Mild Traumatic Brain Injury
Severe traumatic brain injury is a wellestablished risk factor for neurodegenerative diseases, including PD. Recent studies have focused on the role of mild TBI as a risk factor for neurodegenerative disease. A metaanalysis looked at the association between mild TBI and the development of neurological and psychiatric disease.68 Fourteen casecontrol studies and one cohort study were evaluated for the association between mild TBI and PD. A summary relative risk of OR 1.45 for mild TBI was found. An increased risk of PD with TBI was largely noted in the casecontrol studies and not in the cohort study. This was probably due to a limited number of patients in the cohort study and the fact that it only included head injury patients with a loss of conciousness.69 The two Asian studies in this metaanalysis noted an increased PD risk with head injury .70, 71 However, in both these studies, patient numbers were small and it could not be ascertained whether the reported head injury was also accompanied by loss of consciousness. Findings from another metaanalysis were similar.72 The definition of mild TBI is highly heterogeneous across the different studies , with few highquality studies73 and reverse causation have been hypothesized to lead to the reported positive associations.74 A recent large interviewbased casecontrol study performed in Denmark did not find an association between head trauma and PD.75 The risk of PD following mild TBI remains unclear .
The Future Of Parkinson’s Disease Epidemiology
In the next halfcentury, the average age of individuals in both developed and developing countries is expected to show a progressive increase. In the USA alone, this phenomenon of population aging is predicted to result in a three to fourfold increase in PD frequency, or several million persons with the disease. The impact of PD can also be expected to affect diseaseassociated health expenditures, lost income and personal suffering. As described in this chapter, despite intensive research efforts during the past several decades, the cause of typical PD remains unknown. Likely, PD will be understood to be multifactorial, and both genetic and environmental determinants will be important. For example, estimated lifetime penetrance in parkinsonism caused by LRRK2 in the Ashkenazi Jewish population is only about 30% . Both genetic and environmental factors may determine expression of this monogenic form of parkinsonism. Typical PD may similarly be due to many different combinations of genetic or environmental determinants. The investigation of possible geneenvironment interaction in PD is just beginning. In the next decade, investigations involving careful characterization of genetic and environmental factors will be essential to defining the causes of PD.
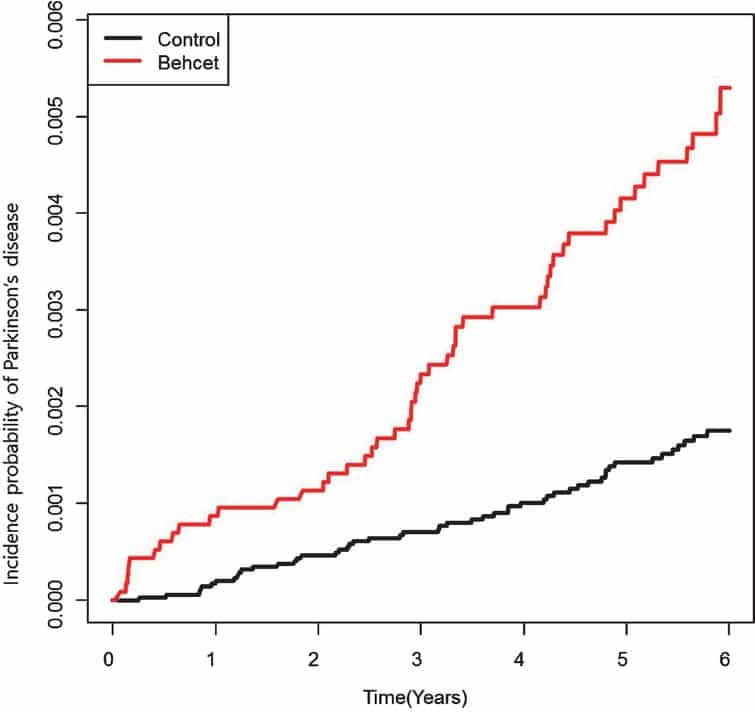
Patient Selection And Diagnostic Criteria
We selected all PD patients registered in the RID program during the 6-year study period. The diagnostic criteria for PD established by the NHI in the RID program are similar to the UK PD society brain bank clinical diagnostic criteria, and are as follows: 1) diagnosis of Parkinsonian syndrome : mild or worse bradykinesia and at least one of the following: muscular rigidity, rest tremor, postural instability 2) the exclusion criteria for PD: history of strokes, head injury, definite encephalitis, drug side effects, and hypoxia 3) supportive prospective positive criteria for PD: three or more required for diagnosis of definite PD in combination with step one: unilateral onset, rest tremor present, progressive disorder, persistent asymmetry affecting the side of onset most, excellent response to levodopa, severe levodopa-induced chorea, levodopa response for 5years or more, clinical course of 10years or more.
