Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinsons disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the persons symptoms strongly suggest to the physician that idiopathic Parkinsons disease is the correct diagnosis.
Helping diagnose Parkinsons with DaTscan and other tests
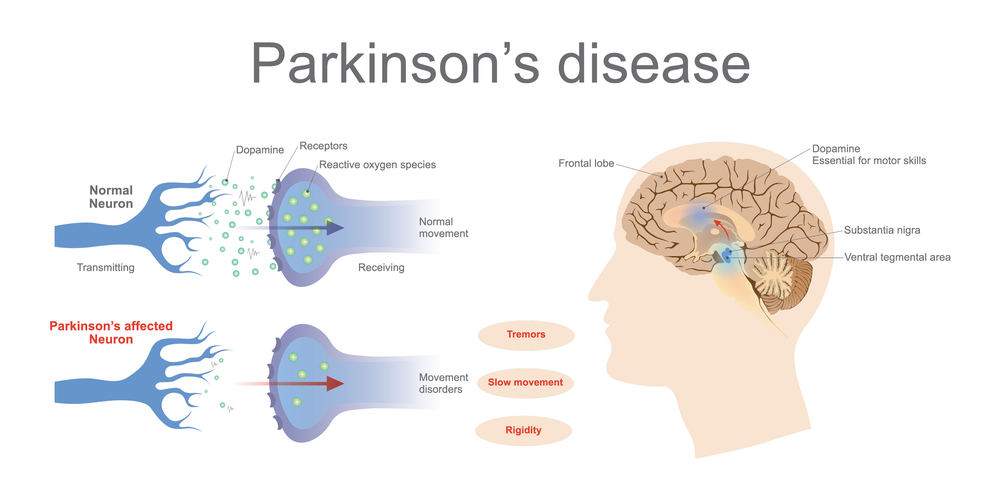
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinsons. Imaging studies to evaluate Parkinsons disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinsons disease from certain other neurologic disorders. Most physicians offices will have access to MRI however, DaTscan imaging may only be available at larger hospitals or medical centers.
