Managing Symptoms In The End Stage Of Parkinsons
Because of the degenerative nature of the disease, patients in the end stage of Parkinsons;are at severe risk of:;;
- Rashes;;
- Digestive Problems ;;
To avoid serious;complications, patients require 24-hour assistance. This includes:;;
- Shifting Them Every Two Hours. To prevent their weight from opening wounds on the skin.;;
- Toileting. Besides walking patients to the bathroom, caregivers need to help them undress and clean up afterwards.;;
- Changing Diapers. If the patient is confined to bed, their diapers need to be checked and changed every two hours to prevent excoriation .;;;
- Bathing & Grooming. If the patient cannot get to the shower, the caregivers will need to give them a sponge bath.;Patients will also need help trimming their nails, combing their hair, and brushing their teeth.;;
- Eating. Caregivers may have to push patients to eat, if they are able.;Because of difficulties chewing and swallowing, soft foods may be all they can eat at this stage. Oatmeal, scrambled eggs, yogurt, applesauce, mashed potatoes, and smoothies are;good choices.;If you serve solid;food, cut it into;small pieces to prevent choking.;;
- Drinking.;Patients need to drink 6-10 glasses of water a day to stay hydrated.;;
- Organizing Medication. Patients are usually prescribed several medications to reduce shakes and control movement.;Medications need to be carefully organized and all caregivers need to be briefed on their instructions.;;;
When is it Time;for;Hospice Care?
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinsons disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, ;bringing you peace of mind. The team is on call 24 hours a day even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
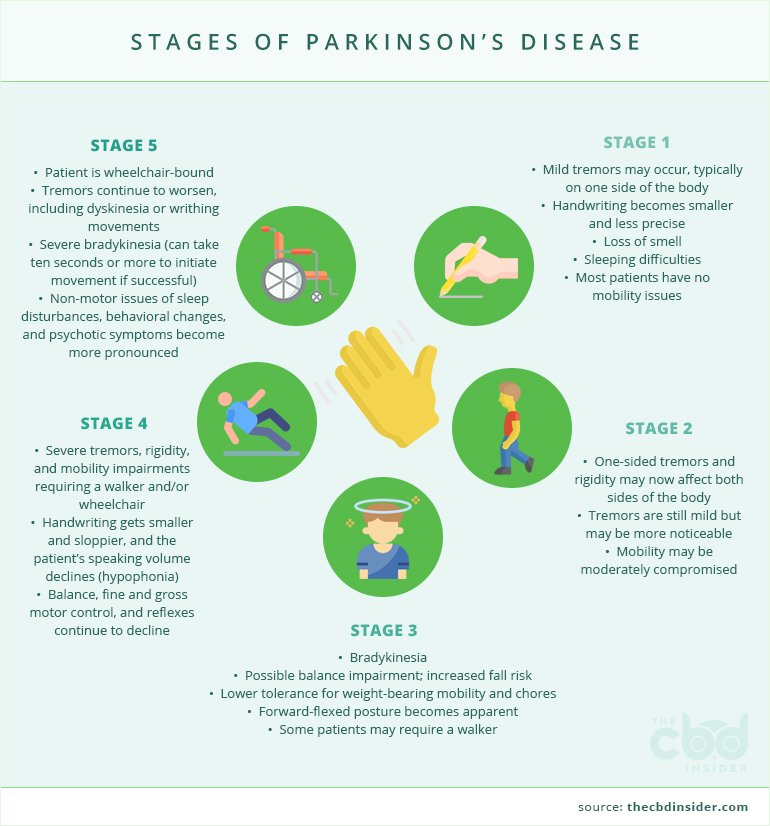
The Stages Of Parkinsons Disease
Stage One The Initial Stage: Symptoms are generally mild and may be easier to hide. Common symptoms include tremors, poor posture, balance issues, stooping of the back, and shaking of the limbs.
Stage Two Both Sides of the Body are Affected: The Parkinsons now affects both sides of the body, with increased symptoms that are more noticeable. Daily tasks become more difficult as symptoms now affect the entire body. It is harder to maintain your balance, walking becomes more difficult and tremors/shaking is more frequent.
Stage Three Increased symptoms & overall slowing down: By stage 3 the typical symptoms are more pronounced and the list of symptoms becomes more inclusive. One of the most noticeable changes is that movements and actions are much slower; including facial expressions, speech, and motor skills. It is common to common to feel light headed, fainting, and experience hypo-tension .
