Why Should I Participate In A Clinical Study
We can only reach breakthroughs in treatment and care if people participate in the studies.
Participating is safe and can help you
Every clinical study is reviewed thoroughly before your doctor asks you to participate. Clinical trials carry some risks, but your doctor is required by law to explain the risks to you clearly and make sure that you understand them. If your doctor tells you about the risks of participating in the study, ask yourself, What are the risks of not participating in the study? Most of the time, if you balance the possible benefits from participating against the risks, it is about the same as the risks of not being in the study.
On the other hand, the study may be of a new drug or treatment that could help you. If you dont participate, it may be years before you have a chance to try that drug.
Some people do not participate because there is no guarantee they will get the experimental therapy they might get the placebo. Again, think carefully about the risks and benefits of entering the study and getting the new treatment, entering the study and getting the placebo or not entering the study at all.
Your participation can help others
If you have PD or any other disease, the drugs, procedures and therapies you use now were scientifically tested, likely by thousands of volunteers. Participating in a clinical trial is your way to pay it forward for people diagnosed with Parkinsons in the future.
Diagnosis Of Parkinsons Disease
There are currently no blood or laboratory tests to diagnose non-genetic cases of Parkinsons. Doctors usually diagnose the disease by taking a persons medical history and performing a neurological examination. If symptoms improve after starting to take medication, its another indicator that the person has Parkinsons.
A number of disorders can cause symptoms similar to those of Parkinsons disease. People with Parkinsons-like symptoms that result from other causes, such as multiple system atrophy and dementia with Lewy bodies, are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinsons, certain medical tests, as well as response to drug treatment, may help to better evaluate the cause. Many other diseases have similar features but require different treatments, so it is important to get an accurate diagnosis as soon as possible.
How Parkinsons Disease Is Diagnosed
Parkinsons disease is usually diagnosed clinically, meaning that a physician looks for the presence or absence of the possible symptoms of Parkinsons disease by interviewing the patient and performing a detailed neurologic examination.
While there is presently no definitive test for Parkinsons, it can often be identified by a general neurologist, who is trained to diagnose and treat neurologic disorders. To avoid misdiagnosis, consultation with a movement disorder specialist is recommended. A movement disorder specialist is a physician who has undergone additional, subspecialty training in the diagnosis and treatment of movement disorders, such as Parkinsons, after training in general neurology.
What to expect during your visit with a physician
Typically, a trained physician will only consider the diagnosis of Parkinsons disease if the person being examined has at least two of the core motor symptoms of Parkinsons, including tremor, the characteristic bradykinesia , or rigidity. At the end of your visit, the physician should discuss with you why you may or may not have Parkinsons disease and the level of certainty about the diagnosis. This determination is based on your medical history and examination at this visit.
Brain imaging and other tools to aid diagnosis of Parkinsons
Don’t Miss: What Are The Side Effects Of Parkinson’s Medication
The Promising Treatments In The 2022 Parkinsons Clinical Trials Pipeline
Posted:
As we know the Parkinsons research community is hard at work to find therapies and treatments to improve the quality of life of Canadians living with Parkinsons and ultimately find a cure. An article outlining the current clinical trials pipeline for Parkinsons was recently published in the Journal of Parkinsons Disease. Here are some of the key highlights. For a refresher on clinical trials and what happens in each phase, here is a helpful FAQ.
As of January 2022, there were nearly 150 Parkinsons therapies active in the clinical trial pipeline:
- 50 products in Phase I
- 65 products in Phase II
- 17 products in Phase III
Most of the drugs in trials are for managing the symptoms of Parkinsons . Developments in disease-modifying treatments the types of treatment that change the course of Parkinsons progression have been slow to emerge. However, in 2022, there are 54 disease-modifying treatments in trial phases, with three graduating to Phase III trials!
Below youll find a brief overview of whats happening in each phase of the trials.
