The Parkinsons Disease Medication Pipeline
The pipeline for Parkinson’s disease medications is extremely crowded these days, with multiple medications at various stages of research development. This is very exciting news for the PD community and is a perfect example of the “hope in progress” part of our organization’s motto. It is thrilling to see the research that is underway, especially the potential treatments that have already made it to the clinical trial phase of development. However, this progress brings with it the welcome challenge of keeping track of all the potential compounds that are in research development! Recently, was published in the Journal of Parkinson’s Disease which cataloged the 145 compounds that are currently being studied in humans via clinical trials for PD. This is a staggering number and is even more exceptional when you consider the many more compounds that are not quite yet ready for human trials, but are currently being studied in the laboratory in test tubes, cell culture or animal models of PD. The number also does not account for compounds that have been studied in small clinical trials, garnered promising data, and will be studied in larger clinical trials in the near future – but are not being tested in clinical trials right now.
Some background on the review
Physical And Supportive Therapies
People with Parkinson’s disease should remain as active as possible, maintaining daily activities and, if possible, a regular exercise program. Support therapies from physiotherapists, occupational and speech therapists can also help with specific exercises, education and retraining to improve coordination, balance and movement. Overall fitness and good muscle tone can help minimise some of the abnormal movements associated with Parkinson’s disease.
The facts on medical cannabis for treating Parkinson’s
To date, no large-scale studies or peer reviewed scientific research have established the safety and effectiveness of medical cannabis for treating the symptoms of Parkinson’s.
There have been a small number of randomised controlled trials conducted but these studies were too small to be meaningful and inconsistent in their approach.
Parkinson’s NSW supports appropriate, ethical scientific research into the therapeutic benefits of medical cannabis. However, evidence of its safety and effectiveness is currently lacking.
Therefore, Parkinson’s NSW does not endorse the use of medical cannabis for the treatment of Parkinson’s.
We recommend that you do not rely on the internet, social media or word of mouth for information about medical cannabis.
If you are considering any form of unproven therapy, first talk to your GP and neurologist about the potential benefits, risks and costs involved.
References
Warning!
Supporting You
Medication For Parkinsons Disease
Once the doctor diagnoses Parkinson’s disease, the next decision is whether a patient should receive medication, which depends on the following:
-
The degree of functional impairment
-
The degree of cognitive impairment
-
Ability to tolerate antiparkinsonian medication
-
The advice of the attending doctor
No two patients react the same way to a given drug, therefore, it takes time and patience to find an appropriate medication and dosage to alleviate symptoms.
Latest Treatments For Parkinsons Disease
Researchers still have much to learn about Parkinson’s disease. As researchers continue to work hard in the fight against this disease, the lessons they learn may lead to new, innovative treatments.
Parkinson’s disease is a neurodegenerative disorder that affects dopaminergic neurons in the substantia nigra area of the brain, advises the Parkinson’s Foundation. Even though the disease itself is not fatal, PD is a serious condition — one which the Centers for Disease Control and Prevention rates as the 14th most common cause of death in the United States due to the disease’s related complications.
PD symptoms affect autonomous functions and the ability to move limbs. The Mayo Clinic notes that most people with PD may show little or no expression, speech may become slurred, arms may not swing when one walks, and stiffness and gait issues may become apparent. PD can affect balance and posture as well.
There is no cure for PD, but there are many different treatments that can slow its progress and reduce symptoms.
WebMD says new treatments for PD give individuals continued hope. Here’s a look at some of the potential options.
