What Causes Psychosis In Parkinsons
Currently, there is not a clear understanding of the exact cause of Parkinsons disease psychosis, although certain brain chemicals and receptors are believed to play a role. In general, the condition is believed to be caused by either one of the following:
Side effect of dopamine therapy:
Although an exact causal relationship has not been established, some believe that this condition may be a side effect of dopaminergic therapy .2Dopaminergic therapy increases dopamine levels, helping improve motor symptoms in patients with Parkinsons disease. However, increasing dopamine levels can also cause chemical and physical changes in the brain that inadvertently lead to symptoms such as hallucinations or delusions.
Natural outcome of the disease:
This condition can be triggered by changes in the brain that occur regardless of taking dopamine enhancing medication. Some of these changes occur naturally as Parkinsons disease progresses.2
Palliative Care Management Of Non
Patients with PD can develop non-motor manifestations, categorized into autonomic dysfunction, cognitive impairment, neuropsychiatric disorders, and sleep disturbances. At the end-stage of PD, non-motor symptoms become more common and can become the most prominent medical problem, leading to increasing decline in quality of life both for patient as well as increasing caregiver burden . Non-motor symptoms occur in up to 50% of PD patients especially in association with the medication off state and may become worse by anti-PD medications . Almost one third of patients reports their non-motor symptoms to be at least as debilitating as their motor symptoms .
All patients with motor fluctuations face at least one non-motor problem during the off phase . In end-stage of PD, dementia, psychosis, and falls become more complex to manage than the motor complications; as a result, managing non-motor aspects is important to increase quality of life and decrease the burden of illness . Chaudhuri and co-workers, using a new 30-item non-motor symptom screening questionnaire , found noticeably high scores among PD patients for impaired taste/smell, impaired swallowing, weight loss, constipation, urinary urgency, forgetfulness, dribbling, sadness, hallucinations, anxiety, sexual dysfunction, falling, reduced concentration, daytime sleepiness, vivid dreams, and sweating .
How Does Someone Recover From A Drug
The best way to treat and recover drug-induced psychosis symptoms is to take the individual to a doctor or psychiatrist as soon as possible. There they will undergo an assessment to determine the best course of action to take.
It is difficult to determine the severity of the drug-induced psychosis symptoms when the person is still drunk or high. Since drugs and alcohol are mind-altering, to begin with, they already impact an individuals ability to see the world through a proper frame of mind.
If it is a strictly drug-induced psychosis, recovery will involve first sobering the individual up.
After the assessment, the doctor or psychiatrist will diagnose and treat the individual. Drug-induced psychosis recovery is different for each person, especially dependent upon the state of their mental health while sober.
It is difficult to provide a blanket outline for recovery from drug-induced psychosis because it is so unique to each individual. Many factors affect and influence the development of an episode of psychosis and how it plays out.
Again, the best idea when someone is experiencing symptoms of drug-induced psychosis is to take them to the emergency room or a local doctor or psychiatrist. No one should try to diagnose someone in psychosis by themselves.
If you are looking for help for a loved one, you can find additional resources here.
Don’t Miss: Is Parkinson’s Disease Fatal
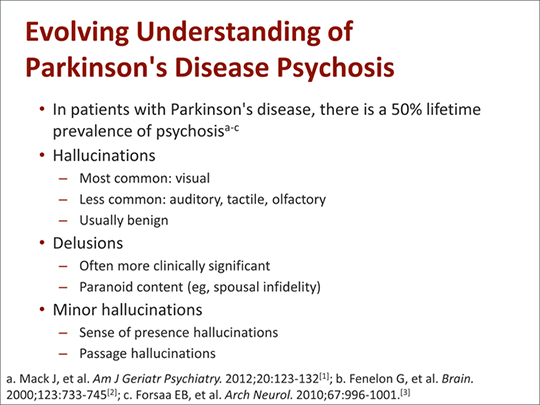
Potential Biomarkers Of Pd Psychosis
A biomarker is defined as a characteristic that can be objectively measured and that can indicate a normal biological process, a pathogenic process, or a pharmacologic response to a specific therapy . Biomarkers can range from clinical, neuroimaging, and biochemical to genetic or proteomic characteristics and their purpose can be to confirm a diagnosis, serve for epidemiological screening, predict an outcome, monitor disease progression, or assess and predict response to a treatment. In the thorough search for a therapy for PD in the past 30 years, next to the complexity of the disease itself, the lack of reliable tools available to monitor progression and to observe the effects of the interventions has been a major drawback. Screening for biomarkers in PD is therefore highly relevant, but no reliable ones are readily available . To this purpose, the PPMI is currently undergoing an observational, multicentre, international study designed to evaluate potential biomarkers of PD progression comprising 400 recently diagnosed PD patients and 200 healthy subjects among a total of 21 centres .