New Treatment For Slowness & Stiffness In Parkinsons Disease
In 2018, Focused Ultrasound was approved to treat tremors in people with PD. Now, the FDA has approved expanding the indications of Focused Ultrasound for Parkinsons disease to also include treatment of bradykinesia rigidity , and dyskinesias.
Individual ultrasound waves do not contain enough energy to do any damage as they pass through a patients skull and brain tissue. But with FUS, multiple waves are all focused on a particular spot so that a lesion is intentionally formed, thus disrupting the circuitry thats causing the issue. During the FUS procedure, MRI technology is used to precisely visualize the brain areas of interest. Previously, a deep-brain structure called the thalamus was targeted that was able to treat the tremor of PD. Now, by targeting of a deep-brain structure called the globus pallidus interna FUS can treat an expanded array of PD symptoms.
Its important to note that FUS will not slow the progression of PD, but it can help manage the symptoms of the disease and improve quality of life. In this way, it is similar to deep brain stimulation , a surgery in which a wire is inserted into deep-brain structures to manipulate the abnormal PD circuitry. Prior to the advent of DBS, lesioning surgery of deep-brain structures was used to treat the symptoms of PD. Today, FUS can perform approximately the same role as lesioning surgery but in a much less invasive way.
Don’t Miss: Does A Dat Scan Confirm Parkinson’s
New Treatment Provides Freedom For Patient
Two advocates of Duopa are Parkinsons patient George Connors and his wife, Kay, of Randleman, North Carolina.
Among the first participants in the clinical trial at Wake Forest Baptist, he has been taking Duopa for more than 5 years now.
Its been a lifesaver, his wife said. It has made it easier for him to get up and do things.
Kay said the unreliable action of levodopa pills made it difficult for her husband to pursue activities he loved. But with Duopa, she said, he goes fishing, mows the yard and does outside work, all without having to remember when to take the pills.
George gave one example of how Duopa works better for him than pills. He said it used to take him as much as an hour each morning to stand up properly because his toes would cramp overnight and the levodopa pills were slow to work. With the Duopa pump system, he said, his toe cramps are gone within minutes.
Siddiqui said that new drugs and new delivery methods for existing drugs can relieve many of the symptoms experienced by people with Parkinsons and that ongoing research holds hope for the future.
Out of all the neurological diseases, we are finding Parkinsons to have more and more treatments available, he said.
What Kinds Of Genetic Research Is Being Done
Researchers are investigating genes that code proteins responsible for producing dopamine. By increasing the amount of dopamine in the brain, Parkinsons symptoms can be minimized if not prevented.
What other treatments are being researched?
- Drug treatments. Researchers are investigating drugs that block the action of glutamate, an amino acid that destroys nerve cells, as well as the role of the antioxidant coenzyme Q-10 in slowing the progression of Parkinsons disease.
- Neural growth factor. Preliminary studies have shown that neural growth factor revives the dormant cells needed to produce dopamine, dramatically improving symptoms.
- Deep brain stimulation. Research is underway to better understand how deep brain stimulation works in Parkinsons disease. Researchers are also studying improved ways of stimulating the brain.
