How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Kathryn P Moore, Movement Disorders neurologist at Duke Health, a Parkinson’s Foundation Center of Excellence.
How Can I Help My Loved One
Your loved ones hallucination episodes are certainly disturbing, but they are usually harmless. Unlike hallucinations caused by other neurodegenerative diseases, hallucinations associated with Parkinsons disease are most often benign.
Not all hallucinations need to be treated. If they do not disrupt your loved ones daily life, there are ways to manage them well. It is still important to inform your neurologist for proper follow-up.
Talk to your loved one about their hallucinations. Together, determine what you can do when they are having a hallucination. This will help both of you be prepared and reassured when it happens.
If the hallucinations are severe, do not tell your loved one that the hallucinations are not real. This will only increase the disparity between reality and the hallucination. It may also create unnecessary conflict with your loved one who is convinced that they are hallucinating.
Study Design And Patients
This study involved data obtained in 40 PD patients and in 22 age- and sex-matched healthy controls, most of whom were included in a previously published study28, which was performed in the OLVG West between July 1, 2017 and November 21, 2017. In summary, all included patients were diagnosed with PD by a neurologist specialized in movement disorders, fulfilled the UK Parkinsons Disease Society Brain Bank Criteria, had a modified Hoehn and Yahr stage between 2 and 5, had a disease duration of at least three years and were older than 50 years. Exclusion criteria for all participants were a neurodegenerative disorder other than PD, and a visual acuity of the best eye below 0.1. The study was performed in accordance with the Declaration of Helsinki Principles and the study protocol was approved by the Medical Ethics Committee of Amsterdam UMC, location VU University Medical Centre in Amsterdam, the Netherlands. All participants provided written informed consent.
For the present study, we included three patients that were excluded from our earlier study: two patients with strabismus and one patient with amblyopia. In these three cases, only the healthy eyes were included in the analysis. Furthermore, we excluded the eyes of participants with glaucoma or an intra-ocular pressure of 21 or higher and the eyes where the segmentation was unreliable due to insufficient OCT scan quality . Patients were examined while they were in the on state.
Recommended Reading: Can A Child Have Parkinson Disease
Next Step: Get A Health Screening
If you think you may have had your first hallucination, its important to talk to your health provider about whats going on. Especially if your hallucinations have come on quickly or are dramatically different, there may be something else going on, like a urinary tract infection, which is associated with cognitive changes in older patients, says Melita Petrossian, M.D., a neurologist at Providence Saint Johns Health Center in Santa Monica, CA. You may also be having vision issues, so that should also get checked, as well as your mental health.
Pdps Impact On Caregivers
As Susans story demonstrates, PDP is difficult for both the patient and their caregivers, particularly because it is impossible to convince someone that their delusions are not real. Logic does not penetrate. In fact, accusations of spousal infidelity are often the last straw when caregivers find caring for their loved one too overwhelming. One of the major problems in dealing with PDP is that the patient and the family often try to hide the problem the patient for fear of being thought crazy and the caregiver due to embarrassment. The reality is that when a Parkinsons Disease patient has psychotic symptoms, his or her mental abilities will be otherwise normal. The patient may not be disoriented, can still balance their checkbook and recall everything theyre supposed to know. When hallucinations or delusions occur, the treating doctor should be notified. No irreversible harm will occur if treatment is delayed, but it is unlikely the problem will go away on its own.
Also Check: Early Diagnosis Of Parkinson’s Disease
What Are The Types Of Parkinsons Hallucinations
Hallucinations can affect any of the five senses:
- Sight . Seeing something that isnt there, such as insects crawling on the walls or a deceased relative.
- Hearing . Hearing voices or sounds that arent real.
- Smell . Smelling an odor that isnt there, like cookies baking or a skunks spray.
- Feeling . Feeling imaginary things, like bugs crawling on your skin.
- Taste . Having a strange taste in your mouth that isnt from something youve eaten or a medical condition.
Some people sense the presence of a person or an animal nearby. Others see real objects transform into other things for example, a vase changes into a dog.
