Prevalence And Risk Factors For Minor Hallucinations In Patients With Parkinsons Disease
Li Zhang
1Department of Geriatric Neurology, Affiliated Brain Hospital of Nanjing Medical University, Nanjing, China
2Department of Biological Sciences, University of Toronto Scarborough, Canada
3Institute of Neuropsychiatric Diseases, Brain Hospital Affiliated to Nanjing Medical University, Nanjing, China
Abstract
1. Introduction
Parkinsons disease is the second largest degenerative disease that has affected a large number of people worldwide . As one of the most detrimental nonmotor symptoms, PD associated psychosis affects up to 75% of patients throughout the disease course . This prevalence is underestimated because the psychotic symptoms are not fully considered as a spectrum that includes minor hallucinations , major hallucinations, and delusions.
Although MHs are now recognized to be closely associated with well-structured VHs , it has not been studied as thoroughly as well-structured VHs. MHs deserve widespread attention because it is the most frequent and earliest type of psychotic phenomenon in PD and occurs even before the onset of motor symptoms . MHs might also be an early predictor of a severe psychotic and cognitive state . Hence, this work was aimed at providing a comprehensive and in-depth understanding of MHs in the Chinese population.
2. Material and Methods
2.1. Patients and Study Design
2.2. Clinical Outcomes
2.3. Statistical Analysis
3. Results
3.1. Prevalence and Characteristics of MHs
| Presence hallucination |
| PD-total |
| PD-total |
| OR |
| 0.048 |
Consent
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Additional Drugs May Be Helpful
In addition to reducing your PD dosages, or removing certain meds from your treatment, there may also be additional drugs to try. If we reach a point where weve optimized medications and cant reduce any further because otherwise we would have more motor dysfunction, there are other medications we can add on to specifically address psychosis, explains Dr. Pan. There are three main options, she says, including Nuplazid , which the FDA approved for psychosis in PD in 2016, plus antipsychotics Clozaril and Seroquel . Your doctor can determine whats best for you.
Also Check: What Are The Early Signs Of Parkinson’s Disease
Showing Up As Your Best Self
Caring for someone with a progressive condition like Parkinsons disease can be challenging. Hallucinations only add to the stress of caregiving, especially if the person youre caring for doesnt have insight into what theyre experiencing.
The more you understand about your loved ones condition, the easier itll be to care for them. Talk to their doctor and read up on Parkinsons disease so youre better equipped to respond when hallucinations occur.
Dont forget to take care of yourself as well. Take regular breaks from caregiving to relax and do the things you enjoy. By tending to your own needs, youll have more energy to devote to your loved one.
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication youre taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldnt be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Don’t Miss: Premorbid Functioning
Common Causes Of Hallucinations
Hallucinations most often result from:
- Schizophrenia. More than 70% of people with this illness get visual hallucinations, and 60%-90% hear voices. But some may also smell and taste things that aren’t there.
- Parkinson’s disease. Up to half of people who have this condition sometimes see things that aren’t there.
- Alzheimer’s disease. and other forms of dementia, especially Lewy body dementia. They cause changes in the brain that can bring on hallucinations. It may be more likely to happen when your disease is advanced.
- Migraines. About a third of people with this kind of headache also have an “aura,” a type of visual hallucination. It can look like a multicolored crescent of light.
- Brain tumor. Depending on where it is, it can cause different types of hallucinations. If it’s in an area that has to do with vision, you may see things that aren’t real. You might also see spots or shapes of light. Tumors in some parts of the brain can cause hallucinations of smell and taste.
- Charles Bonnet syndrome. This condition causes people with vision problems like macular degeneration, glaucoma, or cataracts to see things. At first, you may not realize it’s a hallucination, but eventually, you figure out that what you’re seeing isn’t real.
- Epilepsy. The seizures that go along with this disorder can make you more likely to have hallucinations. The type you get depends on which part of your brain the seizure affects.
What Is Parkinsons Disease Psychosis
Parkinsons disease psychosis is a non-motor symptom of Parkinsons disease that causes patients to experience hallucinations and/or delusions.More than half of all patients with Parkinsons disease eventually develop symptoms over the course of their disease.1
Diagnosing and treating this condition can be complex. The condition relates to both neurology and psychiatry . For this reason, Parkinsons disease psychosis is considered a neuropsychiatric condition, since it deals with mental health symptoms caused by a disease of the nervous system .
Introducing an easier way to track your symptoms and manage your care.
Dont want to download the app? Use the non-mobile version here.