The database did not contain any personal identifiers as all identifiable personal information in the database was removed to comply with the privacy rules of the health insurance portability and accountability act. Informed consent was not required for this study as all the data was obtained from medical records. This study was performed based on the ethical principles of the Declaration of Helsinki of the World Medical Association. All procedural and ethical aspects of this study were approved by the Institutional Review Board of Korea University Ansan Hospital .
Also Check: Does Alcohol Affect Parkinson Tremors
Regional Analysis Of Trends
Table and Fig. show the trends in age-and sex-standardized incidence and prevalence of PD per 100,00 individuals by 17 regions from 2010 to 2015. During this period, the age-and sex-standardized incidence of PD increased in all regions of the country except for Sejong-si. Sejong-si was separated from provinces Chungbuk and Chungnam as a new administrative metropolitan city in 2012. Gyeongbuk and Jeonbuk experienced the largest increase in the incidence of PD from 2010 to 2015. The incidence ratios of these two regions were 1.6 and 1.5, respectively. The highest incidence of PD was recorded in Jeju in 2010 and Jeonbuk in 2015.
Table 3 Age-and sex-standardized incidence and prevalence per 100,000 population by region from 2010 to 2015Fig. 4
Regional trends in age- and sex-standardized incidence and prevalence per 100,000 population from 2010 to 2015. a Incidence in 2010, b Incidence in 2015, c Prevalence in 2010, d Prevalence in 2015.
The age-and sex-standardized prevalence of PD increased in all regions from 2010 to 2015. The largest increase was recorded in Jeonbuk with a prevalence ratio of 1.4 from 2010 to 2015. The highest prevalence of PD was in Seoul in 2010 , and in Jeonbuk in 2015 . The region with the lowest prevalence of PD was Chungbuk. .
General Comments On Methodology
This analysis identified many potentially important differences in the incidence of PD, which could possibly be attributed to environmental or genetic factors. However, as this meta-analysis contains studies with a range of methodological strategies, the differences between age- and gender-specific incidence may also be due to methodological differences or potential population confounders. Ideally, only studies using the same methods of case ascertainment would be combined in the meta-analysis. However, only 27 studies of PD incidence were found, with only 14 providing data that could be combined in the meta-analysis. There were only a few studies that used identical methodologies for case ascertainment. As all methods of case ascertainment have drawbacks, including attrition, misclassification, and nonresponse, the quality of individual studies may be equally as important as the method of case ascertainment in determining PD incidence. Therefore, we chose to combine studies using different methodologies and examine closely for heterogeneity using the I2 statistic calculated from the Cochrane Q chi-square test for heterogeneity. I2 values showed low to moderate heterogeneity in the female age groups from 40 to 70, with considerable heterogeneity in those 70-79 and 80+. Similarly, heterogeneity increased with age in males, though considerable heterogeneity was found in all age groups over 50.
Also Check: Does Parkinson’s Affect Vision
Trends In The Pd Incidence
Globally, the incident number of PD was 1,081.72 × 103 in 2019, which increased 159.73% since 1990. The overall age-standardized incidence rate was 13.43/100,000 in 2019, and it increased with an annual average of 0.61% from 1990 to 2019 . Compared to female patients, male patients had a larger incident number, and a higher increasing trend in ASIR . Among the age groups, the high incident numbers of PD were observed in the patients aged over 65 years, and the largest increasing percentage occurred in the age group of over 80 years .
