Stiff Shoulder Syndrome And Parkinsons Disease
Are your shoulders stiff? You may be suffering from stiff shoulder syndrome. Could it be from Parkinsons disease?
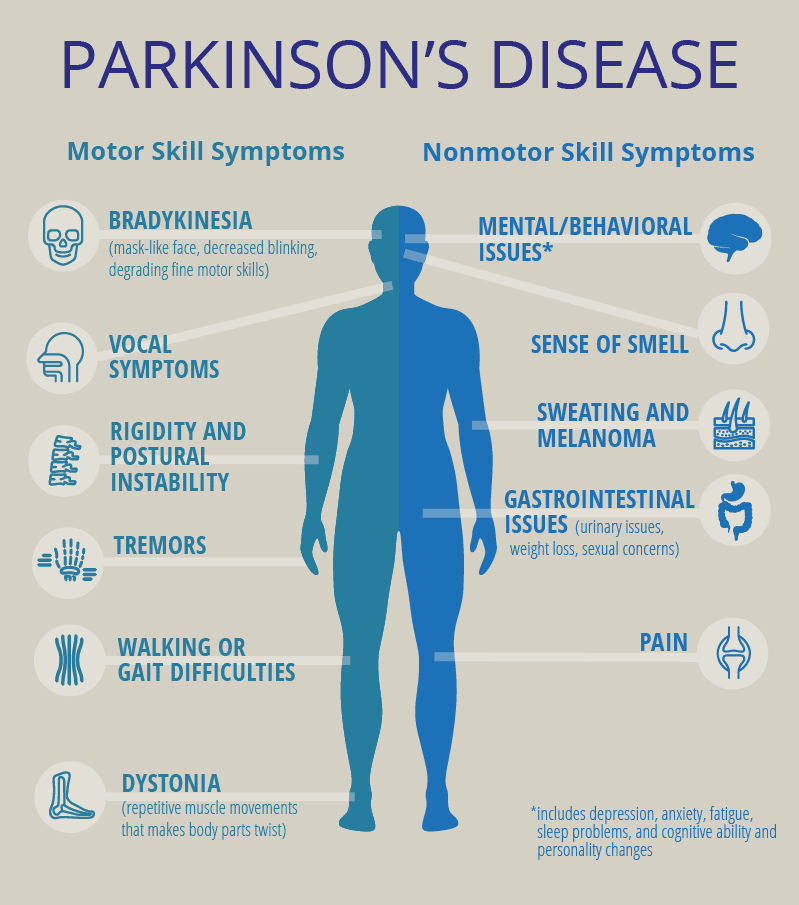
Shoulder stiffness is, in fact, one of the conditions associated with Parkinsons disease, a neurodegenerative disorder caused by a lack of dopamine in the brain. Dopamine is a chemical that helps you to have smooth, coordinated muscle movements.
The bones, ligaments, and tendons that make up your shoulder joint are encased in connective tissues. Frozen shoulder occurs when these tissues thicken and tighten around the shoulder joint, making it harder to move.
Adhesive capsulitis can develop before a diagnosis of Parkinsons disease. The peak incidence occurs around two years prior to the diagnosis of the disease.
Can Parkinsons Affect Your Bowels
If you have Parkinsons, you may be more likely to have problems with your bladder or bowels than people of a similar age without the condition. Some of these problems are common in men and women of all ages, whether they have Parkinsons or not. Bowel problems are very common in the general public.
Active Research Into Several Aspects Of Parkinsons Pain
Researchers are working to better understand the mechanisms behind pain in Parkinsons so that it can be more effectively addressed. They are looking for objective measurements, such as brain imaging, to diagnose and monitor pain, and to evaluate response to treatment. And, theyre investigating several drugs and deep brain stimulation for their potential benefits in treating Parkinsons disease pain.
You May Like: Doctors That Specialize In Parkinsons Disease
Read Also: Parkinson’s Disease And Eye Problems
Complementary And Alternative Medicine
In addition to pharmacologic and interventional treatments, several complementary and alternative therapies have also been investigated for alleviating PD pain. The designation of alternative medicine is a bit of a misnomer as these treatments are typically used alongside traditional pharmacologic and surgical interventions. A number of studies have examined the benefits of complementary therapies, but there is a lack of large-scale, high-level research and results are mixed regarding their effectiveness. Fortunately, most complementary therapies are safe and well-tolerated, and current literature, though limited, does suggest a role for including these therapies as a component of a multimodal approach to pain treatment.