Stage Five The Final Stage: During the final stages the person will require 24/7 one on one care and nursing skills. By stage 5, hospice care for late stage Parkinsons is a necessity and will help everyone involved with the acceptance of the final stage of the disease.Our trained hospice providers will guide you through these final stages. Our goal is to focus on the patient and the family unit as a whole.
Read Also: How Long Can A Person Live With Parkinson’s Disease?
Cold Hands And Feet And Skin Mottling
Hands and feet may become colder and the skin may look blotchy and purplish . It happens because the heart is no longer able to pump blood as well. As a result, blood pressure goes down and the skin grows colder.
This mottling may slowly work its way up the arms and legs. The lips and nail beds can turn blue or purple too.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18;For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19;cyclizine, domperidone have all been suggested in PD.20;However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21;Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20;Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24;as well as for agitation at the end of life.20
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Parkinson’s Disease And Palliative Care
This page outlines the decline of Parkinson’s disease and helps those coping with Parkinson’s understand what a palliative care team provides. There is a brief discussion of when and how to get palliative care, an online quiz to determine if palliative care is right for your family and a link to a palliative care provider search tool.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Also Check: What Is Life Expectancy Of Parkinson’s Patients
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Hospice Care Late Stage Parkinsons
It is important to know your options for hospice care for late stage Parkinsons patients. Our article regarding in home health care for Parkinsons explains some of the basic facts and ideas to maintain quality of life once diagnosed. However, we offer specialized in home care from diagnosis through the final stages of the disease.
The Life of Parkinsons Crossing the bridges & facing forks in the road. Get the most out of life and adjust your lifestyle to make every day as good as possible.
Parkinsons disease is degenerative. Because the disease progresses with time there are basic stages that occur.
What Is Parkinson’s Disease
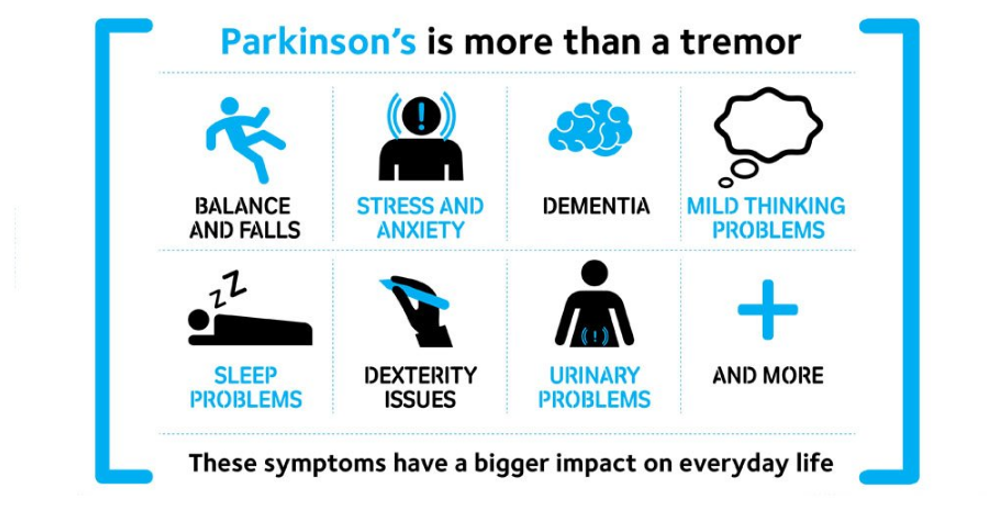
Parkinson’s disease is the second most common neurodegenerative disorder and the most common movement disorder. Characteristics of Parkinsons disease are progressive loss of muscle control, which leads to trembling of the limbs and head while at rest, stiffness, slowness, and impaired balance. As symptoms worsen, it may become difficult to walk, talk, and complete simple tasks.
The progression of Parkinson’s disease and the degree of impairment vary from person to person. Many people with Parkinson’s disease live long productive lives, whereas others become disabled much more quickly. Complications of Parkinsons such as falling-related injuries or pneumonia. However, studies of patent populations with and without Parkinsons Disease suggest the life expectancy for people with the disease is about the same as the general population.
Most people who develop Parkinson’s disease are 60 years of age or older. Since overall life expectancy is rising, the number of individuals with Parkinson’s disease will increase in the future. Adult-onset Parkinson’s disease is most common, but early-onset Parkinson’s disease , and juvenile-onset Parkinson’s disease can occur.