Its more common to have hallucinations at night, when the darkness creates shadows. Hallucinations can last anywhere from a few seconds to a few minutes.
Early in the disease, most people with Parkinsons psychosis have insight, which means they understand that what theyre experiencing isnt real. Later in the disease, often people lose insight and believe that what they see, hear, or feel is real.
Parkinsons Disease Psychosis: A Little
One of the lesser-known symptoms of Parkinsons Disease is Parkinsons psychosis. This webpage explains the prevalence, causes and symptoms, treatment options of PD psychosis. More useful to caregivers are sections on potential triggers of psychotic episodes and what caregivers can do about PD psychosis.
Also Check: How Does Parkinson’s Disease
What Is A Hallucination
A hallucination is a perception of something that does not actually exist. This may be visualised, heard, felt, smelled or tasted. Hallucinations are sometimes confused with illusions, which are distortions of a reality rather than something that is purely imagined – as with hallucinations.
Visual hallucinations: In Parkinson’s, hallucinations are most commonly visual and may be in black and white, in colour, still or moving. Often the images involve small animals and children. They may disappear quickly or may last for some time.
Auditory hallucinations: auditory hallucinations are less common. These generally involve hearing voices or other familiar sounds. Auditory hallucinations can also be part of a depressive symptomatology.
Tactile hallucinations: hallucinations may be tactile, that is, you may feel a sensation, like something touching you.
Smell and taste hallucinations: less commonly you may feel that you can taste something you havent eaten, or you may smell something that is not present, such as food cooking or smoke.