Finally, there has been some research into the use of cannabis for pain treatment in the setting of PD. In two small, open-label, observational trials in PD patients, cannabis was found to improve pain scores as well as significantly decrease heat and cold pain tolerance . The authors postulated that cannabis acts on PD pain via modulation of the peripheral and central pathways . While no adverse effects were found in these trials, unlike with other complimentary therapies, cannabis use carries the risk of unpleasant side effects. Patients must be aware of the potential for paranoia, delusions, breathing problems, increased heart rate, and nausea. These side effects are typically dose related with incidence increasing with higher doses.
A Bottle Neck To Neurological Health
I have noticed that a lot of people with Parkinsons Disease, and other neurological disorders too, such as Alzheimers, suffer with severe neck pain and/or stiff, rigid necks. In terms of neurological problems, our necks can be a pinch point – a constricted passageway or tunnel, through which all the superhighways between our brain and the rest of our nervous system and organs, and from there, out into the far reaches of our fingers and toes, must pass. All of our utilities, the two-way electrical wirings, the broadband and telegraph wires of the nervous system, the water and air supplies, the chemical pipelines providing nutrients and the sewer pipes taking away the excreta of the brain, must pass through this narrow gap. This is no ordinary tunnel: to keep these utility supplies open and running, it was designed to keep on moving itself and in truly extraordinary ways of flexible motions.
Even slight damage or stiffening up of the neck can cause constrictions or interruptions of these important electrical and chemical flows. For oxygen and nutrients that enter through the mouth or nose, it is double jeopardy, as they have to pass through the bottle-neck twice, down into the lungs or to the gut, and back up again to get the brain. The neck is therefore a primary attention site for progressive symptom reduction strategies. In this article, we look at aspects of the neck and consider what we can do to improve our lot.
Also Check: What’s The Cause Of Parkinson’s Disease
Colm Was Diagnosed With Parkinson’s Around 3 Years Ago And Experiences 4 Different Types Of Pain Related To The Condition
The 4 different types of pain I experience all affect my muscles and joints. This includes sudden-onset joint pain typically a frozen shoulder, or pain when I bend an elbow or knee. It usually lasts between 6-8 weeks and will usually go away for a week or 2, only to reappear in another joint. It greatly restricts my movement and its constant nature can be frustrating.
I also have issues with leg cramps and dystonia, which I frequently experience when waking in the morning, or when moving between different ground surfaces. The cramps are very severe with sudden onset, but slowly wear off after some minutes.
My Parkinson’s has worsened certain pre-existing conditions, including back problems, which were caused by a childhood injury. This has caused me painful episodes throughout my life, but my Parkinson’s seems to have exacerbated this to the point where I’m totally incapacitated with pain and stiffness.
As a carer, I have no option but to try and carry on with my normal duties…I find it helps to wake about 2 hours earlier than normal to take my medication.
I keep an armchair and some dressing aids in my bedroom, as a bout of very severe back pain makes getting in and out of bed or dressing myself difficult.
I also experience muscle stiffness and inflexibility, which cause me pain due to over-exertion. This happens if I don’t take regular breaks throughout the day. As a carer myself for 3 disabled family members, this can prove very difficult.
Want More Practical Articles Like This
Much more can be found in our Every Victory Counts® manual. Its packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Request your copy of the Every Victory Counts manual by clicking the button below.
Thank you to our 2020 Peak Partners, Amneal and Kyowa Kirin, with special support from Adamas, for helping us make printing, distributing, and shipping the Every Victory Counts manual for free possible.
Recommended Reading: Zhichan Capsule
You May Like: Parkinson’s Disease And Spinal Stenosis
Ocean Trial Testing If Ongentys Can Ease Pain Of Motor Fluctuations
According to an article published in 2018 in Frontiers in Neurology, both low back pain and Parkinsons are associated with impaired proprioceptive function, sensory orientation during standing balance, anticipatory postural adjustments, automatic postural responses, and striatal-cortical function.
All of those are present as I wobble and weave through my off periods. Neck and back pain are more intense on the right side, but its subtle and hard to distinguish when the spasms are happening.
The authors of the Frontiers in Neurology article go on to suggest that it may not be so implausible to consider as an axial parkinsonism, rendering it the most prevalent parkinsonism in the world.Axial parkinsonism symptoms include gait freezing, postural instability, and trunk posture alterations and can have a significant impact on patients quality of life. Moreover, these symptoms are poorly responsive to dopaminergic drugs and surgical therapies.
