes with their health and damages the cellular networks required for normal brain function. However, the relationships between alpha-synuclein, vulnerable cells, and network activity are not understood. By identifying and understanding the causes and effects of this damage in brain networks, and affected nerve cells and their connections, we aim to enable therapies that directly target this disorder.
Hypothesis: We hypothesize that networks of nerve cells in the cortex of the brain become dysfunctional because of damage caused by pathological deposits of the protein alpha-synuclein in vulnerable cells.
Impact on Diagnosis: Diagnostic biomarkers for PD can leverage our findings of which types of neurons, their connections, and molecular markers are most affected. For treatment, our work will define novel mechanisms that can directly restore network function by targeting specific types of cortical nerve cells and their connections.
Leadership
Circuitry and Brain-Body Interactions | 2021
Quantification Of Astrocyte And Microglia Abundance And Microglial Neutral Lipid Content
GFAP-immunolabeled HS SN and PD SN whole-ventral midbrain sections were tile-scanned with a Keyence BZ-X700 fluorescent microscope using a 20× objective with fixed exposure and cutoff values. Stitched images containing the entirety of the tissue were thresholded in ImageJ , and the indicated region of the SNpc was outlined manually. The analyze particles plug-in was used to quantify the percentage of SNpc occupied by the GFAP+ signal above threshold relative to the measured area. TMEM119+ microglia and TO-PRO+ nuclei were imaged by confocal fluorescent microscopy in four to six randomly chosen fields of view within the SNpc, at 100× magnification. TMEM119+/TO-PRO+ microglia were manually counted, and the mean average cells per field of view per patient were reported. TMEM119+ microglial neutral lipid content was determined by imaging of TMEM119 and BODIPY at fixed settings, manual isolation of TMEM119+/TO-PRO+ cell profiles, and measurements of the average integrated density of BODIPY+ signal per cell. The experimenter was blinded to the patient group being imaged and analyzed.
You May Like: Does Sam Waterston Have Parkinson
Breaking Down The Parkinson’s Pathway: How Affected Brain Cells Respond During Different Behavioral Tasks
by Anne Trafton, Massachusetts Institute of Technology
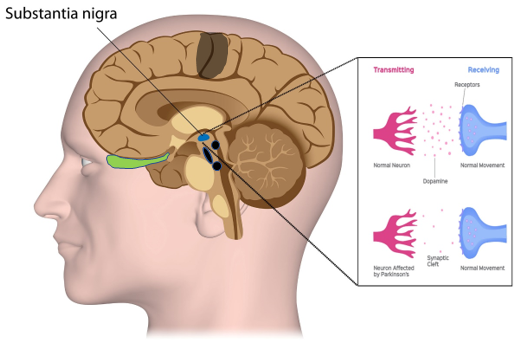
The key hallmark of Parkinson’s disease is a slowdown of movement caused by a cutoff in the supply of dopamine to the brain region responsible for coordinating movement. While scientists have understood this general process for many years, the exact details of how this happens are still murky.
“We know the neurotransmitter, we know roughly the pathways in the brain that are being affected, but when you come right down to it and ask what exactly is the sequence of events that occurs in the brain, that gets a little tougher,” says Ann Graybiel, an MIT Institute Professor and member of MIT’s McGovern Institute for Brain Research.
A new study from Graybiel’s lab offers insight into some of the precise impairments caused by the loss of dopamine in brain cells affected by Parkinson’s disease. The findings, which appear in the March 12 online edition of the Journal of Neuroscience, could help researchers not only better understand the disease, but also develop more targeted treatments.
Lead author of the paper is Ledia Hernandez, a former MIT postdoc. Other authors are McGovern Institute research scientists Yasuo Kubota and Dan Hu, former MIT graduate student Mark Howe and graduate student Nuné Lemaire.
Cutting off dopamine
The interneurons, however, never developed the firing patterns seen in normal interneurons during learning, even after the rats had learned to run the maze. The local circuits were disabled.