Show Sources
Don’t Miss: How Young Can Parkinson’s Start
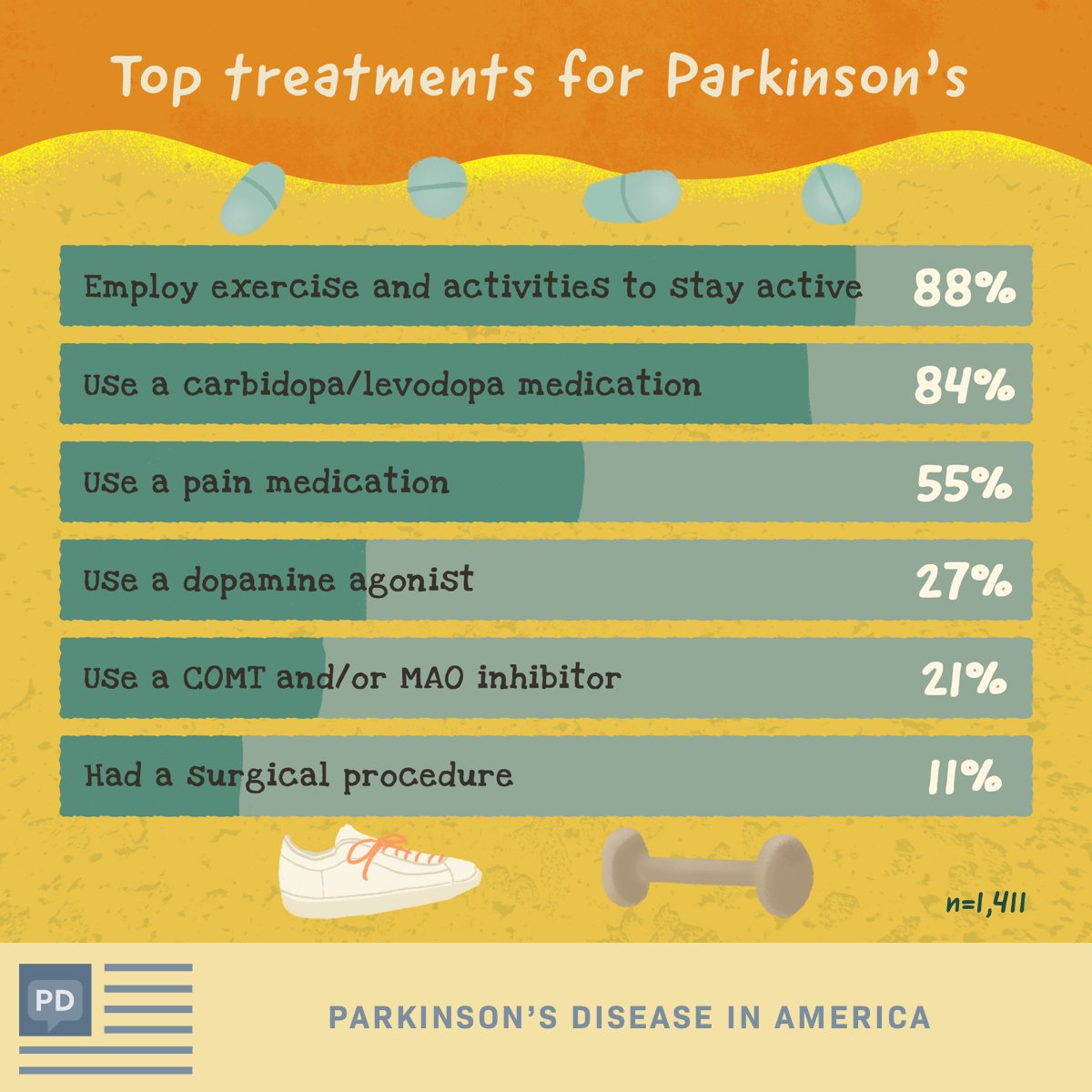
Searching To Control Symptoms: New Methods Of Delivery
In recent months, symptomatic treatment of PD has had some new developments as well. A new drug for PD, rotigotine, has been introduced in Europe and elsewhere as Neupro. This compound is a dopaminergic agonist, a class of drugs that also includes drugs that have been available for many years in the U.S., including Mirapex, Requip, and Permax . Neupro is unique in how it is delivered: it is absorbed through the skin and so has been marketed as a transdermal patch with continuous delivery over 24 hours. So far, experience with Neupro suggests that it is effective and well tolerated. However, whether this drug or its unique mode of delivery will offer a significant advantage over currently marketed medications of the same class still remains to be learned.
PD still presents many challenges for the medications of the future. Among the unmet needs are ways to reverse the problem of imbalance, especially falling backward. The flexed posture of PD, swallowing and speech difficulties, and situation-specific freezing are all challenges for improved drug therapy. Scientists have not yet determined where in the brain and what types of biochemical disturbance underlie these problems.