In a 2008 article published in The Journal of the Canadian Chiropractic Association, a chiropractic doctor noted how early Parkinsons without tremor imitated mechanical back pain. During a follow-up visit with the patient after the official Parkinsons diagnosis, the provider noted that something started to change about a year earlier.
The articles author wrote:
Dont Miss: What Medication Is Given For Parkinsons
Carotid Body Activation And Parkinsons Disease
Drawing all of the above together, it is first interesting to note that the motor functions which the medulla controls are the very things that are most obviously offline or downregulated in people with PD, namely the voluntary movement of the face, head and neck, and of the limbs.
Next, consider that activations of the carotid bodies, due to a lack of oxygen to the brain, have very significant influence on the medulla, and that the primary response of the carotid body is to put the body into an oxygen preserving shutdown or frozen state, in which one loses access to voluntary muscle movements through the action on the medulla.
Thirdly, note that it seems sufficient dopamine is required for turning the carotid body activation off again.
Then a simple and elegant, self-consistent explanation emerges, that, in people with idiopathic PD, our carotid bodies have become stuck on in the activated state, initially triggered by a lack of oxygen to the brain, but then not having enough dopamine supplies to be able downregulate or switch the activation off again, effectively trapping us in a permanent shutdown state of Freeze or Tonic Immobility.
Unresolved issues with oxygen supply to the brain could potentially be causing the carotid body to be continually firing off danger signals, resulting in Dorsal Vagus activated types of shutdown. If we then dont create enough dopamine supplies to overcome this, then we cant turn this response off.
Don’t Miss: Can You Reverse Parkinson Disease
Annual Report Parkinson’s Disease Center And Movement Disorders Clinic
I hope this letter finds you well. On behalf of the Parkinsons Disease Center and Movement Disorders Clinic, I am pleased to share highlights of activities and achievements from the past year.
Our success is made possible thanks to the generosity of supporters like you. I hope youll be inspired to continue your support of our world renown movement disorders fellowship program. Many of the alumni of our training program have become leaders in the field of Parkinsons disease and other movement disorders. For example, Francisco Cardoso, M.D., Ph.D., an alumnus of our program, is the current president of the International Parkinson and Movement Disorder Society, an umbrella organization for all movement disorders.
I am happy to report that, based on our accomplishments, our designation as the Parkinsons Foundation Center of Excellence has been extended for another five years. We have been also honored by extension of our Tourette Association of America Center of Excellence.
In addition to over 60 clinical trials and investigator-initiated studies, we have expanded our diagnostic program by providing skin biopsies to search for evidence of Parkinsons disease and related disorders in very early stages of the disease. We continue to provide the state-of-the art deep brain stimulation and other neuromodulation approaches to our patients and are now offering focused ultrasound as a new treatment for Parkinsons disease and essential tremor.
Dr. Joseph Jankovic
Psychiatric And Neurobehavioral Disorders
These disorders are related to the connection between the brain and behavior. Neurobehavioral disorders are impairments associated with brain diseases like multiple sclerosis, stroke, and dementia or brain injury. Psychiatric disorders are associated with abnormal functions of the part of the brain responsible for social cognition. Historically, the study and treatment of these disorders were separate, but today doctors embrace a connection between the two in order to better treat and diagnose a wide range of conditions affecting the brain.
Also Check: How To Care For A Person With Parkinson’s Disease
Dropped Head Syndrome Results In Neck Pain Trouble Eating & Interferes With Vision
Dropped head syndrome causes a recognizable deformity with varying degrees of chin on chest posture. There is usually weakness of the neck muscles that results in the head dropping forward, sometimes called ptosis of the head. The fixed flexion or forward bending of the neck is often painful, interferes with feeding and horizontal eye gaze. The head is typically able to be passively ranged or moved up by hand.
It is most often associated with problems of the nerves and/or muscles, however in some cases there is no obvious cause even after extensive evaluation, or muscle biopsy may indicate a cause that is isolated to the neck extensor muscles and non-inflammatory. These cases are called isolated neck extensor myopathy or may be described as idiopathic head ptosis, where neck muscle weakness is the only symptom.
There are many potential and varied causes: central or peripheral nerve disorders like myasthenia gravis or Parkinsons disease, autoimmune problems of muscle and connective tissue such as polymyositis and systemic sclerosis they may be systemic and progressive with a poor prognosis like amyotrophic lateral sclerosis .