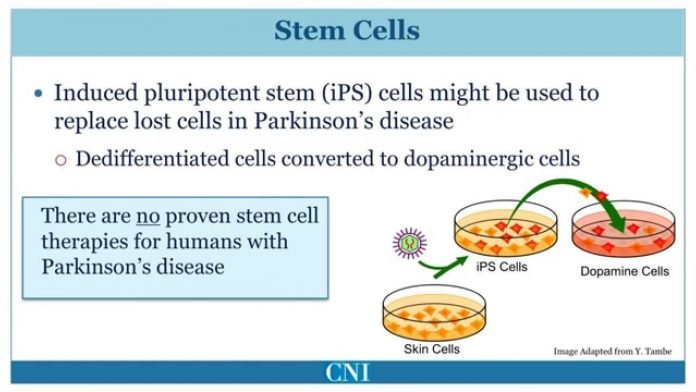
Stem cell usage?tem cells can turn into any type of cell, and there is hope that they can transform into the dopamine-producing neurons used to treat PD. But there is increased risk of involuntary movement from too much dopamine with this treatment. Stem cell therapy also may present ethical and moral issues with some patients.
Signal Contributor
As A Person Explains Their Off Period Its More Of A Sad Testimony Because Youre Sharing What Youre Missing In Life

Steven D., Living with Parkinson’s Since 2005
Co-Chair of the PwP Advisory Board & Founder and CEO of the Connecticut Advocates for Parkinson’s
In a 2014 survey conducted by the Michael J. Fox Foundation, 64% of approximately 3,000 people living with Parkinson’s reported that they spent two or more hours per day in OFF periods15
What Are The Latest Approved Treatments For Parkinsons Disease
Several medicines have been approved for the treatment of Parkinson’s disease. Here are some of the available medicines for Parkinson’s disease:
Nuplazid 3,4
Nuplazid was approved for the treatment of patients with hallucinations and delusions associated with Parkinson’s disease psychosis by the Food and Drugs Administration on April 29, 2016. On December 3, 2020 The approved an update to the prescribing information for Nuplazid that will allow the medication to be taken more easily by Parkinson’s patients who have difficulty swallowing.
Ongentys 5,6
Ongentys is a medication used for the treatment of Parkinson disease. It is indicated for the treatment of adult patients with Parkinson disease. It is used as an add-on to levodopa/DOPA decarboxylase inhibitors in patients who are having fluctuations in the control of their condition.
Opicapone was approved for treating patients with Parkinson’s Disease as an add-on to levodopa/DOPA decarboxylase inhibitors in patients who are having fluctuations in the control of their condition by the European Medicines Agency on June 24, 2016 and by the Food and Drug Administration on April 24, 2020.
Nourianz/Nouriast 7,8,9
Nourianz/Nouriast was approved by the Food and Drug Administration , USA, on August 27, 2019 and by the Pharmaceuticals and Medical Devices Agency , Japan, in June 2013.
Inbrija 10,11,12
What Are The Side Effects Of Too Much Carbidopa Levodopa
Dizziness, lightheadedness, nausea, vomiting, loss of appetite, trouble sleeping, unusual dreams, or headache may occur. If any of these effects persist or worsen, tell your doctor or pharmacist promptly. This medication may cause saliva, urine, or sweat to turn a dark color.
READ: Why did Bud drive away with Lefty Lewis car?