Table 1. The changes in incidence and prevalence of Parkinson’s disease worldwide, and in sexes, SDI areas, and regions, 19902019.
Figure 1. Trends in the ASR of incidence, prevalence, and YLDs of Parkinson’s disease in global, SDI areas and geographic regions from 1990 to 2019. ASR, age-standardized rate SDI, sociodemographic index YLDs, years lived with disability.
Figure 2. The distribution of Parkinson’s disease incidence in age groups, SDI areas and geographic regions from 1990 to 2019. was the incident number in age groups was the ASIR in SDI areas was the incident number in geographical regions. ASIR, age-standardized incidence rate SDI, sociodemographic index.
Trends In Ylds Caused By Pd
In 2019, the number of YLDs caused by PD was 1210.09 × 103 globally, with an increase of 154.73% since 1990. The overall ASR of YLDs reported an increasing trend from 1990 to 2019, with the EAPC of 0.53 . Male patients had a higher burden, and undertook a larger increasing trend than female patients . Among the age groups, the highest YLD number was seen in the age group of over 80 years , and the percentage increased pronouncedly among the patients aged 45 years old .
Table 2. The changes in YLDs of Parkinson’s disease worldwide, and in sexes, SDI areas, and regions, 19902019.
The upward trend in the ASR of YLDs occurred in all SDI areas from 1990 to 2019, particularly the middle one . In terms of geographic regions, the largest number of YLDs was seen in East Asia , while the lowest one was in Oceania . The percentage of YLDs number increased from 27.97% in Eastern Europe to 256.90% in Central Latin America during 19902019. The ASR of YLDs ranged from 8.01/100,000 in Eastern SubSaharan Africa to 20.84/100,000 in East Asia. Increasing trends in the ASR of YLDs occurred in most regions, particularly East Asia . However, a minor decreasing trend was found in Oceania . The ASRs of YLDs were positively associated with SDI among the regions in 2019 .
Don’t Miss: How Do You Get Tested For Parkinson’s Disease
Single Genes Causing Parkinsonism
Genetic defects responsible for parkinsonism have been identified in some families . In many of these cases, the clinical features resemble typical PD. However, within affected families there are often clinical features that are unusual for PD. At present, mutations in at least five genes have been firmly associated with parkinsonism: synuclein parkin DJ1 PTENinduced putative kinase I and leucinerich repeat kinase 2 or dardarin . PINK1 homozygous mutations have been reported to be an important cause of disease among Italian sporadic patients with earlyonset parkinsonism, whereas the role of single heterozygous mutations is less clear . The LRRK2 G2019S mutation is the most common pathogenic mutation linked to parkinsonism, accounting for 12% of cases, including cases of not only younger but also older age at disease onset . Other candidate PD loci have been proposed, including putative diseasecausing mutations in the ubiquitin carboxyterminal hydrolase L1 and in a nuclear receptor of subfamily 4 . These candidates do not map to known PD linkage regions, but polymorphisms in both genes have been associated with PD in some casecontrol studies . The GSK3B polymorphism has been reported to alter transcription and splicing and interact with tau haplotypes to modify PD risk .
Motor Circuit In Parkinson Disease
The basal ganglia motor circuit modulates the cortical output necessary for normal movement .
Signals from the cerebral cortex are processed through the basal ganglia-thalamocortical motor circuit and return to the same area via a feedback pathway. Output from the motor circuit is directed through the internal segment of the globus pallidus and the substantia nigra pars reticulata . This inhibitory output is directed to the thalamocortical pathway and suppresses movement.
