Hallucinations And Delusions In Parkinsons Disease
It might be surprising to learn that 20 to 30 percent of people with Parkinsons disease will experience visual hallucinations. While typically not a symptom of PD itself, they can develop as a result to a change in PD medication or as a symptom of an unrelated infection or illness. It is important to know the signs of hallucinations and how to manage them.
Hallucinations and other more severe perceptual changes can be distressing to family often more so than to the person experiencing them. For the well-being of people with PD and caregivers, it is important to identify hallucinations as early as possible and take steps to reduce them.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about hallucinations and delusions in Parkinsons hosted by Christopher G. Goetz, MD, Professor of Neurological Sciences, Professor of Pharmacology at Rush University Medical Center, a Parkinsons Foundation Center of Excellence.
How To Care For Someone Who Experiences Hallucinations
If the person you care for experiences a hallucination, there are a few things youll want to do in the moment and others youll want to do when the moment passes.
The most important thing to remember is to never try and talk the person with Parkinsons out of their hallucination. They are actively experiencing it and by trying to talk them out of it, they may either feel like they arent being heard or that their experience is being diminished.
What matters in the moment is their safety and your reassurance that theyre going to be okay. You might calmly say, I understand that youre seeing X. Im not having that experience, and I just want you to know that everything is going to be okay, theres nothing dangerous happening here and youre safe.
Other strategies Dr. Joanne Hamilton, PhD, ABPP-CN of Advanced Neurobehavioral Health of Southern California, shared with us are to:
Here are a few actions you can take once the hallucination has passed:
Can Parkinsons Disease Make You Aggressive
Parkinsons disease Dementia or PD Dementia can make a patient very aggressive. Parkinsons Dementia Aggression germinating from Parkinsons disease Dementia can lead patients to behave erratically, experience sudden anger outbursts, feel constantly irritated, and always be in a state of restlessness. Outbursts are generally in the form of:
- Shouting
- Falling
Types Of Eye Movements
There are three kinds of eye movements that can change with PD:
- Saccadic rapid eye movements direct us to gaze at a specific object or to read lines of print.
- Pursuit eye movements allow us to follow an object as it moves.
- Vergence eye movements allow us to move our eyes in different directions2
Changes to these eye movements due to Parkinsons can also result in different kinds of visual difficulties. The inability to control eye movements can lead to involuntary blinking, double vision and other motor issues that can affect visual acuity.
Dry eyes can be treated with drops or ointments, warm wet compresses, but are not generally cured. The blink reflex can be impacted by PD. This manifests as either a slowing of the reflex, appearing as inappropriate staring, dry or burning eyes; and by reduced vision. Blepaharospasm and apraxia are two common eyelid motion issues. Blephararospasms are eyelid spasms that cannot be controlled, cause eyelids to squeeze, and can be relieved with Botox injections. Apraxia is a condition that makes it difficult to open eyes. There are specialized lid crutches and cosmetic tape that can be applied to hold the eyelids open.2
Selfcare For The Person With Parkinsons
- Join a Parkinsons support group if you dont already belong to one. Talk about your experiences, ask for help if you need it and share whats worked and not worked for you.
- Offer to have coffee with someone you know has been newly diagnosed and offer them support and encouragement.
- Make time to exercise and get out in nature every day.
- Communicate frequently with your doctors and discuss the possibility of tweaking your medications if your symptoms become worse.
- Rest when you need it.
- Plan a day trip or a vacation and get away from your normal surroundings.
- Take control where you can and keep authoring your own story.
- Practice or or Tai Chi to relax and calm your mind.
- Start a new project that youre excited to work on every day.
- Communicate with your care partners and let them know how they can best help you.
Who Is At Risk For Psychosis
Theres no predicting with certainty which patients with Parkinsons disease will go on to develop symptoms like hallucinations or delusions. A number of risk factors both internal and external- are associated with the condition.Some of these risk factors include: age, duration and severity of Parkinsons disease; and the taking of dopamine therapy.3-6
Do You Have Any Advice For The Family Friends And Carers Of People With Parkinsons Experiencing Hallucinations
Tell the patient that what they are experiencing is not real and do not pretend that you also experience the same thing. Be calm and friendly with the patient experiencing hallucinations can be quite stressful.
Need to know
Per Odin is a neurologist, professor and head of the neurology department at Lund University, Sweden. He also works at an outpatient clinic in Bremen, Germany. He has focused on Parkinsons disease, both clinically and in research, since 1987.