Advances In Deep Brain Stimulation
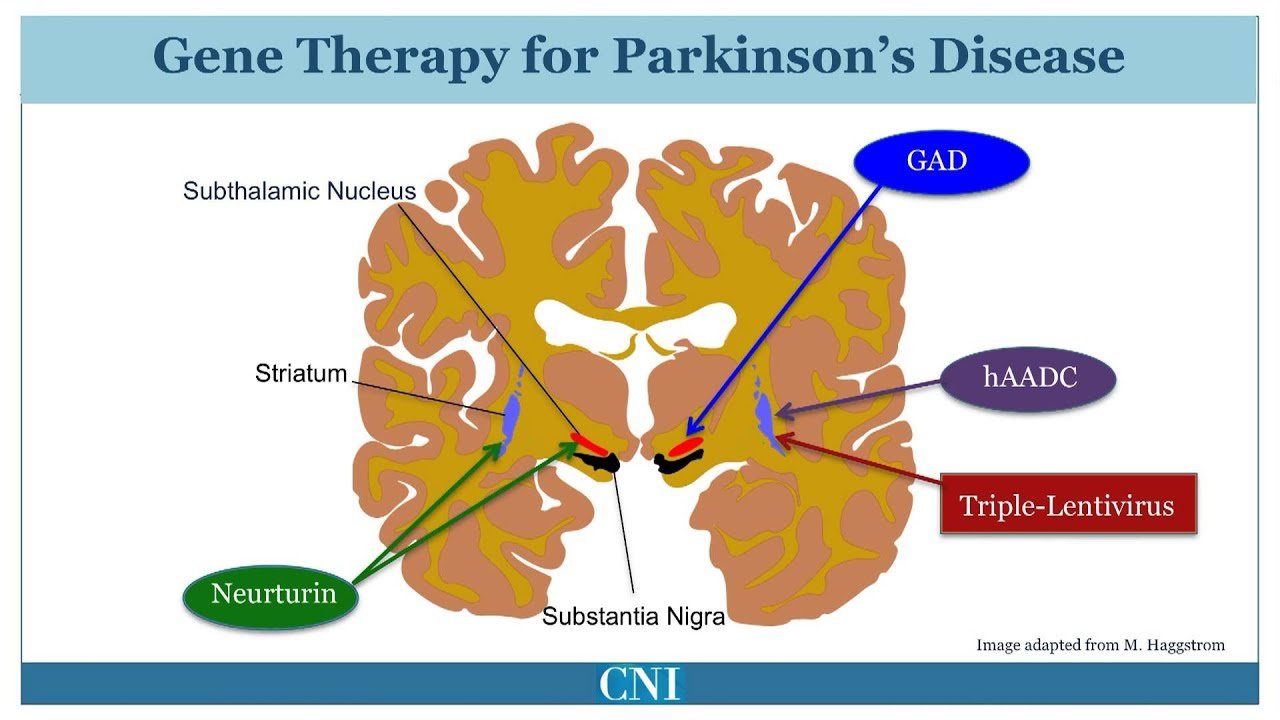
Deep brain stimulation is another established treatment for PD that is useful in treating dopamine-dependent motor symptoms when levodopa-induced side effects become particularly problematic. DBS involves the surgical implantation of electrodes that stimulate subcortical structures including the subthalamic nucleus and globus pallidus internus–. DBS offers significant improvements in motor symptoms and fluctuations in comparison to best medical therapy in some advanced PD patients, but dopamine-resistant symptoms other than tremor respond poorly. It has also been suggested in an open-label trial that DBS is beneficial in early PD patients, with improved tremor scores and reduced development ofde novo tremor. In addition to surgical complications, DBS strategies may cause cognitive and neuropsychiatric adverse effects as well as speech dysfunction. Novel DBS approaches, including adaptive DBS, targeting different regions, and refined intra-operative imaging techniques promise to offer improved clinical applicability and reduce the impact of adverse effects.
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Vocal Symptoms
Add On To Dopamine Agonist
Safinamide has been studied also as an add on to dopamine agonist monotherapy. Two study has been conducted. The 015 study was a double-blind controlled trial where safinamide 100 and 200 mg/day were added to a stable dose of dopamine agonist. The study demonstrated a significant improvement of the UPDRS III total score, UPDRS part II and CGI-C in the safinamide 100 mg group; the percentage of responders was higher in both safinamide groups compared to placebo. In this study, the dose of 200 mg failed to reach significance. The MOTION study was a 6-month , randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of two fixed doses of SAF . This trial enrolled patients with early idiopathic PD treated with a single dopamine agonist. Six hundred and seventy-nine patients were randomized to receive safinamide 50 mg once daily, 100 mg, or placebo. Six hundred and seven patients completed the 24-week treatment period. Safinamide 100 mg/day significantly improved UPDRS III , and PDQ-39 compared to placebo. There was borderline significant improvement in ADL for the 100 mg/day, as well as UPDRS III for the 50 mg/day group.