Explore further
Causes Of Parkinsons Disease
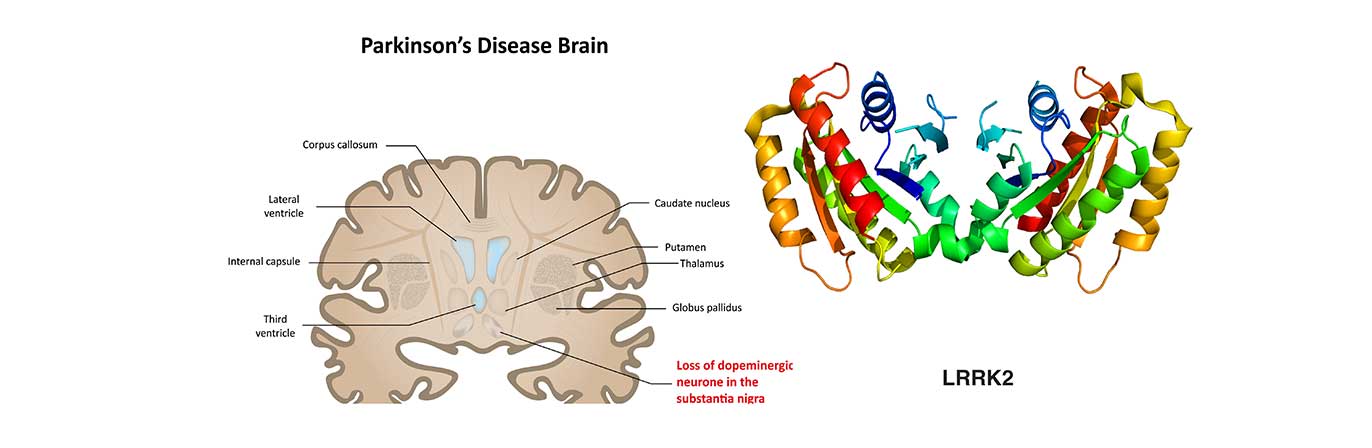
Parkinsons disease is a progressive neurodegenerative disorder best known for its movement-related symptoms. However, it also causes cognitive changes.
Parkinsons underlying cause is the death of dopamine-producing neurons, or nerve cells, in a brain region called the substantia nigra.
Dopamine is a neurotransmitter, which is a molecule produced by the body to send messages between nerve cells. It is involved in a range of behaviors, including control of body movements, learning and memory, the sleep-wake cycle, and moods, such as depression and mania.
Both genetic and environmental factors appear to influence a persons risk of developing Parkinsons. Thats why the disorder is thought to be a product of a combination of these factors. Genetics loads the gun and environment pulls the trigger, is one way Parkinsons has been described.
Read Also: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
The Cellular Composition Of Ad Brains Is Altered
Most neuronal markers are significantly downregulated in AD temporal cortex samples from the MayoClinic dataset . In contrast, all astrocytic and a few microglial and oligodendrocytic markers are significantly upregulated in AD brains.
CIBERSORTx , a tool that estimates cell type abundances in tissues from their bulk transcriptomes and machine learning-inferred cell-type-specific gene expression profiles, was used to derive the composition in major cell types of AD brain samples . These estimates are concordant with the observations in Figure 1A, including significant increase and decrease, respectively, in the proportions of astrocytes and neurons in AD brain samples. Despite the known differences in gene expression between mouse and human brain cells , the same trends can be seen using the mouse signature . We also performed principal component analysis on normalized gene expression in the MayoClinic brain samples. The neuronal composition, along with the disease effect, is correlated with the first principal component , i.e., that retaining the most data variance . Sex also shows a strong association with PC1 but there is no significant difference in age or neuronal proportion between female and male individuals .
Don’t Miss: What Essential Oils Are Good For Parkinson’s Disease
Modeling Pd In The Lab
Neurons are difficult to study within the brains of living people, and they cannot be extracted and grown in the lab for research purposes. Based on a Nobel prize-winning scientific breakthrough from 2006, scientists have another way to study neurons from patients. Cells from the skin or blood can now be reprogrammed to an embryonic-like state, called induced pluripotent stem cells, which are then capable of becoming any cell type in the body, including neurons of the brain. For example, blood cells taken from a patient with PD can be reprogrammed into iPS cells in a lab. Those cells can in turn be made into a virtually unlimited supply of dopamine-producing and other types of neurons that can be closely studied by scientists.
Since these cells have the same genetic makeup as the patient, they can exhibit the same disease-processes as the cells in the patient. By comparing the development of iPS cell-derived neurons from PD patients to those from healthy individuals, researchers are studying what goes wrong in PD neurons, and what genes may be involved in the development of the disease. Scientists can use these neurons to further understand disease progression as well as discover new drugs that might be effective at delaying or reversing the disease.
Cortical Pathophysiology Of Parkinsonism
Study Rationale: The outer mantle of the brain, the cerebral cortex, plays a significant role in selecting and controlling movements. Changes in the activity of cortical neurons are key to disorders of movement, especially Parkinsons disease . It is unknown, however, which specific cell types are involved and how their activity changes during the course of the disease. In these experiments, we will use new technologies to study large groups of specific types of cortical neurons and explore how their activity and morphology change in animal models of chronic PD.
Hypothesis: Our hypothesis is that groups of cortical neurons that send fibers to the spinal cordunlike those that send projections to the striatumstart to show abnormal activity and undergo morphological changes in connections that provide inputs to them when parkinsonism develops.