Two pathways exist within the basal ganglia circuit, the direct and indirect pathways, as follows:
-
In the direct pathway, outflow from the striatum directly inhibits the GPi and SNr striatal neurons containing D1 receptors constitute the direct pathway and project to the GPi/SNr
-
The indirect pathway contains inhibitory connections between the striatum and the external segment of the globus pallidus and between the GPe and the subthalamic nucleus striatal neurons with D2 receptors are part of the indirect pathway and project to the GPe
The STN exerts an excitatory influence on the GPi and SNr. The GPi/SNr sends inhibitory output to the ventral lateral nucleus of the thalamus. Dopamine is released from nigrostriatal neurons to activate the direct pathway and inhibit the indirect pathway. In Parkinson disease, decreased striatal dopamine causes increased inhibitory output from the GPi/SNr via both the direct and indirect pathways .
Don’t Miss: Can You Get Rid Of Parkinson Disease
Analysis Of The Influential Factors Of Eapc
The ASR in 1990 served as the disease reservoir at baseline, and the HDI reflected the level of human development, and the availability of health resources in settings, including regions and countries. The EAPCs of the incidence, prevalence, and YLDs had a negative association with the corresponding ASRs in 1990 . Meanwhile, only the EAPCs of incidence had a positive association with HDI in 2019 , which further explained that the trends of the ASIR increased pronouncedly in the high SDI regions and countries from 1990 to 2019.
Figure 7. The association s between EAPCs and ASRs in 1990 at the national level. EAPCs of incidence , prevalence , YLDs had negative associations with ASR in 1990, respectively. The association was calculated with Pearson correlation analysis. The size of circle is increased with the numbers in 1990. EAPC, estimated annual percentage change ASR, age-standardized rate YLDs, years lived with disability.
The Importance Of Establishing Parkinsons Prevalence Numbers
Parkinsons Prevalence estimates will help the Parkinsons Foundation attract the attention of federal and state government as well as the pharmaceutical industry to the growing need and urgency in addressing PD. This is an important first step to better understanding who develops PD and why.
The next phase of this study will be to determine the rate of PD diagnosis or incidence, how that has changed over time and what is the rate of mortality among those affected by PD. Determining the prevalence and incidence will allow the PD community to effectively advocate for additional money and resources necessary to support Parkinsons research.
Parkinsons Foundation Prevalence Project numbers highlight the growing importance of optimizing Parkinsons care and treatment for people with Parkinsons, which would help future caregivers and ease the strain on health and elder care systems.
Through this study, the Foundation works to better understand Parkinsons with the goal of solving this disease. Establishing these numbers and using them to educate the PD community and influence legislation will help the Foundation provide tailored support for under-resourced PD populations across the U.S.
The published study is available in the Parkinsons Foundation scientific journal, npj Parkinsons Disease.
Recommended Reading: How Do You Diagnose Parkinson’s
Prevalence Of Parkinsons State
Western and Southern states appear to have lower rates of Parkinsons disease, while Northeastern and many Midwestern states have higher rates . Mississippi and Montana have the lowest rates of Parkinsons, at 5.1 per 10,000. Vermont has the highest rate of Parkinsons at 9.9 per 10,000.
Exhibit 2: Prevalence of Parkinsons Disease, by geography
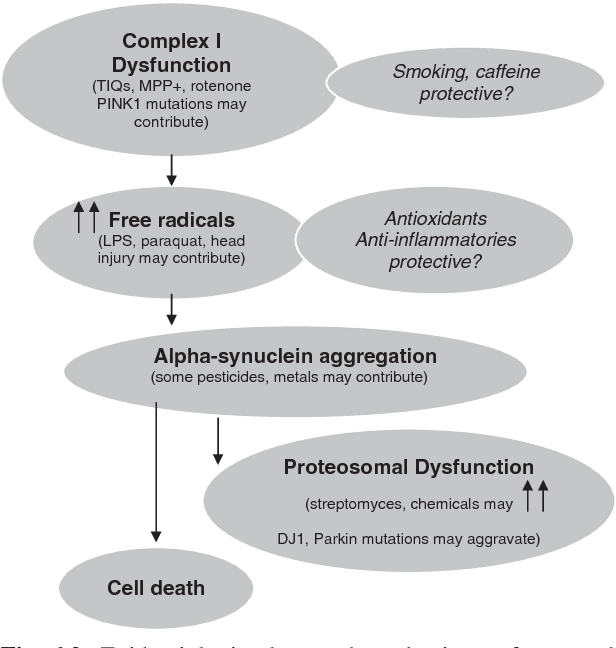
Proposed Environmental Risk Factors For Parkinson’s Disease
Risk factor investigation in PD is challenging, as the time of life most important to investigate is not known. It is likely that years, and possibly even decades, pass between the time of risk factor exposure and the clinical onset of parkinsonism. Casecontrol studies are an efficient way to study proposed disease risk factors, particularly in relatively uncommon disorders, such as PD. Potential limitations to this design include biased recall, the lack of validation of exposure and, in prevalent studies, survivor bias. Prospective cohort studies, assessing risk factors in advance of disease, avoid many of the biases of casecontrol studies, but risk factor investigation is limited to those selected for study and diagnostic accuracy may be less certain.