Post-hoc analyses of pooled data confirmed improvement in motor symptoms by UPRDS III and in cardinal symptoms with 100 mg/day.
Safinamide has also shown to be effective in improving ON and OFF time in addition to levodopa alone or with any combination of antiparkinsonian therapies.
Could You Remind Us Of What Sort Of Care You Received What Treatments Are You Taking Are They Effective
My treatment at the moment is:
- 6:00 AM : 1 Duopa 125 mg + 1 Azilect
- 7:30 AM: 1 Mirapex 2.10 mg + 1 Mirapex 1.05 mg
- 9:00 AM: 1 Duopa 62.5 mg
- 12:00 PM: 1 Duopa 125 mg
- 3:00 PM: 1 Duopa 62.5 mg
- 6:00 PM: 1 Duopa 125 mg
- 10:00 PM: 1 Duopa 125 LP + 1 Duopa 62.5 mg
And if I need it at night, I take 1 Duopa 62.5 mg.
It took more than a year to find this right dosage, and I think it suited me before, but with all the work I’m doing on myself and feeling better and better, I hope my neurologist will lower it soon.
Because I haven’t told you yet that my next goal is to put my Parkinson’s into remission! I don’t say cure, let’s not delude ourselves! After all, every year around the world, we hear these kinds of experiences where doctors don’t know why but people manage to do it.
What Is Fetal Cell Transplantation
Fetal cell transplantation is a procedure in which fetal cells are implanted into the brains of people with Parkinson’s disease to replace the dopamine-producing cells in the substantia nigra. Although promising, this area of research is one of the most controversial. Some studies have found that fetal cell transplantation caused an increase in severe involuntary movements due to too much dopamine in the . There are also moral and ethical objections to the use of fetal cell implants. As a result, other methods of treatment are being explored.
The Latest Developments In Parkinsons Treatment: What Patients And Caregivers Need To Know
Select Justice » » The Latest Developments In Parkinson’s Treatment: What Patients and Caregivers Need To Know
It’s devastating to watch a loved one live with Parkinson’s disease. The progressive condition doesn’t just affect the person with the diagnosis — it’s also hard on caregivers, who are often forced to make difficult decisions on how to care for their loved one.
Medications for Parkinson’s can significantly help the motor issues associated with the disease. Current Parkinson’s treatments only fight symptoms, however — they do nothing to stop the progression of the disease, which is caused by a loss of neurons.
Research on potential causes of and treatments for Parkinson’s disease is ongoing. Recent research has shown a possible link between pesticide exposure and the development of Parkinson’s disease, particularly in regards to the pesticide paraquat. Researchers are hopeful that new treatment protocols continue to effectively fight the symptoms of Parkinson’s disease-related to pesticide exposure.
Parkinson’s disease research can be devastatingly slow. To speed treatment research, the Coalition Against Major Diseases has created a data-sharing partnership between non-profits, pharmaceutical companies, and government organizations to spearhead Parkinson’s research in the most efficient way possible.
Here, we’ll explore the latest treatments for Parkinson’s disease, as well as the treatment advancements that are likely to be made in the coming years.
Advanced And Future Treatments For Parkinsons
Graham Rogers, M.D.Kimberly Holland
While there’s no cure for Parkinson’s disease, recent research has led to improved treatments.
Scientists and doctors are working together to find a treatment or prevention technique. Research is also seeking to understand who is more likely to develop the disease. In addition, scientists are studying the genetic and environmental factors that increase the chance of a diagnosis.
Here are the latest treatments for this progressive neurological disorder.
In 2002, the FDA approved deep brain stimulation as a treatment for Parkinson’s disease. But advances in DBS were limited because only one company was approved to make the device used for the treatment.