The most common cause of dropped head syndrome is isolated neck extensor myopathy and may have a benign clinical course.
Read Also: How Are You Tested For Parkinsonâs Disease
What Is Special About Parkinsons Syndrome Sufferers
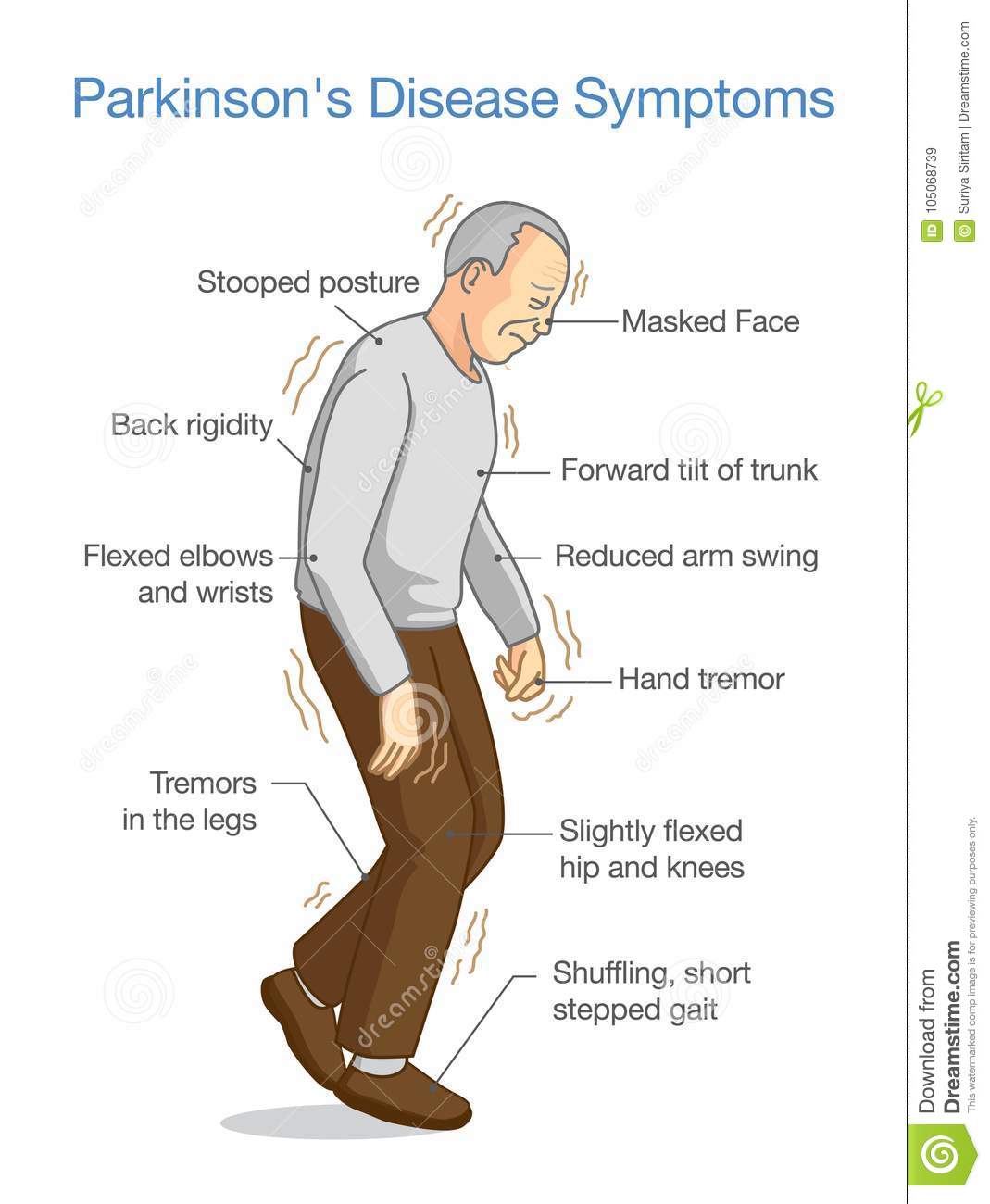
Parkinsons Syndrome is a condition where the important nuclei below the brain become dysfunctional resulting in impaired communication and transmission of nerve impulses to and from nerve fibres throughout the body. Consequently some cognitive processes, eyesight focus, muscle control or strength may deteriorate. This often presents in a haphazard fashion with increasing stiffness of the joints and muscles and intention tremor most noticeable in the hands. Fine movements and writing ability deteriorate, The gait deteriorates as seem as a shuffling pattern with small steps with a quickening of gait as power is mustered and spasm is overcome, Whilst there is a downhill trend the process of deterioration may arrest for periods.