Read Also: Paroxysmal Kinesigenic Dyskinesia Prognosis
Visual Hallucinations According To The Duration Of Parkinson’s Disease
The prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of Parkinson’s disease . We compared the characteristics of the patients with and without hallucinations among those with a short history of Parkinson’s disease and those with a long history . The results are shown in Table 7. Visual hallucinations had been present for a mean of 0.8 years in the patients with short-duration Parkinson’s disease and for 2.4 years in the patients with long-duration Parkinson’s disease . However, eight patients with long-duration Parkinson’s disease and one patient with short-duration Parkinson’s disease could not remember the year of onset of visual hallucinations. In both groups, patients with formed visual hallucinations were older and were more likely to be demented, according to DSM criteria, than non-hallucinators. The MMP score was lower in patients with visual hallucinations, although the difference reached significance only in patients with long-duration Parkinson’s disease. Patients with visual hallucinations had a more severely affected motor state than non-hallucinators in the long-duration group only.
Who Is At Risk For Psychosis
Theres no predicting with certainty which patients with Parkinsons disease will go on to develop symptoms like hallucinations or delusions. A number of risk factors both internal and external- are associated with the condition.Some of these risk factors include: age, duration and severity of Parkinsons disease and the taking of dopamine therapy.3-6
Also Check: What Is Life Expectancy Of Parkinson’s Patients
What Should I Do When My Loved One Is Experiencing A Hallucination
Most importantly, dont try to convince your loved one that what theyre experiencing isnt real. Theyll feel like youre putting down an experience that seems authentic to them.
Once a person has lost insight, itll be very difficult to convince them that what theyre experiencing isnt happening. Trying to argue with them may agitate and even enrage the person. Making them anxious could cause their hallucinations to get worse.
Instead, talk to the person gently and reassuringly. You might say something like, I understand that you see a dog in the corner of the room. Everything is going to be OK. Youre safe. You might even say that the dog must have left already.
Remember that the person cant control what theyre experiencing. Try to be as sympathetic as you can when you talk to them.
One approach that can help is to turn on all the lights in the room. Hallucinations are more likely to happen in dimly lit areas, and this can be caused by disease-related changes that affect the eyes.
Then, have the person really focus on what theyre seeing. That may reset their brain and help them see whats actually in front of them.
If the person doesnt have insight, try a distraction. Move them to a different room. Turn on the TV or play a game they like.
Try to keep your loved one as calm as possible. If they become very agitated or violent, call their doctor or 911.
Selfcare For The Person With Parkinsons
- Join a Parkinsons support group if you dont already belong to one. Talk about your experiences, ask for help if you need it and share whats worked and not worked for you.
- Offer to have coffee with someone you know has been newly diagnosed and offer them support and encouragement.
- Make time to exercise and get out in nature every day.
- Communicate frequently with your doctors and discuss the possibility of tweaking your medications if your symptoms become worse.
- Rest when you need it.
- Plan a day trip or a vacation and get away from your normal surroundings.
- Take control where you can and keep authoring your own story.
- Practice meditation or yoga or Tai Chi to relax and calm your mind.
- Start a new project that youre excited to work on every day.
- Communicate with your care partners and let them know how they can best help you.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Treatments That Can Cause Psychosis
Dopamine therapies and anticholinergics are treatment types that can lead to hallucinations and delusions. If you or a family member are experiencing symptoms of Parkinsons psychosis, your doctor may recommend adjusting or discontinuing medications in these classes.
Dopamine Therapies
Hallucinations and delusions can be a side effect of dopamine therapies. Parkinsons disease develops when the brain cannot produce sufficient dopamine, a neurotransmitter that controls movement and emotions. Dopamine therapies, also referred to as dopaminergic drugs, work by increasing dopamine levels in the brain. Some dopamine therapies work by converting the brain chemical levodopa to dopamine, and others mimic dopamines effects in the brain .
Anticholinergics
Anticholinergics reduce the levels of acetylcholine a neurotransmitter that helps regulate motor functions. Hallucinations can be a side effect of these medications, especially for people over age 70.
How To Manage Hallucinations And Delusions
- Hallucinations and delusions are nonmotor symptoms of Parkinsons disease.
- There are a variety of ways to manage hallucinations and delusions, including medication.
- Discuss symptoms of psychosis with your or your loved ones doctor right away.