In June 2015, the FDA approved the
Help Your Patients Uncover The Troublesome Symptoms Of Off Periods9
Both physicians and patients agree: OFF periods can be one of the most difficult aspects of Parkinson’s disease. It’s understood that recognizing the symptoms of OFF periods is challenging because of a variety of reasons, including interpatient symptom variability and reliance on patient reporting.9
People with OFF periods may not discuss their symptoms or communicate the impact of the symptoms to their healthcare provider as they may be unaware that the changes they are experiencing are a result of OFF periods. Because patients may not recognize the more subtle changes they are experiencing as symptoms of OFF periods, enhancing communication around the full spectrum of symptoms is important.9
Instead Of Burning Your Writings As You Say In Your First Testimonial You Chose To Publish Them Why Did You Do This What Do You Write About
Yes, I realized that everything I had written could perhaps help other people, so the idea of putting it all together and making a book was natural to me.
I’m not a writer, so it’s written very simply with ordinary words. As it was originally only for me, there are personal things, I thought I would take them out, but at the same time they are part of life and can help. I’m talking, for example, about constipation problems and all that it causes, we know that Parkinson’s sufferers are very much affected by this and as I’ve found a solution that helps me enormously, I’ve decided to leave everything.
I am therefore “laying myself bare” so that all my feelings are clear.
I also decided that this book would serve as a basis for me to go and speak at hospitals and other places.
I was admitted for a week at the regional hospital center in Lille to assess my condition and treatment and well, they couldn’t believe that my Parkinson’s hadn’t progressed when I explained all that I had been up to in my daily life.
You Have Been Seeing A Hypnotherapist As Well What Benefits Do You Get From Hypnosis
I have been seeing a hypnotherapist for 3 years now. Hypnosis has been a revelation for me and it is not unrelated to the benefits I feel. Today, it helps me mentally, spiritually and even in terms of my strength, it helps me to look within myself and understand myself better. Thanks to her, today, I am much more serene about the things that happen in my life.
I live my life as I have never lived it before, I have learnt to put things into perspective, I no longer get caught up in futile things.
But do know, this requires a lot of work at the beginning and I’m still not there yet. It’s an ongoing process but I do enjoy it as well.
Who Can Get It
While anyone can develop Parkinson’s disease, age is the greatest factor in receiving a diagnosis. The average age of developing this disease is 60, and men are more likely to receive a diagnosis than women. Having a close relative, like a parent or sibling, who has Parkinson’s disease doubles your risk factor.
Assembling Your Care Team
Assembling a team that will provide you with physical and emotional support and adapt to your needs over time is one of the best ways to remain healthy. Parkinson’s disease is complex and requires an interdisciplinary approach to care. The care team may include, but is not limited to:
- Movement disorder specialist
- Rehabilitation specialists including physical, occupational, and speech therapists
- Nurse
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
Phase One To Phase Two
Nineteen Australian Parkinson’s patients were recruited for the trial, and 18 were administered the drug, in three different volumes: Small, medium and large.
Dr Evans said he expected to see – at best – the participants’ disease remain at the same level.
What he observed surprised him.
“But it was shown not only that people got better, they improved in signs and symptoms of Parkinson’s,” Dr Evans said.
“This was more marked in higher-dose groups, who were given 72 milligrams of the drug a day.
“I was playing it down to patients at the start, saying, ‘This probably won’t make you feel better’. But people were coming back saying, ‘I feel better on this drug’.”
Dr Evans theorised the drug was effective because of the way it activated affected neurones.
In Parkinson’s disease, some neurones are dead, and some are sick, while some remain functioning.
“What the drug has done is bring back those sick neurones into functioning well,” he said.
Photo: Getty
With just a couple of final assessments to be made in phase one, researchers are already looking to phase two, which will involve more trials over longer periods of time and larger control groups.
“The challenge in Parkinson’s is that it is a very slowly progressing disease,” Dr Evans said.
“… if you’re just slowing the progress of the disease, you do need to study people for longer.