6.3.3.1. Rural living, farming, well water
Numerous studies worldwide have identified rural living, farming, gardening and drinking well water as risk factors for PD , but the results are somewhat inconsistent because of differences in the way the studies assessed the effects of rural living. Overall, risk of PD appears to be increased in rural dwellers especially in the USA. Metaanalysis results also support that risk factors include farm living and use of well water and pesticides. Although the specific associations are varied, the consistency of the general finding is remarkable.
6.3.3.2. Pesticides
6.3.3.3. Metals
6.3.3.4. Polychlorinated biphenyls
6.3.3.5. Occupation
Read Also: Things To Help Parkinson’s
Diet Obesity Physical Activity
6.3.4.1. Diet
Diet is a very difficult exposure to measure both because of its complexity and the fact that most individuals have qualitatively relatively similar diets . Despite these challenges, several dietary factors have been associated with PD.
Excess intake of dairy products has been associated with increased risk of PD in two large prospective cohorts . In a study of health professionals, whether the effect was due to calcium or milk could not be determined. Moreover, the risk was most marked in men, and not clearly observed in women. In the second study, PD incidence was more than twice as high in men drinking more than 16 ounces daily in midlife, compared to those who consumed no milk. This effect was independent of calcium. No women were included in this cohort. The reason for this association is unclear. One explanation is that milk may be a vehicle for potential neurotoxicants such as organochlorine pesticides or tetrahydroisoquinolines.
Other studies suggested different dietary risk factors for PD. PD risk was mildly raised in association with high dietary iron intake, but the risk markedly increased with high intake of both iron and manganese . Another study indicated increased risk with high vitamin C, carotenoids and sweet food, including fruit intake, but the number of cases studied was small . Among those with PD, homocysteinemia has been indicated as a potentially reversible risk factor for depression or cognitive decline .
6.3.4.2. Obesity
Trends In The Pd Prevalence
The global prevalent number of PD increased 155.50% from 1990, and reached 8,511.02 × 103 in 2019. The overall ASR of prevalence was 106.28/100,000 in 2019, and showed an upward trend from 1990 to 2019 . Compared with female patients, male patients had a higher prevalence, and showed a larger increasing trend . Among the age groups, the pronounced high prevalent numbers occurred in patients aged over 65 years , and the largest increasing percentage occurred in the age group of over 80 years .
All SDI areas presented increasing trends in the ASR of PD prevalence, and the most pronounced one was seen in the middle SDI area . At the regional level, the largest prevalent number in 2019 appeared in East Asia , while the lowest one occurred in Oceania . The increasing percentage of prevalence varied from 27.54% in Eastern Europe to 256.90% in Central Latin America. In 2019, the ASR of prevalence ranged from 55.94/100,000 in Eastern Sub-Saharan Africa to 145.44/100,000 in East Asia. Trends in the ASR of prevalence increased in most regions, particularly East Asia . Whereas, only Oceania had a minor downward trend . A positive association was observed between the ASRs and SDI in 2019 among regions .
Read Also: Parkinson’s Disease And Sleep Disorders