Impact on Diagnosis: A better understanding of how movement problems in PD develop is key to developing more effective methods to control them. Characterizing the abnormalities in specific families of cortical neurons may allow us to develop new therapies that target the affected circuits through deep brain stimulation, pharmacologic, or genetic methods.
Leadership
Don’t Miss: Can A Teenager Get Parkinson’s Disease
How Do Symptoms Progress And What Is The Outlook
The symptoms of PD tend to become gradually worse over time. However, the speed of progression varies greatly from person to person. When symptoms first begin, you may not need treatment when symptoms are relatively mild.
Most people with PD can expect to have some time of relatively mild symptoms. Then, when the symptoms become worse, they can expect several years of good or reasonable control of the symptoms with medication. But everyone is different and it is difficult to predict for an individual how quickly the disease will progress. Some people may only be slightly disabled 20 years after PD first begins, whereas others may be very disabled after 10 years.
Research into PD is active. For example, one main aim of research is to find medicines that prevent the damage to the affected cells, rather than just treating the symptoms, which is the main value of treatment at present. Further research on these chemicals continues. Research is underway using stem cell therapy to help treat PD. Other researchers are looking at alpha synuclein, a protein that gathers around the junction between nerve cells and is thought to affect the way messages are conducted between the brain and the nerves controlling movement.
Further reading and references
Sn Microglia Accumulate Neutral Lipids In Pd
Next, to investigate the possibility of lipid changes in microglia accompanying the perturbed lipid distribution in neurons and astrocytes, HS and PD SN sections were costained with BODIPY and an antibody to TMEM119 to visualize microglial neutral lipid storage and overall microglial abundance . PD SN contained more numerous and larger microglial cell profiles per field of view , and PD SN microglia had more associated BODIPY+ neutral lipids compared with age-matched HS SN microglia .
Microglia accumulate neutral lipids in PD SN. Representative micrographs of BODIPY and TMEM119 colabeled microglia in HS SN and PD SN. Boxed insets are shown in higher magnification with orthogonal views on the right. Dashed lines indicate TMEM119+ microglial cell outlines. Nuclei are shown in merged views . Average number of TMEM119+/TO-PRO+ microglia per randomly chosen field of view. **P< 0.01, n = 4 to 6 subject averages per group, n = 4 to 6 fields of view per subject. Quantification of BODIPY+ neutral lipid associated with TMEM119+/TO-PRO+ microglial cell profiles. *P< 0.05, n = 4 to 6 subject averages per group, n = 5 to 10 microglial cell profiles per subject.
Recommended Reading: Life Expectancy After Parkinson’s Diagnosis
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Mapping The Modulatory Landscape Governing Striatal Dopamine Signaling And Its Dysregulation In Parkinsons Disease
Study Rationale: Nerve cells that produce the brain chemical dopamine die in people with Parkinsons disease . These nerve cells extend long and thin fibers called axons that release dopamine from thousands of different points, sending signals to other nerve cells in a brain area called the striatum. Many different types of cells and molecules in the striatum can directly control how dopamine is released, but we havent yet discovered which ones are the most important and how they are affected in Parkinsons. By better understanding this cooperation between striatum and the release of dopamine from axons, we could provide new knowledge toward ways to restore normal function.
Hypothesis: We think that other molecules in the striatum play a very important role in controlling the release of dopamine, particularly for the types of dopamine axons that are most vulnerable in PD. We believe that this role is disrupted in the disease and could be targeted to rescue symptoms.
Impact on Diagnosis: Our discoveries will provide knowledge that may help to find new ways of treating Parkinsons using medicines that target the key signaling molecules in striatum that control dopamine release.
Leadership
Circuitry and Brain-Body Interactions | 2021
Also Check: How Long Does Parkinson’s Last
Parkinsons Disease Signs And Symptoms
The first symptom many people notice is a subtle tremor in their hands. However, research has found that Parkinsons disease can actually begin years or even decades before motor problems start. By the time motor-related symptoms appear, people with Parkinsons disease have already lost 50% of a specific type of dopamine cell found in the brain. They may also have experienced non-motor symptoms, such as sleep disturbances, sudden body movements or vocalizations, mood changes, anxiety, constipation and loss of smell.
This disease can progress to other parts of the body and increase in severity, leading to a loss of functional independence. Symptoms can include: trembling of hands or limbs, which typically starts on one side trouble making facial expressions quieter voice volume rigid muscles slowness or freezing of movement impaired balance or coordination depression or mood issues sleep problems and difficulty walking, completing tasks or remembering things.
People with Parkinsons disease can be more susceptible to illness and infection, and when they do get sick, it can cause their Parkinsons symptoms to worsen.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