They Mistake Objects For People Or Animals
The most common symptoms of Parkinsons related psychosis are visual illusions and hallucinations, says Dr. Barrett. These can start out mild, with the person looking at an object but seeing something else. For example, they might mistake a lamp for a human or think the mailbox is a deer. These are early, minor hallucinations that may evolve to be more bothersome or pervasive, says Barrett.
You May Like: Is Parkinson’s Disease Fatal
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Examples Of Delusions In Pd
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Is Parkinson Disease
Parkinson;disease is a movement disorder. It can cause the muscles to tighten and become rigid This makes it hard to walk and do other daily activities. People with Parkinsons disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson;disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson disease. When it affects someone younger than age 50, it’s called early-onset Parkinson disease. You may be more likely to get early-onset Parkinson disease if someone in your family has it. The older you are, the greater your risk of developing Parkinson disease. It’s also much more common in men than in women.
Parkinson disease is a chronic and progressive disease.; It doesn’t go away and continues to get worse over time.
Neuropsychiatric Disorders In Parkinsons Disease: What Do We Know About The Role Of Dopaminergic And Non
- 1Inserm U1171 Degenerative and Vascular Cognitive Disorders, Lille University Medical Center, Lille, France
- 2CNRS, Institut des Sciences Cognitives Marc Jeannerod, UMR 5229, Lyon University, Bron, France
Besides the hallmark motor symptoms , patients with Parkinsons disease have non-motor symptoms, namely neuropsychiatric disorders. They are frequent and may influence the other symptoms of the disease. They have also a negative impact on the quality of life of patients and their caregivers. In this article, we will describe the clinical manifestations of the main PD-related behavioral disorders . We will also provide an overview of the clinical and preclinical literature regarding the underlying mechanisms with a focus on the role of the dopaminergic and non-dopaminergic systems.
Read Also: Parkinson’s Stage 5 Life Expectancy
Diagnosis Of Dip And The Role Of Dat Imaging
The clinical diagnostic criteria for DIP are defined as 1) the presence of parkinsonism, 2) no history of parkinsonism before the use of the offending drug, and 3) onset of parkinsonian symptoms during use of the offending drug. Since asymmetrical rest tremors are common in many DIP patients and symptoms persist or progress after cessation of the offending drug, patients clinically diagnosed with DIP may include individuals in the preclinical stage of PD whose symptoms were unmasked by the drug.,,,
DATs are presynaptic proteins in the membrane on terminals of dopaminergic neurons. They take up dopamine from the synaptic cleft projections that extend from the substantia nigra to the striatum. These transporters control dopaminergic transmission by spatial and temporal buffering, rendering the molecule an imaging target in diseases affecting the dopaminergic nigrostriatal pathway. Single-photon-emission computed tomography and positron-emission tomography scans are available using several DAT ligands., SPECT radioligands include 123I-N-3-fluoropropyl-2-carbomethoxy-3-nortropane , 123I-ioflupane, DaTSCAN, and 123I-2-carbomethoxy-3-tropane . PET scans may be superior to SPECT for imaging DATs, in that the lower energy of positrons provides higher resolution, resulting in better image quality with widespread clinical applications. However, most DAT imaging studies, including those in patients with DIP, have utilized SPECT.,-
Psychosis In Mental Illness
There are a number of mental illnesses that can include psychotic episodes as a symptom. Schizophrenia is often the first illness that comes to mind when people think of psychosis, however, not every type of schizophrenia includes psychotic symptoms. Paranoid schizophrenia is characterized by both hallucinations and delusions, though how disruptive this depends on how severe the condition is. People with bipolar disorder can also experience psychosis. This typically occurs during severe manic periods. Psychosis can also appear in people with major depressive disorder, which can result in a diagnosis of psychotic depression. Unfortunately, this disorder has a high mortality rate due to the intense suffering combined with psychotic episodes. Other disorders that have psychosis as a symptom include delusional disorder and schizoaffective disorder. Plus, it can present in degenerative brain diseases like Parkinsons disease, Huntingtons disease, and dementia.
Brain tumors, cysts, or untreated HIV or syphilis can also cause psychosis. When an individual has a mental illness that already has the potential to include psychosis, drug abuse can more easily lead to this symptom. It can be tricky to determine whether the drug abuse triggered the psychosis or whether the early effects of psychosis led to drug abuse. At the same time, certain substances can interact with antipsychotic medications, causing them to become less effective or ineffective, triggering a psychotic episode.
You May Like: Parkinson’s Disease Life Expectancy
How Caregivers Can Cope With Parkinsons Related Psychosis
As a caregiver, you might struggle to cope when your loved one insists that their hallucination or delusion is real. That said, you dont have to fight every battle. When reasonable, it might be better to not always contradict your loved one when the hallucinations or delusions are fairly fixed, because that can just become a point of contention and argument that increases the stress for both the patient and caregiver, says Barrett.