Usually hallucinations are not threatening or distressing. If you hallucinate you may be unaware that your perceptions are not real, and sometimes imagined images or sensations can be comforting. But hallucinations can also be distressing and you may feel threatened or frightened and may need reassurance and comfort from those around you.
How Common Are They
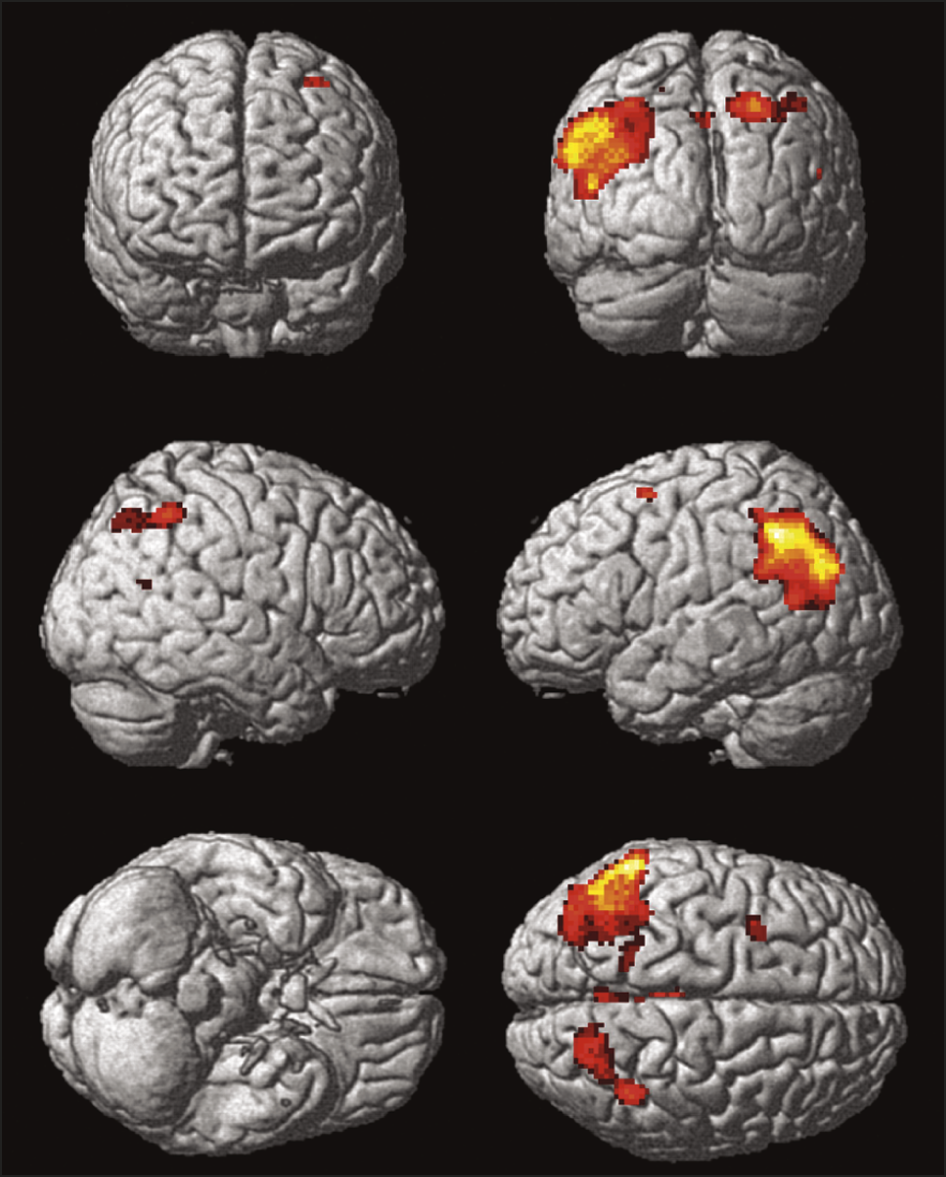
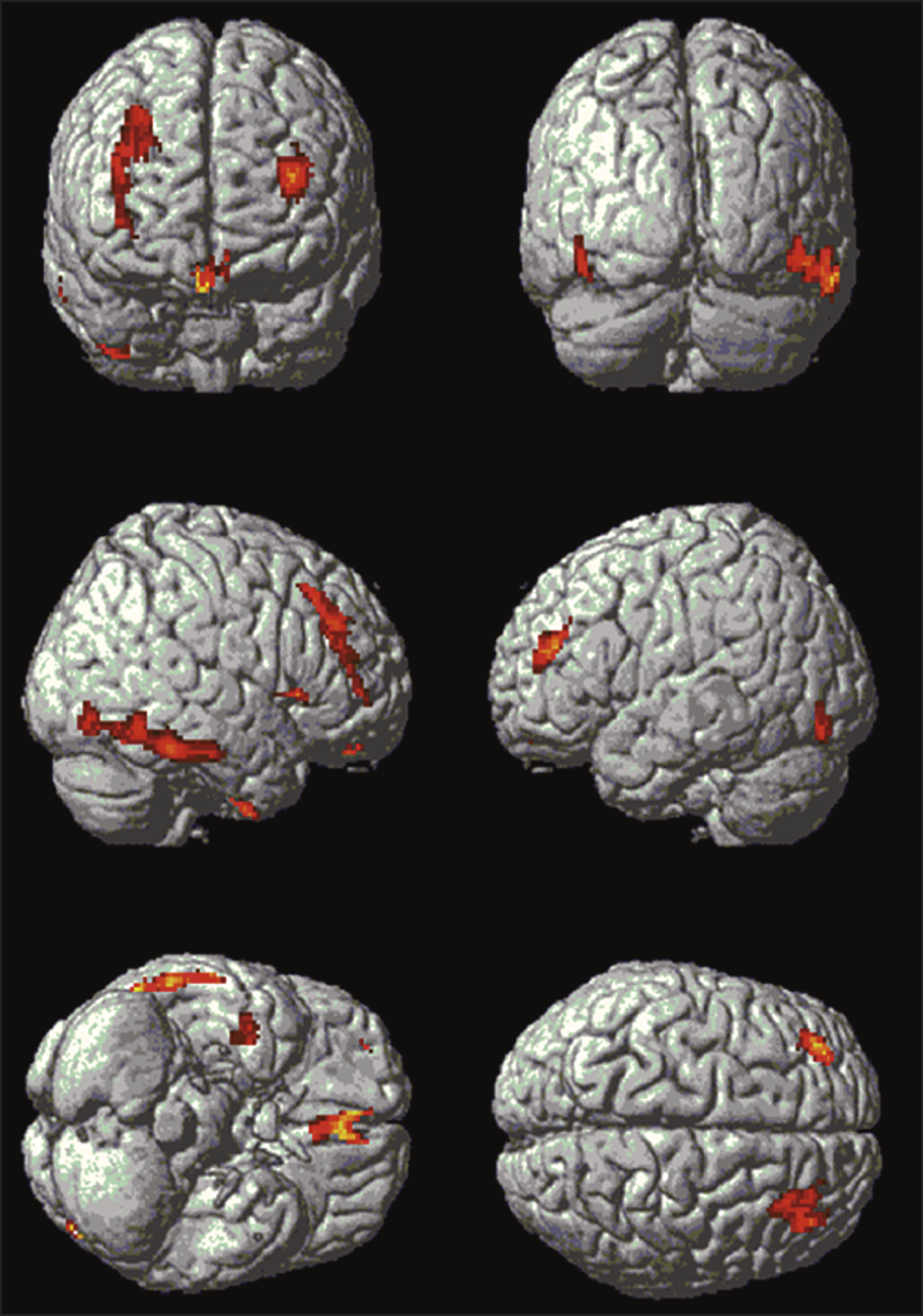
According to the Parkinsons Foundation, about 20% to 30% of people with PD experience psychosis, which includes visual hallucinations. At early stages , hallucinations may occur because of changes in the way the brain transmits information to the visual cortex, says Ritesh Ramdhani, M.D., a neurologist at Lenox Hill Hospital in New York City. These hallucinations can change as the disease progresses, but they usually start as minor and not distressing.
Recommended Reading: Early Onset Parkinson’s Tremor
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication youre taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldnt be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Get The Every Victory Counts Manual For Care Partners
Do you have the Every Victory Counts Manual for Care Partners! Released in 2021, this resource is available at no cost in print and digital versions. To learn more and request your copy, .
This content was supported in part by Acadia Pharmaceuticals. To learn more about Parkinsons disease psychosis, visit moretoparkinsons.com
Read Also: Does Sam Waterston Have Parkinson
Comparison Of Hallucinators And Non
The patients with isolated minor hallucinations were compared with the patients with no hallucinations . The only significant difference was a higher CES-D score in the group with minor hallucinations . When the presence of depression was determined using the cut-off values of the CES-D, depression was more frequent in the patients with minor hallucinations than in the patients without any hallucinations , but this difference did not reach significance.
The patients with formed visual hallucinations are compared with the non-hallucinators in Table 5. Patients with visual hallucinations differed in a number of respects: they were older, had a longer duration of disease, had a more severe motor state, had more depressive symptoms, and were more likely to have cognitive impairment, day-time somnolence and a history of ocular pathology. They were less likely to receive anticholinergics or selegiline and received a higher daily dose of levodopa, but the levodopa-equivalent dose did not differ significantly between the two groups. Visual hallucinations were recorded in 70% of the patients with dementia versus 10% of non-demented patients , and in 55% of the patients with severe cognitive disorders versus 8% of the patients with absent or moderate cognitive impairment .
The patients with hallucinations of any type were compared with the patients with no hallucinations. The results were identical to those of the preceding analysis, except for the degrees of significance .
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Recommended Reading: Is Insomnia A Symptom Of Parkinson’s Disease
A Caregivers Guide To Parkinsons Disease Psychosis
While more than 50% of those taking carbidopa-levodopa may experience psychosis , medication management of these symptoms is a balancing act. First, families must bring psychotic behavior to the attention of your medical team. Medical causes of the behavior, like infection must be ruled out, followed by a review of medications and possible medication adjustments before a lifestyle changes and possible medications for treatment are added.