Also Check: What Are The Signs Symptoms Of Parkinsons Disease
New Treatment For Parkinsons Disease
This fall, the Montreal Neurological Institute and Hospital expects to introduce a previously unavailable form of treatment for Parkinsons disease patients. Although the treatment will be limited to patients who fulfill specific criteria, the treatment has been shown to be effective in Europe, where it has been available for more than a decade.
The treatment involves administering the drug Duodopa directly into the patients small intestine via the stomach through a tube. The drugs dosage is controlled by a mini-pump weighing about half a kilogram that the patient wears at the waist. The body transforms levodopa to dopamine to increase the amount of dopamine in the brain. Parkinsons disease symptoms are linked to dopamine levels. Carbidopa helps to guide levodopa to the brain and also helps to avoid stomach upset and other undesirable side effects of levodopa.
The benefit of the Duodopa treatment is that the patient gets the drug continuously and so avoids the kinds of fluctuations that can come when drugs are taken orally at intervals during the day. Some patients have difficulty swallowing, and with this treatment, theres no need to swallow, says Dr. Anne-Louise Lafontaine, a neurologist and Director at The Neuros Movement Disorder Clinic.
Not all Parkinsons disease patients will qualify for the treatment.
This article was submitted by Neuro staff
Dont Miss: Do Parkinsons Tremors Come And Go
You May Like: How To Stop Parkinson’s Freezing
Where Is Drug Development Headed
Overall, experts say the Parkinsons disease field aims to develop therapies that can slow or stop disease progression. Kordower notes several promising gene therapy and stem cell therapy approaches are entering the early stages of clinical development.
Most ongoing PD trials are at the Phase II stage, according to GlobalDatas Clinical Trial Database. While institutions are sponsoring 84 trials of the 133 ongoing Phase II studies , pharma companies are running 44 trials of the 56 ongoing Phase I studies .