To find out more about Parkinsons disease and hallucinations, visit the EPDA website.
Read more:
Additional Drugs May Be Helpful
In addition to reducing your PD dosages, or removing certain meds from your treatment, there may also be additional drugs to try. If we reach a point where weve optimized medications and cant reduce any further because otherwise we would have more motor dysfunction, there are other medications we can add on to specifically address psychosis, explains Dr. Pan. There are three main options, she says, including Nuplazid , which the FDA approved for psychosis in PD in 2016, plus antipsychotics Clozaril and Seroquel . Your doctor can determine whats best for you.
Volunteer To Help Out
Everyday responsibilities like shopping, cooking, and cleaning become much more difficult when you have a movement disorder. Sometimes people with Parkinsons need help with these and other tasks, but they may be too proud or embarrassed to ask for it. Step in and offer to run errands, prepare meals, drive to medical appointments, pick up medications at the drug store, and help with any other day-to-day tasks they have difficulty with on their own.
Treating Psychosis That Can Accompany Parkinson’s Disease
Although treatment options are limited, physicians must learn to recognize and effectively treat Parkinson’s psychosis.
A new medication may soon be available to treat the hallucinations and delusions that often accompany Parkinson’s disease. “It shows promise in improving the hallucinations without worsening the motor functions,” says Jennifer G. Goldman, MD, an associate professor of neurology at Rush University Medical Center in Chicago.
She explained that, to date, good medications for treating Parkinson’s psychosis have been unavailable. “It would be very exciting to have another agent available to use,” she says.
Parkinson’s Psychosis People who have Parkinson’s disease may develop psychosis, possibly as a result of the medications used to treat the movement disorders but also possibly related to the disease itself. These misperceptions can range from illusions, such as a chair looking like a dog, to false beliefs, perhaps of an unfaithful spouse or an imaginary person living in the house, Goldman explains.
The hallucinations are primarily visualone of the many differences between psychosis symptoms in Parkinson’s and those in schizophrenia. With schizophrenia, people might have delusions of grandeur, believing they have unreal abilities, or they might hear voice commands. With Parkinson’s psychosis, Goldman explains, auditory hallucinations are infrequent and if they arise, generally are confined to background noise, such as children or music playing.
Parkinsons Disease And The Perfect Golf Swing: Reflections On My Dad
The earliest memories I have of my dad are of him practicing his golf swing in front of a mirror. It was a beautiful golf swing, perfected through hours upon hours of repetition. He loved the game. He was very physically fit, as a U.S. Marine. He would routinely do 100 push-ups and then run around the neighborhood in his black Marine Corps boots to assure he kept his callouses for reserve weekends. It was the late 1960s.
He must be a great player, I thought. It took me a few years to realize that my dad did not play golf.
My dad was the oldest son of Irish immigrants. At the age of 18, two weeks into his freshman year at Iona College, my dad received the news that he had a new sibling, a brother. This brother, his youngest, was born with Downs Syndrome. This news would impact my dads life in ways he couldnt have imagined.
Dad completed his graduate studies, began his career in public education and bought his first house. He changed the oil in his old Volkswagens and tuned up the lawnmower to save money. As he pushed the mower past the picture window at the front of our house, he would stop and practice his golf swing in the reflection, so he would be ready for the day when he had the time and resources to play.
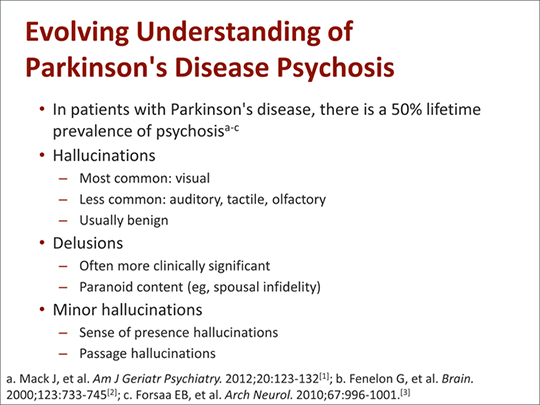
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
Lifestyle Changes Can Help
Beyond treatment with medications, other changes to your lifestyle may be helpful in managing psychosis symptoms in PD, says Dr. Pan. For example, increasing time spent with friends and engaging with others both help brain health in general, and may help reduce cognitive complications and psychosis in Parkinsons patients, says Dr. Pan. Also, a regular routine is important, such as keeping a regular sleep schedule, which can help with preventing psychosis and cognitive health, in general. Exercise is also protective in slowing the progression of Parkinsons, she adds.