Predictive Factors And Pathophysiology
Minor hallucinations/illusions
Patients with isolated minor hallucinations/illusions differed from patients without hallucinations only by the presence of more depressive symptoms on the CES-D rating scale, suggesting that depressive symptoms are a facilitating factor. Indeed, depression may sometimes trigger or aggravate hallucinations associated with deafness or ocular pathology . However, when we analysed depression according to CES-D cut-off scores, the difference between the Parkinson’s disease patients with minor hallucinations/illusions and those with no hallucinations was not significant. Interestingly, hallucinations involving the deceased spouse have been reported in up to half of widowed persons, with a higher frequency in the elderly . In the present study, the `presence’ was that of a deceased relative in only three cases bereavement cannot therefore explain the bulk of the cases.
Dopaminergic agents and other treatments
In the present study, non-hallucinators were more likely to be on anticholinergics or selegiline than patients with hallucinations. A similar paradoxical, negative association between anticholinergics and hallucinations was found by Sanchez-Ramos and colleagues . This reflects the recommendation whereby the use of these drugs in patients with cognitive impairment is avoided because of the well-known risk of cognitive worsening and/or hallucinations in this population.
Cognitive impairment
Sleepwake disturbances
Motor status
Depression
Also Check: Can You Have Parkinson’s At A Young Age
What Are Parkinsons Hallucinations
Symptoms of psychosis occur in up to 50% of people with Parkinsons disease.
Parkinsons disease psychosis is considered a neuropsychiatric condition. This means it involves neurology and psychiatry . While the psychosis involves mental health symptoms, they are caused by Parkinsons disease, which is a disease of the nervous system.
Psychosis in Parkinsons disease comes in two forms:
- Hallucinations: Sensory experiences that are not really happening
- Delusions: False beliefs not based on reality
These symptoms can be debilitating and scary for the people experiencing them. They can interfere with a persons ability to care for themselves and to relate to other people.
Psychotic symptoms in Parkinsons disease are associated with increased caregiver distress, risk of hospitalization and nursing home placement, and healthcare costs.
A study suggests the presence of hallucinations and delusions in people with Parkinsons disease is a predictor of mortality .
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD. They cause limited worsening of PD while treating hallucinations and delusions.
Also Check: What Do Lewy Bodies Do In Parkinson’s Disease
Some Examples Of Delusions And Their Impact In Pd Include:
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression
Demographics And Clinical Scores
Demographic results are summarized in Table 1. All groups were matched for age and there were no significant differences in duration of PD or levodopa dose between the PDD-CVH and PDD-NCVH groups. PDD patients displayed a significant reduction in global cognitive function, UPDRS motor score relative to controls, with the PDD-CVH group global cognitive function and motor function were significantly worse when compared to the PDD-NCVH group. The NPI recorded the severity of hallucinations as mild in 29.4% PDD-NCVH which were phenomenologically classified as Illusions , presence , shadow , and simple by the NEVHI. Further stringent grouping into PDD_NVH dropped the reporting of mild hallucinations to 10%.
Table 1. Participant demographics and clinical scores.
You May Like: Can Citalopram Cause Parkinson’s
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that arent real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what theyre seeing isnt real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the persons doctor. If their symptoms dont improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
How To Care For Someone Who Experiences Delusions
If the person youre caring for experiences confusion or delusions, heres what you can do in the moment:
- Stay as calm and patient as you can and remember that this belief has nothing to do with you and only with what is going on in their mind
- Remove any objects in the room that could pose a danger to them or to anyone else
- Clear space so there are no tripping hazards and its easy for the person to move around
- Do not try to reason with the person or convince them why their belief is false
- Reassure them that everything is going to be okay
- If the person becomes aggressive, minimize your movements and remain calm
- Ask the person to talk to you about what they are feeling and really listen to them so they dont feel threatened
- If you feel like you or they are in danger, call 911
Here are a few actions you can take once the delusion has passed:
- Inform their doctor immediately
- Educate others who may care for the person how to handle the situation if it happens
- If the person is open to it, discuss it with them and ask them to explain what the experience is like for them and if theres anything different you could do next time
- Seek expert advice if you feel like you need support in managing these episodes
You May Like: Is Neuropathy A Sign Of Parkinson’s
How Commonly Do Parkinsons Disease Patients Develop Psychosis
Psychosis in Parkinsons disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinsons disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinsons disease patients . In the early stage of Parkinsons disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinsons disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.