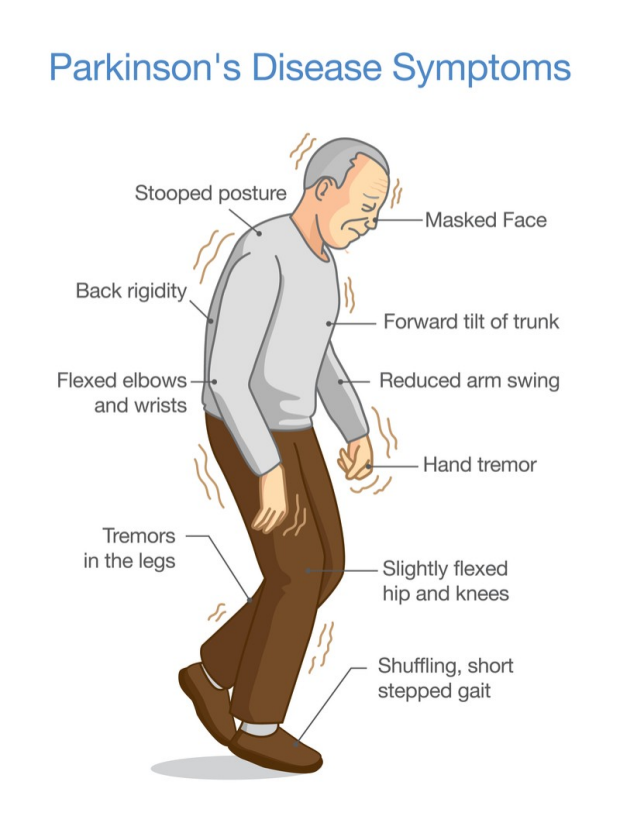
Hallucinations and delusions are symptoms of Parkinsons disease psychosis. Parkinsons psychosis impacts between 20 percent and 40 percent of individuals with Parkinsons disease. Managing hallucinations and delusions can be more challenging than managing motor symptoms of Parkinsons, like tremors, muscle stiffness, slowed movements, and loss of balance. A combination of interventions, including medication and changes around the home, are often necessary to manage hallucinations and delusions.
Don’t Miss: Parkin 2 Disease Symptoms
Memory Problems And Dementia
Research shows that hallucinations and delusions often happen when someone with Parkinsons also has problems with memory, thinking problems or dementia.
If you experience hallucinations at an early stage of Parkinsons, it could be a sign of another medical condition, such as dementia with Lewy bodies.
What Causes Hallucinations
Hallucinations can have several causes:
- Adverse effects of some medications that enter the brain are the main cause of hallucinations. These include antiparkinsonian drugs, pain killers, muscle relaxants, and sedatives.
- Neuron degeneration can spread to areas of the brain responsible for vision. The brain can then misinterpret the images transmitted to it or create perceptions without any external stimulus.
- Other medical conditions related or unrelated to Parkinsons disease. Infection, cognitive disorders, dementia, visual impairment can also cause hallucinations.
Most people living with Parkinsons disease do not experience hallucinations. Some episodes are often associated with:
- Dementia
Recommended Reading: What Are Early Warning Signs Of Parkinson’s Disease
What Can I Do
Not all forms of hallucinations need to be treated. Occasional spots or insects in your visual field do not need treatment if they do not disrupt your daily life. However, talk to your neurologist to review your medication.
Inform your loved ones about your hallucination tendency and your most frequent hallucination patterns. Reassure them that these hallucinations are harmless, that you remain perfectly sane and that these episodes are not linked to an accelerated progression of Parkinsons disease. Talk to them about how you feel during these episodes and what they can do to support you adequately.
Parkinsons Disease Psychosis: A Little
One of the lesser-known symptoms of Parkinsons Disease is Parkinsons psychosis. This webpage explains the prevalence, causes and symptoms, treatment options of PD psychosis. More useful to caregivers are sections on potential triggers of psychotic episodes and what caregivers can do about PD psychosis.
Read Also: What Essential Oils Are Good For Parkinson’s Disease
How Is Psychosis Managed
The urgency of treatment will depend on the type and characteristics of psychosis. Sometimes, when the hallucinations are mild and benign, and insight is retained, it is best that the Parkinson regimen be kept as is. However, when a patient is experiencing more threatening paranoid delusions, then more aggressive treatment is warranted .
The management of psychosis includes:
- Follow us on or on .
What The New Research Shows
Olaf Blanke is founding director of the Center for Neuroprosthetics at the Ecole Polytechnique Fédérale de Lausanne in Switzerland, and the senior author of the new study. He and his colleagues used a new robotic diagnostic tool that captures sensory and motor processing through brain imaging to determine the severity of the progression of the disease by safely provoking hallucinations in Parkinsons patients.
Patients tell me they feel like someone brushed against them.
In Parkinsons disease, hallucinations are among the most disturbing non-motor symptoms. The association between formed visual hallucinations and a more severe form of Parkinsons disease with cognitive decline and dementia is relatively well known. The most common and amongst one of the earliest hallucinations in Parkinsons disease, is the presence hallucination, the sensation of another person being present and nearby when no one is there. Patients tell me they feel like someone brushed against them, Blanke says.
Blanke and his colleagues studied the behavioral and neural mechanisms underlying symptomatic presence hallucinations in Parkinsons disease. The researchers induced the presence hallucination in the MRI scanner by means of robotically mediated sensorimotor stimulation to trigger the occurrence of symptomatic presence hallucination in these patients.