What Causes Hallucinations In People With Parkinsons Disease
Hallucinations are very common in Parkinsons disease. More than half of patients experience them at some stage. They are normally thought to be an effect both of the condition itself and of Parkinsons medication. The risk of hallucinations increases with cognitive impairment, longer disease duration, age and other diseases.
Visual and auditory hallucinations may occur as a side effect of antiparkinsonian drugs which are used to treat the condition. They are often dose-dependent and in principle reversible.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Comparison Of Hallucinators And Non
The patients with isolated minor hallucinations were compared with the patients with no hallucinations . The only significant difference was a higher CES-D score in the group with minor hallucinations . When the presence of depression was determined using the cut-off values of the CES-D, depression was more frequent in the patients with minor hallucinations than in the patients without any hallucinations , but this difference did not reach significance.
The patients with formed visual hallucinations are compared with the non-hallucinators in Table 5. Patients with visual hallucinations differed in a number of respects: they were older, had a longer duration of disease, had a more severe motor state, had more depressive symptoms, and were more likely to have cognitive impairment, day-time somnolence and a history of ocular pathology. They were less likely to receive anticholinergics or selegiline and received a higher daily dose of levodopa, but the levodopa-equivalent dose did not differ significantly between the two groups. Visual hallucinations were recorded in 70% of the patients with dementia versus 10% of non-demented patients , and in 55% of the patients with severe cognitive disorders versus 8% of the patients with absent or moderate cognitive impairment .
The patients with hallucinations of any type were compared with the patients with no hallucinations. The results were identical to those of the preceding analysis, except for the degrees of significance .
Parkinsons Disease Psychosis: Hallucinations Delusions And Paranoia
As part of Parkinsons Disease and its treatment, hallucinations, illusions, delusions, suspiciousness and paranoid behaviors occur in over 50% of patients. In this 1-hour webinar Dr. Christopher Goetz suggests lifestyle changes, medication adjustments and a recently FDA approved drug to specifically treat psychosis in Parkinsons Disease.
I Had A Hallucination: What Next
Research has shown that for many people with PD who have them, hallucinations begin after a change in medication, more specifically, an increase in levodopa . Additional factors make a person more likely to experience hallucinations when medications are changed, such as other cognitive problems or memory issues, depression and sleep problems. Dementia|A term used to describe a group of brain disorders that cause a broad complex of symptoms such as disorientation, confusion, memory loss, impaired judgment and alterations in mood and personality.] also increases the risk of hallucinations and delusions when PD medications are changed. Dementia means cognitive changes whether in memory, judgment or attention that interfere with daily life.
One thing that does not affect the risk of hallucinations is your regular dose of levodopa. Rather, studies show that it is a change in dose an increase in a dose that has been stable that sets off hallucinations.
Tip: Experiencing a hallucination does not mean you are going crazy. Many people recognize that their hallucinations are not real. Do not react to these visions or sounds or engage them dismiss them. Bring up the topic with your doctor immediately.
What Should I Do When My Loved One Is Experiencing A Hallucination
Most importantly, dont try to convince your loved one that what theyre experiencing isnt real. Theyll feel like youre putting down an experience that seems authentic to them.
Once a person has lost insight, itll be very difficult to convince them that what theyre experiencing isnt happening. Trying to argue with them may agitate and even enrage the person. Making them anxious could cause their hallucinations to get worse.
Instead, talk to the person gently and reassuringly. You might say something like, I understand that you see a dog in the corner of the room. Everything is going to be OK. Youre safe. You might even say that the dog must have left already.
Remember that the person cant control what theyre experiencing. Try to be as sympathetic as you can when you talk to them.
One approach that can help is to turn on all the lights in the room. Hallucinations are more likely to happen in dimly lit areas, and this can be caused by disease-related changes that affect the eyes.
Then, have the person really focus on what theyre seeing. That may reset their brain and help them see whats actually in front of them.
If the person doesnt have insight, try a distraction. Move them to a different room. Turn on the TV or play a game they like.
Try to keep your loved one as calm as possible. If they become very agitated or violent, call their doctor or 911.