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinson’s disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinson’s is caused by a combination of environmental and genetic factors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinsons disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
Recommended Reading: Can Adderall Cause Parkinson’s
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
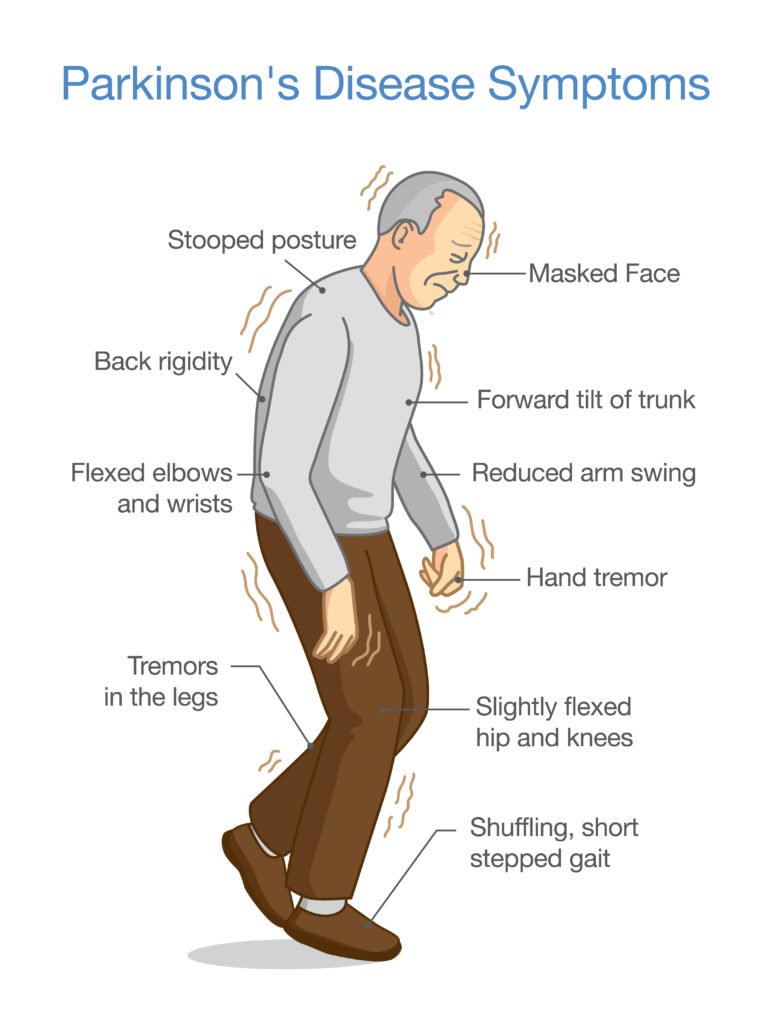
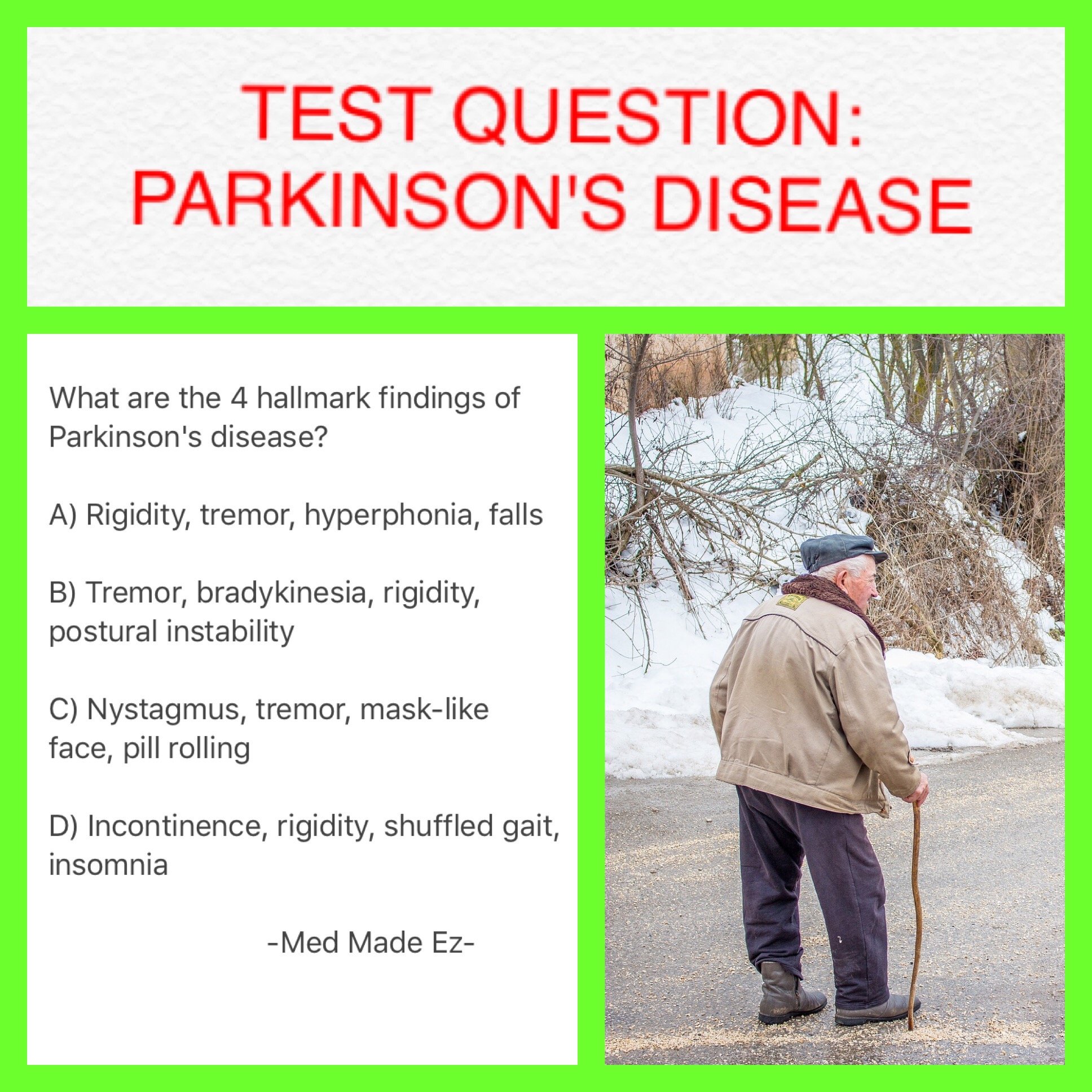
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Stooping Or Hunching Over
Are you not standing up as straight as you used to? If you or your family or friends notice that you seem to be stooping, leaning or slouching when you stand, it could be a sign of Parkinson’s disease .