As the field awaits results from the slew of ongoing trials, experts agree that the PD trials reading out in the remainder of 2022 could have a substantial impact. These four trials are all very timely, Eidelberg says. The community of movement disorder specialists and neurologists would use these drugs because the indications were talking about are really very common.
Related Companies
What Is Parkinsons Disease
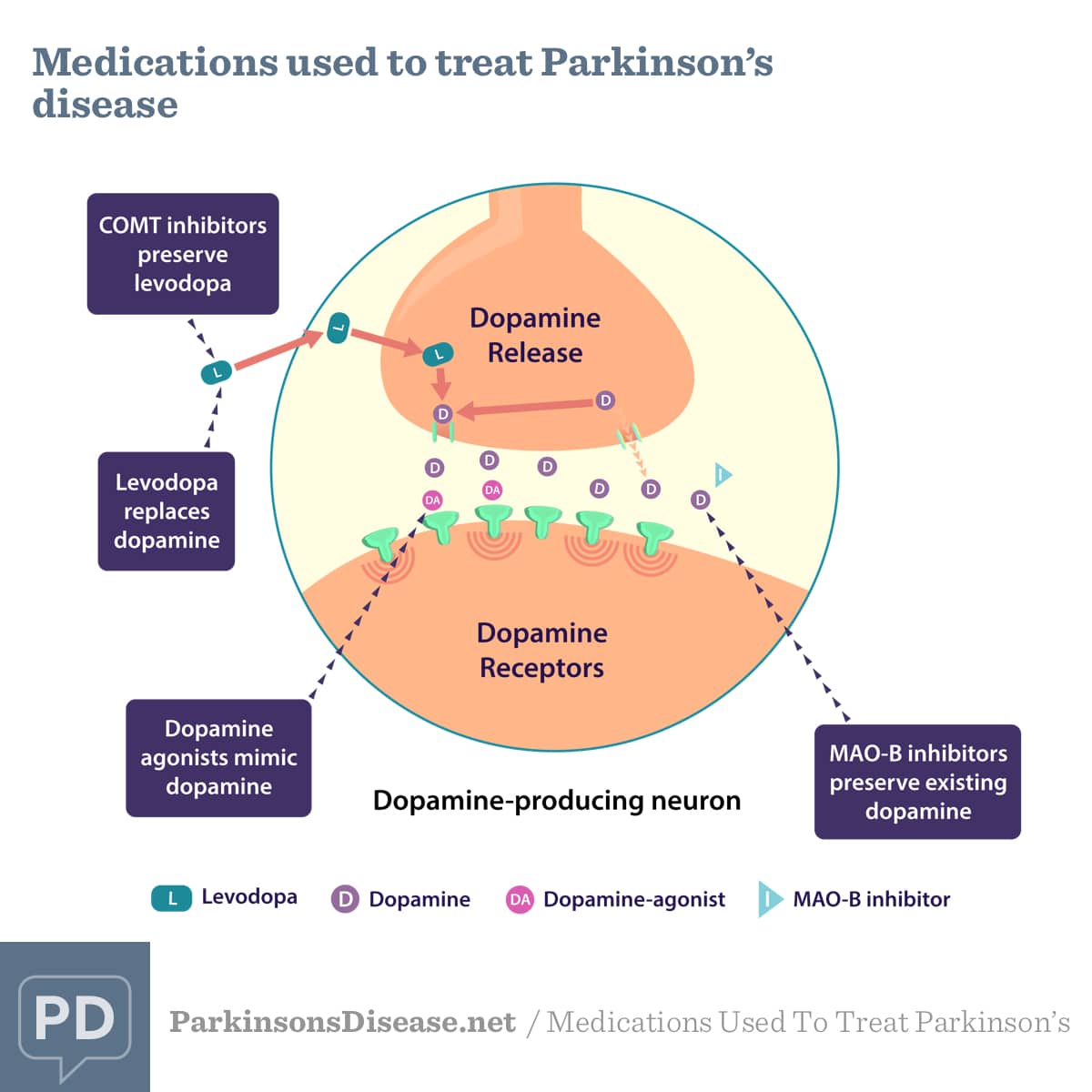
Parkinsons disease is a progressive brain disorder that causes shaking and muscle stiffness, and slows movement. It develops when neurons in a particular part of the brain stop working properly and are lost over time. These neurons produce an important chemical called dopamine. Dopamine is used by the brain to send messages across brain areas to help control movement. Eventually, the brain cannot make enough dopamine to control the movement properly.1,2
You May Like: Parkinson’s Dementia Support Group
What Are Off Episodes
Firstly, its important to understand what OFF episodes are and why they happen. OFF episodes are defined as a temporary returning of Parkinsonian symptoms such as tremor, rigidity, loss of postural reflexes and memory problems, while taking levodopa medication. OFF episodes affect the majority of people with PD, and it can occur at any stage of the illness.
Some patients experience OFF episodes when they first wake in the morning known as akinesia while others notice symptoms returning at the end of a dose when the drug starts to wear off. For some, the OFF episodes are random and severe. Uncontrolled Parkinsons symptoms can significantly impact your quality of life, which is why scientists are committed to finding new and improved treatment options.
Advanced And Future Treatments For Parkinsons
While theres no cure for Parkinsons disease, recent research has led to improved treatments.
Scientists and doctors are working together to find a treatment or prevention technique. Research is also seeking to understand who is more likely to develop the disease. In addition, scientists are studying the genetic and environmental factors that increase the chance of a diagnosis.
Here are the latest treatments for this progressive neurological disorder.
In 2002, the FDA approved deep brain stimulation as a treatment for Parkinsons disease. But advances in DBS were limited because only one company was approved to make the device used for the treatment.