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.
Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD: quetiapine , clozapine and the newest agent, pimavanserin . They cause limited worsening of PD while treating hallucinations and delusions.
How Commonly Do Parkinsons Disease Patients Develop Psychosis
Psychosis in Parkinsons disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinsons disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinsons disease patients . In the early stage of Parkinsons disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing; that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinsons disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.
What Is A Hallucination
A hallucination is a perception of something that does not actually exist. This may be visualised, heard, felt, smelled or tasted. Hallucinations are sometimes confused with illusions, which are distortions of a reality rather than something that is purely imagined – as with hallucinations.
Visual hallucinations: In Parkinson’s, hallucinations are most commonly visual and may be in black and white, in colour, still or moving. Often the images involve small animals and children. They may disappear quickly or may last for some time.
Auditory hallucinations: auditory hallucinations are less common. These generally involve hearing voices or other familiar sounds. Auditory hallucinations can also be part of a depressive symptomatology.
Tactile hallucinations: hallucinations may be tactile, that is, you may feel a sensation, like something touching you.
Smell and taste hallucinations: less commonly you may feel that you can taste something you havent eaten, or you may smell something that is not present, such as food cooking or smoke.
Usually hallucinations are not threatening or distressing. If you hallucinate you may be unaware that your perceptions are not real, and sometimes imagined images or sensations can be comforting. But hallucinations can also be distressing and you may feel threatened or frightened and may need reassurance and comfort from those around you.
How Does Parkinson’s Cause Vision Issues
Parkinsons is characterized by a loss of dopamine producing cells in the substantia nigra portion of the brain. The reduction of dopamine can affect the visual cortex. So Parkinsons can impair mobility of the eyes just like the limbs. There are several kinds of visual disturbances that may be experienced by people with Parkinsons. Many who experience changes in vision or eye mechanics seek out a consultation from a neuro-opthalmologist, someone who specializes in visual problems associated with neurological disease.2
Parkinsons Disease And Psychosis: Hallucinations Delusions
Parkinson’s disease psychosis occurs in around 50% of PD patients. In Parkinson’s disease, hallucinations and confusion are relatively common, often occurring as side-effects of Parkinson’s medications. These symptoms can also be indicative of Parkinson’s disease psychosis, however, so it’s important to consult your doctor if you think you might be delusional or psychotic. In the meantime, here is everything you need to know about Parkinson’s disease psychosis, including symptoms and treatment.
Parkinsons Disease: Symptoms Of Psychosis
Common symptoms of psychosis in Parkinsons disease include:
Confusion and delusional thinking are common in PD psychosis, so you may not be able to identify psychotic symptoms in yourself. Usually, Parkinson’s disease psychosis is noticed by loved ones or care staff. However, if you think you’re displaying some of the signs, report them to your doctor immediately. Psychotic episodes can be incredibly frightening and upsetting, but there’s no need to suffer in silence.
Parkinson’s Disease Psychosis: The What When Why And How
Psychosis is a psychiatric term used in neurology to refer to a spectrum of abnormalities. Parkinsons disease psychosis is where people experience hallucinations or delusions. Hallucinations is seeing, hearing, or smelling things that dont exist. With tactile hallucinations, one can feel a presence that isnt there. Delusions are believing something that is not true, like that a spouse is being unfaithful or caregivers are stealing. In this one-hour talk, movement disorder specialist Christopher Goetz, MD, focuses on hallucinations and spends a little time on delusions.
Visual Hallucinations According To The Duration Of Parkinson’s Disease
The prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of Parkinson’s disease . We compared the characteristics of the patients with and without hallucinations among those with a short history of Parkinson’s disease and those with a long history . The results are shown in Table 7. Visual hallucinations had been present for a mean of 0.8 years in the patients with short-duration Parkinson’s disease and for 2.4 years in the patients with long-duration Parkinson’s disease . However, eight patients with long-duration Parkinson’s disease and one patient with short-duration Parkinson’s disease could not remember the year of onset of visual hallucinations. In both groups, patients with formed visual hallucinations were older and were more likely to be demented, according to DSM criteria, than non-hallucinators. The MMP score was lower in patients with visual hallucinations, although the difference reached significance only in patients with long-duration Parkinson’s disease. Patients with visual hallucinations had a more severely affected motor state than non-hallucinators in the long-duration group only.