What is normal?If you have pain from an injury or if you are sick, it might cause you to stand crookedly. Also, a problem with your bones can make you hunch over.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Passive Manipulation Of Limbs
To test for the presence of rigidity, we need to passively manipulate the limbs of the patient. However, If the disease is in its early stage or the symptoms are well controlled with medications, we may not be able to see rigidity. We will need to use some activation maneuvers, that basically consist in performing repetitive movements with the limb contralateral to the one that is being tested.
Also, there are two types of rigidity:
– Lead-pipe rigidity: where the tone is uniformly and smoothly increased throughout the entire range of movement
– Cogwheel rigidity: where a tremor is superimposed on the hypertonia, making the movement irregular due to intermittent increase and reduction of tone
Upper Extremity Testing
For the upper extremity the most sensitive joint where to check for rigidity is the wrist. To uncover rigidity, passively rotate the wrist and feel for a resistance to the movement. It is very important that the arm of the patient is fully relaxed when rotating the wrist. To do this, place your proximal hand under the patients forearm, while your distal hand grabs and rotates the wrist of the patient. When rigidity is present, the range of motion will be preserved but you will feel a resistance in performing the movement.
Wrist rotation with activation maneuver.
It is also possible to test for rigidity in the elbow by passively flexing and extending the forearm.
Elbow flexion-extension with activation maneuver.
Lower Extremity Testing
What Is Parkinsons Disease
Parkinsons disease is a progressive brain disorder that affects mobility and mental ability. If you or a loved one has been diagnosed with Parkinsons, you may be wondering about life expectancy.
According to some research, on average, people with Parkinsons can expect to live almost as long as those who dont have the condition.
You May Like: Parkinsons Disease Hereditary
Determining Diagnosis Through Response To Parkinsons Medication
If a persons symptoms and neurologic examination are only suggestive of Parkinsons disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinsons disease to provide additional information. In the case of idiopathic Parkinsons, there is typically a positive, predictable response to Parkinsons disease medication in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
How A Diagnosis Is Made
The bedside examination by a neurologist remains the first and most important diagnostic tool for Parkinsons disease . Researchers are working to develop a standard biological marker such as a blood test or an imaging scan that is sensitive and specific for Parkinsons disease.
A neurologist will make the diagnosis based on:
- A detailed history of symptoms, medical problems, current and past medications. Certain medical conditions, as well as some medications, can cause symptoms similar to Parkinsons.
- A detailed neurological examination during which a neurologist will ask you to perform tasks to assess the agility of arms and legs, muscle tone, gait and balance, to see if:
- Expression and speech are animated.
- Tremor can be observed in your extremities at rest or in action.
- There is stiffness in extremities or neck.
- You can maintain your balance and examine your posture.
Also Check: How Quickly Does Parkinson’s Disease Progress
What Is Rem Behavior Disorder And How Is It Connected To Parkinson’s
A: REM behavior disorder is different than other sleep problems, like insomnia. People who have it may jerk or kick it’s as though they are acting out their dreams. In a similar pattern to anosmia, people with idiopathic REM sleep behavior disorder have at least a 50 percent chance of eventually developing Parkinson’s disease.
How Is Parkinson’s Disease Diagnosed
Diagnosis is difficult at every stage of the disease, but particularly in the early stages. No single test can provide a diagnosis. A diagnosis will likely involve physical and neurological examinations, conducted over time to assess changes in reflexes, coordination, muscle strength, and mental function. Your doctor might also see how you respond to medicine.
You may need to have brain imaging tests to rule out other conditions that might be causing your symptoms. Such tests could include MRI and CT scans and possibly some other types of scans. Blood tests may also be done to exclude other illnesses.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
When To Seek Hospice Care
When you or your loved one have a life expectancy of six months or less, you become eligible for hospice care a type of comfort care provided at the end of life for someone living with end-stage Parkinsons disease. Hospice provides extra support so your loved one can live as comfortably as possible.