In June 2015, the FDA approved the
You May Like: Sam Waterston Tremor
Read Also: Do You Die From Parkinson’s Disease
Designer Neurons Offer New Hope For Treatment Of Parkinson’s Disease
- Date:
- Arizona State University
- Summary:
- Scientists describe a process for converting non-neuronal cells into functioning neurons able to take up residence in the brain, send out their fibrous branches across neural tissue, form synapses, dispense dopamine and restore capacities undermined by Parkinson’s destruction of dopaminergic cells.
Neurodegenerative diseases damage and destroy neurons, ravaging both mental and physical health. Parkinson’s disease, which affects over 10 million people worldwide, is no exception. The most obvious symptoms of Parkinson’s disease arise after the illness damages a specific class of neuron located in the midbrain. The effect is to rob the brain of dopamine — a key neurotransmitter produced by the affected neurons.
In new research, Jeffrey Kordower and his colleagues describe a process for converting non-neuronal cells into functioning neurons able to take up residence in the brain, send out their fibrous branches across neural tissue, form synapses, dispense dopamine and restore capacities undermined by Parkinson’s destruction of dopaminergic cells.
The current proof-of-concept study reveals that one group of experimentally engineered cells performs optimally in terms of survival, growth, neural connectivity, and dopamine production, when implanted in the brains of rats. The study demonstrates that the result of such neural grafts is to effectively reverse motor symptoms due to Parkinson’s disease.
New perspectives on Parkinson’s disease
Parkinsons Treatment On The Horizon
Immunotherapy: Researchers at the Columbia University Medical Center and the La Jolla Institute for Allergy and Immunology have found evidence that autoimmunityin which the immune system attacks the bodys own tissuesplays a role in Parkinsons disease. The findings raise the possibility that the death of neurons in Parkinsons could be prevented by therapies that dampen the immune response.
Our findings raise the possibility that an immunotherapy approach could be used to increase the immune systems tolerance for alpha-synuclein, which could help to ameliorate or prevent worsening symptoms in Parkinsons disease patients, says study co-leader Alessandro Sette, Dr. Biol. Sci., professor in the Center for Infectious Disease at La Jolla Institute for Allergy and Immunology in La Jolla, Calif. The study was published in Nature.
The idea that a malfunctioning immune system contributes to Parkinsons dates back almost 100 years, said study co-leader David Sulzer, PhD, professor of neurobiology at CUMC. But until now, no one has been able to connect the dots. Our findings show that two fragments of alpha-synuclein, a protein that accumulates in the brain cells of people with Parkinsons, can activate the T cells involved in autoimmune attacks.
This is the strongest evidence we have so far that a drug could do more than provide symptom relief for Parkinsons disease, says the studys senior author, Professor Tom Foltynie .
Dont Miss: Sam Waterston Parkinsons
Read Also: How To Lose Weight With Parkinson’s Disease
Why Scientists Believe Theyve Made New Breakthrough In Parkinsons Disease Treatment By Building On Gdnf Research
The Finnish researchers are now working to improve the properties of BT13 to make it more effective as a potential treatment that could benefit many people living with the disease.
The study, which was published online yesterday in the journal Movement Disorders, builds on previous research on another molecule that targets the same receptors in the brain.
GDNF or glial cell line-derived neurotrophic factor is an experimental treatment for Parkinsons discovered in 1993 that has been shown to bring dying brain cells back to life and particularly effective in dopamine neurons.
It was the subject of a BBC documentary in February 2019 that followed a phase two trial in Bristol involving 42 patients. While the results werent clear cut, GDNF has shown promise to restore damaged cells in people with Parkinsons.
However, the GDNF protein requires complex robot-assisted surgery to deliver the treatment to the brain because its a large molecule that cant cross the blood-brain barrier a protective wall that prevents some drugs from getting into the brain.
BT13 is a smaller molecule that is able to cross the blood-brain barrier and therefore could be more easily administered as a treatment if shown to be beneficial in further clinical trials.
Dr Yulia Sidorova, lead researcher on the study, said: We are constantly working on improving the effectiveness of BT13.
Our ultimate goal is to progress these compounds to clinical trials in a few coming years.
Related Article