For example, if your loved one is falsely accusing you of cheating or stealing from them, you might want to correct them. But if they mistake a lamp for an animal or see a monkey in the backyard and they arent bothered by it, resist the urge to correct them just for the sake of correctness. If they want to know, Is that real or not? then of course you can clarify, says Barrett. But if theyre not bothered or upset by their hallucinations, its OK sometimes to just let it be.
However, if the psychosis is bothersome and interfering with your loved ones care, help them talk with their doctor about treatments that could help.
And above all else, remember to take care of yourself. Research published in 2015 in Parkinsonism & Related Disorders shows that psychosis is particularly burdensome for caregivers of people with Parkinsons disease. If thats the case, dont hesitate to lean on others, such as your family members or hired help, for support.
How Substance Abuse Can Lead To Mental Illness
A study published in the American Journal of Psychiatry sheds light on this issue. It reports that about one-third of patients with drug-induced psychosis went on to develop mental illness.
It is known that an underlying mental health disorder can be a risk factor for developing a substance use disorder. This study concludes that a high number of addicts acquired a psychotic disorder as a result of the substance abuse.
This happens most with people who use cannabis and then have a psychotic event. After the event about 50% of them ended up with sustained mental illness, states The British Journal of Psychiatry. This study revealed that young male cannabis users were at highest risk for this outcome.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Parkinsonism Due To Other Neurological Disorders
The following neurological disorders are known to cause parkinsonian symptoms:
Vascular parkinsonism;Also known as arteriosclerotic parkinsonism, this condition is caused by multiple small strokes.
The onset of symptoms can be sudden or gradual, and often includes mobility problems in your legs. Symptoms may level off for a period of time.
Vascular parkinsonism has the slowest rate of progression of all atypical parkinsonisms. It doesn’t usually cause tremors, either.
Post-traumatic parkinsonism;Also known as post-traumatic encephalopathy or “punch-drunk syndrome,” this condition may be caused by a severe head injury or by frequent head trauma, such as from boxing or football.
Post-traumatic parkinsonism can lead to a type of dementia called chronic traumatic encephalopathy . In March 2016, the National Football League admitted that there might be a link between CTE and head trauma.
Essential tremor;This is a tremor that tends to run in families and become worse over time. It’s usually seen most severely in the hands, especially when the hands are moving.
Normal pressure hydrocephalus ;This condition is caused by an abnormal increase in fluid in the cavities of the brain.
NPH can sometimes be treated by draining the extra fluid into your abdomen using a shunt.
Environmentally Caused Parkinsonism
The following disorders are caused by outside factors like drugs and infection:
The following substances can cause drug-induced parkinsonism:
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Pathophysiology Of Pd Psychosis
The pathophysiological processes underlying PD psychosis can be subdivided into intrinsic and extrinsic . While intrinsic PD psychosis is thought to be caused by alterations in dopamine, serotonin, and acetylcholine systems involving subcortical projections as well as synaptic and neuronal changes in limbic and cortical structures , extrinsic PD mainly involves dopaminergic or anticholinergic therapies, especially dopamine agonists .
To better understand the neurotransmitter dysfunctions underlying the development of hallucinations, the effect of hallucinogenic agents with known mechanisms of actions is of advantage. Classically, hallucinogenic agents were subdivided into those affecting the cholinergic system and those involving the aminergic system, herein dopaminergic and serotoninergic agents being included . The described clinical characteristics and associated hallucinations caused by these two distinct systems also differ: while the effects caused by anticholinergic agents are associated with peripheral autonomic features, confusion, disorientation, and visual hallucinations, mostly poorly formed and of a threatening nature, the symptoms caused by aminergic agents are characterised by a heightened awareness of objects, forms, and colours with a clear sensorium, sometimes involving the presence of hypnagogic phenomena of a dream-like quality .
They Hear Noises Or Voices That Arent There
People with Parkinsons related psychosis commonly report hearing footsteps, a shutting door, or creaking in the house that others dont hear, says Barrett. These auditory hallucinations are less common than visual hallucinations, but sometimes they occur in tandem, especially in those with more severe psychosis.
Recommended Reading: Is Parkinson’s An Autoimmune Disease
Electroconvulsive Therapy And Deep Brain Stimulation
Electroconvulsive therapy has shown beneficial effects in the treatment of neuropsychiatric symptoms in PD in some studies in the literature. The most recently published study on the effect of ECT in 29 drug-refractory PD patients with psychiatric symptoms, 12 of them having psychosis and depression and one having isolated psychosis, showed an improvement in measures of motor as well as nonmotor function assessed by means of different scales as seen in .
How Is Parkinson Disease Diagnosed
Parkinson disease can be hard to diagnose. No single test can identify it. Parkinson can be easily mistaken for another health condition. A healthcare provider will usually take a medical history, including a family history to find out if anyone else in your family has Parkinson’s disease. He or she will also do a neurological exam. Sometimes, an MRI or CT scan, or some other imaging scan of the brain can identify other problems or rule out other diseases.
Don’t Miss: Is Parkinson’s Hereditary
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person