Don’t Miss: Parkinson Hereditary Risk
Can You Live With Parkinsons Without Medication
Medication aside, there are many ways people living with Parkinsons disease can improve their health and well-being, preserve physical function, ease symptoms and enhance quality of life. Chief among these are getting regular exercise, eating a healthy diet, staying hydrated and getting an adequate amount of sleep.
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
Also Check: Sam Waterston Parkinsons
What Does End Stage Parkinson’s Disease Look Like
In the final stage of Parkinson’s disease, patients are unable to perform basic movements without assistance and require one-on-one care, according to Healthline. Quality of life rapidly declines as sufferers become bedridden or wheelchair bound and experience worsening memory and speaking problems. Infections become more common and incontinence worsens. Sadly, medications and treatments provide little or no relief to patients in this stage of the disease.
The progression of Parkinson’s disease is divided into five stages, with the disease increasing in severity as the number of the stage increases, explains Healthline. The speed of progression of the disease and specific symptoms vary from patient to patient.
In stage one, Parkinson’s patients experience mild symptoms that affect only one side of the body, such as tremors or shaky limbs, notes Healthline. In stage two, motor symptoms begin to affect both sides of the body, and patients may start to experience difficulty walking and maintaining balance. Stage three is considered moderate Parkinson’s disease, and patients in this stage typically have difficulty performing basic physical movements, but can still function on their own without assistance. In stage four Parkinson’s disease, patients begin to experience severe, disabling symptoms and often cannot live on their own without a caregiver. Stage five is the end stage of Parkinson’s disease.
What Symptoms Can Be Expected In Advanced Pd
- Pain 86%
- Shortness of breath 54%
- Problems in swallowing 40%14
In an analysis of 339 death certificates and medical notes in the UK, pneumonia was found to be a terminal event in 45%.13
Caregiver distress with choking and the risk of choking to death is also mentioned in a separate study in to experiences regarding all stages of PD.4
In a survey of symptoms and their association with quality of life, in those patients with advanced disease, uncontrolled pain, anxiety and hallucinations were significantly associated with poor quality of life.9
Seizures are also noted in a description of the last phase of Parkinsonian syndromes,15;and in retrospective studies of PD patients overall.16,17
These above symptoms often occur on the background of weight loss, pain, and cognitive impairment. It is important therefore to note which medications given at the end of life may exacerbate these symptoms, and which should be considered in anticipation of them.
You May Like: Can Parkinson’s Change Your Personality
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
What To Expect In The Late Stages Of Alzheimers Disease
What To Expect In The Late Stages Of Alzheimers Disease
As Alzheimers advances into the later stages, caregivers and family members can expect quite a few new symptoms of the disease. Fortunately, being prepared now can help people better cope with the challenges of the late stages of Alzheimers.
Although the disease doesnt affect every person the same way, informed caregivers can often reduce later stage crisis. Read our list of the symptoms to expect in the late stages of Alzheimers to better prepare for tomorrow, today.
Recommended Reading: Average Life Expectancy For Parkinson Disease
Pharmacologic Issues At End
As PD progresses there are fewer dopaminergic neurons in the substantia nigra as well as a progressively lower capacity to store exogenous levodopa and convert it to dopamine for storage and release in the remaining neurons. Additionally, as the dose requirements of levodopa increase, the patient’s functioning is inhibited before his next dose of medication . This usually takes place 24 hours after a levodopa dose and may appear as sensory , psychiatric or autonomic symptom, or progression of motor symptoms or dystonia . This is called end of dose wearing off. Wearing off has not been fully explored, but may be connected to pharmacokinetic changes, and shortening of striatal levodopa half-life resulting from progressive degeneration of nigrostriatal dopaminergic terminals . To treat motor symptoms it is necessary to deliver medication effectively. Patients with advanced PD often notice that protein-rich meals will diminish the effectiveness of levodopa doses . This can be alleviated by reducing protein intake during daytime and limiting protein intake at night to 40 grams . There are some strategies to Improve absorption of Levodopa include: advise patients to take levodopa before meals, on an empty stomach , advise patients to avoid protein-rich meals and bulk-forming foods , advise patients against lying down, and encourage them to move around, after ingesting a dose , and advise patients to mix levodopa, crushed into a powder, into sparkling liquid .