“But if this drug holds up … maybe we can get in a shorter amount of time.”
Photo: Getty
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
New Study Gives Clue To The Cause And Possible Treatment Of Parkinson’s Disease
Zebrafish model research reveals clues about molecular triggers of Parkinson’s Disease
Niigata University
image: Immunostaining: Top panel SH-SY5Y cells transfected with GBA, ATP13A2, and PINK1 siRNAs are stained for dsDNA , histone H2B and Hsp60 . White arrows indicate cytosolic dsDNA of mitochondrial origin. Triple siRNA: Knockdown of GBA, ATP13A2, and PINK1 expression with siRNAs. Coimmunostaining: Bottom panel In situ hybridization of mitochondrial DNA and coimmunostaining for histone H2B and Hsp60 in SH-SY5Y cells transfected with GBA, ATP13A2, and PINK1 siRNAs. White arrows indicate cytosolic dsDNA of mitochondrial origin. Triple siRNA: Knockdown of GBA, ATP13A2, and PINK1 expression with siRNAs.view more
Niigata, Japan – Researchers from Brain Research Institute, Niigata University, Japan may have unraveled a new approach that could revolutionize the treatment, prevention, and possibly reversal of the damages that could lead to Parkinson’s Disease . This novel finding utilizing the cellular and zebrafish models, demonstrated how the leakage of mitochondrial dsDNA into the cytosol environment of the cell can contribute to the impairment of brain tissue of patients with PD.
Parkinson’s disease is the second most common neurodegenerative disease, and its prevalence has been projected to double over the next 30 years.
###
Journal
DOI
10.1038/s41467-021-23452-x
Media Contact
Garment Technologies To Prevent Falls
Frequent falls, owing to faulty gait and posture are common among people with Parkinson’s Disease. A team of researchers are in the process of developing smart garment technologies that would prevent falls in people with this neurological condition. The researchers from Neuroscience Research Australia and University of New South Wales are set to make StandingTall-PD, a neuro-rehabilitation programme that aims to prevent freezing-of-gait and falls, and enhance patients independence. The programme uses visual, audio and haptic sensory cues to help rewire the parts of the brain that control walking and prevent falls. The combination of visual, audio and sensory elements helps to form new connections in the less affected parts of the brain, leading to improved walking ability, the researchers said.
Existing dopamine therapies offer benefit in treating motor dysfunction in Parkinson s but may not alleviate gait and balance challenges, said Jamie L. Hamilton, Associate Director at the Michael J. Fox Foundation in the US.
The new programme has the potential to become an affordable option to address gait and balance issues and improve overall quality of life for people with Parkinson s, added Hamilton.
For the study, researchers will give participants a mat with colour-coded stepping targets, a pair of Sensoria Smart Socks, an iPad and phone.
What Will A Cure For Parkinson’s Look Like
Because Parkinson’s varies so much from person to person, there may not be a single ‘cure’.
Instead we may need a range of different therapies to meet the needs of the individual and their specific form of the condition.
This mix may include treatments, therapies and strategies that can:
- slow or stop the progression of the condition
- replace or repair lost or damaged brain cells
- control and manage particular symptoms
- diagnose Parkinson’s at the earliest possible stage.
And this could involve medical treatments, such as drugs and surgical approaches, as well as lifestyle changes, for example to diet and exercise.
Surgery For Parkinsons Disease
Based on the severity of the condition and the medical profile, the doctor may recommend surgery as one treatment option for Parkinson’s disease.
There are several types of surgery that may be performed that can help patients with Parkinson’s disease. Most of the treatments are aimed at helping the tremor or rigidity that comes with the disease. In some patients, surgery may decrease the amount of medication that is needed to control the symptoms.
There are three types of surgeries that may be performed for Parkinson’s disease, including the following:
It is important to remember that surgery may help with symptoms of Parkinson’s disease, but does not cure the disease or stop the progression of the disease.