You May Like: Parkinson Patient Life Span
A Caregivers Guide To Parkinsons Disease Psychosis
While more than 50% of those taking carbidopa-levodopa may experience psychosis , medication management of these symptoms is a balancing act. First, families must bring psychotic behavior to the attention of your medical team. Medical causes of the behavior, like infection must be ruled out, followed by a review of medications and possible medication adjustments before a lifestyle changes and possible medications for treatment are added.
Hallucinations According To The Duration Of The Disease
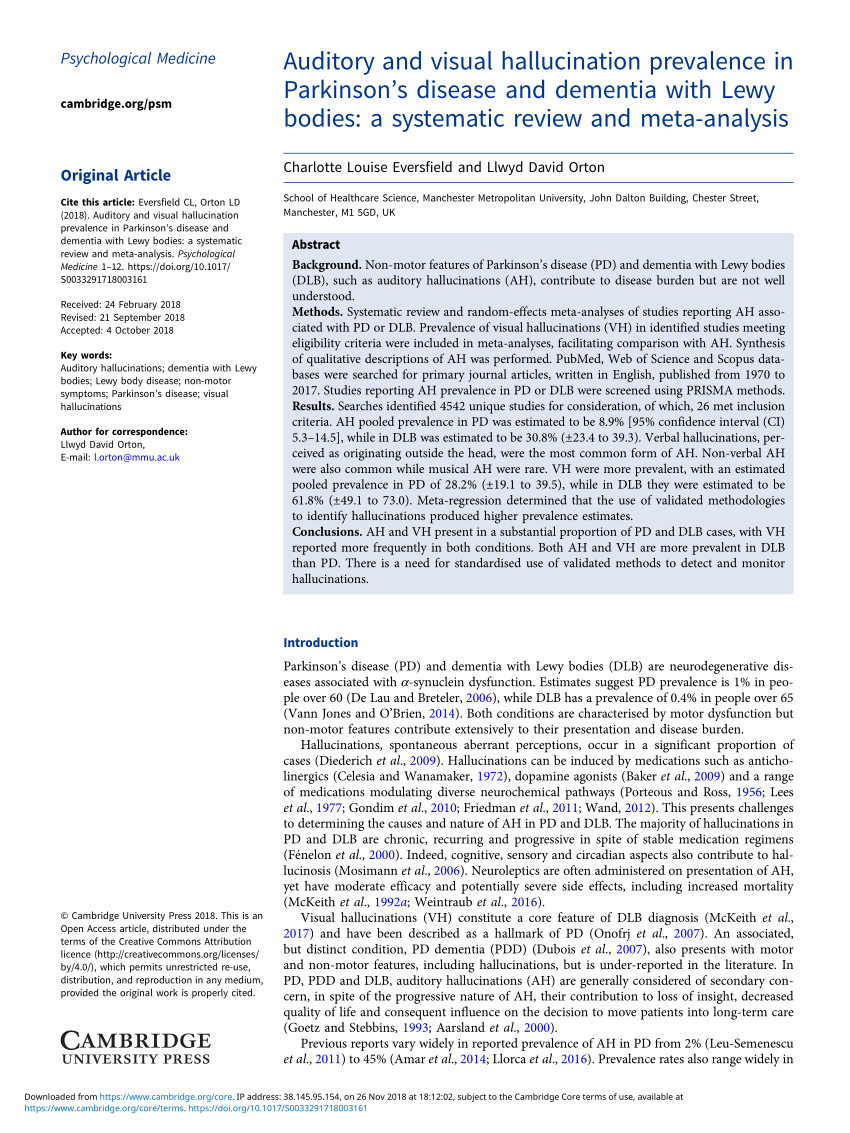
We found that the prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of the disease. Moreover, the duration of Parkinson’s disease was an independent predictor of visual hallucinations in the multivariate analysis. Other studies gave conflicting results on the relationship between hallucinations and disease duration. In a retrospective study of 100 patients, logistic regression analysis also showed an association between `psychosis’ and an increased duration of the disease . An association between the duration of the disease and the occurrence of hallucinations was also found by some investigators but not by others .
Table 1
Also Check: Life Expectancy After Parkinson’s Diagnosis
Or Parkinsons Itself May Lead To Psychosis
In other cases, the disease’s progression, rather than its treatments, is likely at the root of psychosis, says Ling Pan, M.D., clinical assistant professor of neurology and neurosurgery at NYU Langone Health in New York City. Psychosis can be symptom of Parkinsons itself, so patients, for example, who have not been on medications you track the natural course of their disease may develop psychosis as part of the disease pathology. However, it appears PD medications do increase the risk, she adds.
Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is the risk factors to look out for biological and environmental triggers that can bring them on and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
You May Like: Is Parkinson’s Disease Fatal