If you have experienced a significant decline in your ability to move, speak, or participate in activities of daily living without caregiver assistance, its time to speak with a hospice professional.
Read more: What is hospice care?
Some of the things that determine whether your loved one with end-stage Parkinsons is eligible for hospice include: difficulty breathing, bed bound, unintelligible speech, inability to eat or drink sufficiently, and/or complications including pneumonia or sepsis.
If you live in South Jersey, our nurse care coordinator can answer your questions and decide if your loved one is ready for hospice care. Call us 24/7 at 229-8183.
Managing Depression In Parkinsons Disease
People with Parkinsons, family members and caregivers may not always recognize the signs of depression and anxiety. If you are experiencing depression as a symptom of Parkinsons, it is important to know it can be treated.
Here are some suggestions:
- For information and support on living well with Parkinsons disease, contact our Information and Referral line.
- As much as possible, remain socially engaged and physically active. Resist the urge to isolate yourself.
- You may want to consult a psychologist and there are medications that help relieve depression in people with Parkinsons, including nortriptyline and citalopram .
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Imaging And Lab Tests
Your doctor may order some imaging tests and laboratory tests. Imaging tests can include computed tomography scans and magnetic resonance imaging scans. Laboratory tests can include blood tests and urine tests.
While these tests and scans will not help diagnose Parkinsons disease, they can help rule out other conditions that have similar symptoms.
Your doctor may also suggest that you get a dopamine transporter scan . This scan requires a single-photon emission computed tomography scanner. It involves an injection of a small amount of a radioactive drug so that your doctor can study the dopamine systems in your brain .
While a DaTscan cannot conclusively prove that you have Parkinsons, it can help confirm your doctors diagnosis and eliminate other conditions.
What You Can Expect
Parkinson does follow a broad pattern. While it moves at different paces for different people, changes tend to come on slowly. Symptoms usually get worse over time, and new ones probably will pop up along the way.
Parkinsonâs doesnât always affect how long you live. But it can change your quality of life in a major way. After about 10 years, most people will have at least one major issue, like dementia or a physical disability.
Don’t Miss: Does Restore Gold Work For Parkinson’s
Single Photon Emission Computed Tomography
In single photon emission computed tomography , a gamma ray-emitting radioactive isotope is tagged to a molecule of interest , which is given to the person with by intravenous injection. The labelled cocaine derivatives 123I–CIT and 123I-FP-CIT tropane) have most commonly been used, although only the latter is licensed in the UK. These label the presynaptic dopamine re- site and thus the presynaptic neurone, which can be visualised in two-dimensional images. These demonstrate normal uptake in the caudate and putamen in controls and in people with essential tremor, neuroleptic-induced parkinsonism or psychogenic parkinsonism, but reduced uptake in those with PD, PD with dementia, or .
How useful is SPECT in discriminating from alternative conditions?
Theories About What Causes Parkinsons
The cause of Parkinsons disease is still unknown, although there is some evidence for the role of genetics, environmental factors, or a combination of both. It is also possible that there may be more than one cause of the disease. Scientists generally believe that both genetics and environment interact to cause Parkinsons disease in most people who have it.
Currently, there is an enormous amount of research directed at producing more answers about what causes Parkinsons disease and how it might be prevented or cured. When physicians diagnose Parkinsons, they often describe it as idiopathic . This simply means that the cause of the disease is not known.
Read Also: What Color Is The Ribbon For Parkinson’s
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229
Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
Read Also: How Do You Beat Parkinson’s Fatigue
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinsons disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
From Evidence To Recommendation
The pathological studies emphasise the need for particular care in making a clinical diagnosis of . There is limited evidence to suggest that the UK Brain Bank Criteria have adequate sensitivity and specificity in comparison with post-mortem findings. The accuracy of diagnosis using the Brain Bank criteria increases as the condition progresses.
The availability of brain tissue has fostered much valuable research in recent years and should be encouraged in the future. Diagnostic information derived from post-mortem examination can also be of value to the families of individual patients.
RECOMMENDATIONS
- R9.
-
should be diagnosed clinically and based on the UK Parkinsons Disease Society Brain Bank Criteria.
- R10.
-
Clinicians should be encouraged to discuss with patients the possibility of tissue donation to a brain bank for purposes of diagnostic confirmation and research.
Recommended Reading: Parkinson’s Ribbon
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