Seldom does this process directly generate nerve pain such as sciatica. Back or Neck pain and pain referred in to the arm or leg may arise in Parkinsons Syndrome Sufferers as part of the Degenerative Disc Disease seen in the rest of the population and with the same pathologies disc protrusions, nerve entrapment / scarring / tethering, Lateral Recess Stenosis, Axial Stenosis, Spondylolytic Spondylolisthesis, vertebral slippage, Instability, Failed Back Surgery or failed chronic pain management.
Also Check: Are Parkinson’s Symptoms Worse At Night
The Medulla Part Of The Brain
The medulla is a long cone-shaped structure which makes up the part of the brainstem at the top of the spinal cord. It is responsible for autonomic functions ranging from vomiting to sneezing, heart beat, breathing, vomiting, and blood pressure, as well as sleep. It connects the higher levels of the brain to the spinal cord, and is responsible for several functions of the autonomous nervous system which include the control of breathing via signals from the carotid bodies and other chemical sensors in the body.
It is also primarily involved in carrying out the somatic motor function of the muscles of the face, head and neck, as well as for voluntary motor control of the body and limbs. Connections to the somatosensory cortex suggest that the medulla is also responsible for modulating sensory information from the body.
How Does Parkinsons Affect Your Neck
The neck can tilt, turn, bend forward, bend backwards, or assume a position that is a combination of these movements. This can be associated with PD, but may also accompany other forms of parkinsonism. The most common scenario in PD and parkinsonian disorders, is a neck that is mostly bent forward or flexed.
Read Also: Is Parkinson’s Disease A Motor Neuron Disease
Pain In Parkinsons Disease: A Spotlight On Women
This 2-page interview with neurologist, Dr. Jori E. Fleisher, discusses pain in Parkinsons disease with some interesting statistics about women and pain. Dr. Fleisher outlines the 4 primary types of pain in PD, how depression interferes with pain management, the role of exercise and medications in pain management as well as alternative therapies.
James* Was Diagnosed With Parkinson’s In 2011 His Pain Has Worsened As His Condition Has Progressed
When I was diagnosed with Parkinson’s, I initially felt little to no pain. It’s only now, in the advanced stages of the condition, that I’ve started feeling pain, coupled with the normal ageing process.
One of the worst pains I experience is dystonia and dyskinesia of the upper body, especially in my neck and head. It usually starts with a pulsing headache, followed by jerking of the muscles in my face, neck, upper torso and hands. It’s particularly severe in my arthritic finger and my neck. It can be severe to mild, often very distressing, and can last up to 2 hours.
I also have mild to moderate, uncontrollable movements or swaying associated with dyskinesia. It’s more prominent when I’m sitting down at a table or working on my laptop. Strangely, I feel this pain at its worst when I’m on the phone, or trying to explain something, or if I’m feeling over-excited or anxious which is when I become severely dyskinetic. There’s now a dull, continuous pain in my neck, caused through the movement, which gets sharper during bouts of the symptom.
I also experience pain when standing, mostly during a ‘wearing off’ period. My knees pull towards each other and the pain is so severe that I can’t walk. Luckily it only lasts a minute or 2, but the pain can be distressing.
To ease the pain, I take paracetamol as and when, occasionally co-codamol, and very occasionally an anti-inflammatory, for the arthritis. I previously tried cannabis oil but it was of no benefit to me.
Read Also: Does Parkinson’s Cause Constipation
When Sciatica Symptoms Become Severe
If your sciatic nerve becomes seriously compressed, the resulting symptoms can go from uncomfortable to quite painful and even embarrassing. You may become weak and numb on one side. Sometimes, even getting your leg or foot to move becomes impossible. If the pain hits you suddenly, and with great intensity, its probably time to visit a physical therapist to begin easing the pain.
Another telltale sign? The sciatic nerve can become compressed in the area that controls bladder and/or bowel function. If you lose control of either or both of these functions, youll obviously want to get professional help. Visit a doctor to rule out other problems. She will likely run tests, as well as refer you to a physical therapist.