Is Early Diagnosis Possible
Experts are becoming more aware of symptoms of Parkinsons that precede physical manifestations. Clues to the disease that sometimes show up before motor symptoms and before a formal diagnosis are called prodromal symptoms. These include the loss of sense of smell, a sleep disturbance called REM behavior disorder, ongoing constipation thats not otherwise explained and mood disorders, such as anxiety and depression.
Research into these and other early symptoms holds promise for even more sensitive testing and diagnosis.
For example, biomarker research is trying to answer the question of who gets Parkinsons disease. Researchers hope that once doctors can predict that a person with very early symptoms will eventually get Parkinsons disease, those patients can be appropriately treated. At the very least, these advances could greatly delay progression.
Parkinson’s Disease and Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
What Should I Expect During The Mri
As the MRI scan begins, you will hear the equipment making a variety of banging, clanging and muffled thumping sound that will last for several minutes. None of them are anything other than annoying. Other than the sound, you should experience no unusual sensations during the scanning.
Certain MRI exams require an injection of a contrast material. This helps identify certain anatomic structures on the scan images.
Please feel free to ask questions. Tell the technologist or the doctor if you have any concerns.
Mri And Pet Reveal Parkinsons Is Two Diseases
Advanced imaging shows Parkinsons can begin as brain-first or body-first.
Its been a long-standing question in neuroscience: is Parkinsons more than one disease? Now, thanks to MRI and PET scans, clinicians have an answer yes. And, having this knowledge could pave the way for personalized medicine for these patients.
Based on the analysis of advanced imaging scans, researchers have determined that Parkinsons in, in fact, two distinct conditions one that begins in the intestines and moves to the brain, and one that starts in the brain and migrates to the intestines and other organs.
Until now, many people have viewed the disease as relatively homogeneous and defined it based on the classical movement disorders. But, at the same time, weve been puzzled about why there was such a big difference between patient symptoms, said Per Borghammer, Ph.D., professor of nuclear medicine and neuroscience at Aarhus University in Denmark. With this new knowledge, the different symptoms make more sense, and this is also the perspective in which future research should be viewed.
In addition to the showing the differences between the brain-first and body-first types of Parkinsons, the team also hypothesized that isolated REM sleep behavior disorder a known risk factor for developing Parkinsons could be specifically associated with body-first disease.
The team of Aarhus University researchers published their findings recently in the journal Brain.
Recommended Reading: What Are Early Warning Signs Of Parkinson’s Disease
Further Testing In Parkinson’s
In other situations, where perhaps the diagnosis is not as clear, younger individuals are affected, or there are atypical symptoms such as tremor affecting both hands or perhaps no tremor at all, further testing may help. For example, imaging can play a role in differentiating between essential tremor and Parkinsons. It can also be important to confirm what is initially a clinical diagnosis of Parkinsons prior to an invasive treatment procedure such as surgical DBS
Mri Brain Scans Detect People With Early Parkinson’s
Oxford University researchers have developed a simple and quick MRI technique that offers promise for early diagnosis of Parkinson’s disease.
The new MRI approach can detect people who have early-stage Parkinson’s disease with 85% accuracy, according to research published in Neurology, the medical journal of the American Academy of Neurology.
‘At the moment we have no way to predict who is at risk of Parkinson’s disease in the vast majority of cases,’ says Dr Clare Mackay of the Department of Psychiatry at Oxford University, one of the joint lead researchers. ‘We are excited that this MRI technique might prove to be a good marker for the earliest signs of Parkinson’s. The results are very promising.’
Claire Bale, research communications manager at Parkinson’s UK, which funded the work, explains: ‘This new research takes us one step closer to diagnosing Parkinson’s at a much earlier stage one of the biggest challenges facing research into the condition. By using a new, simple scanning technique the team at Oxford University have been able to study levels of activity in the brain which may suggest that Parkinson’s is present. One person every hour is diagnosed with Parkinson’s in the UK, and we hope that the researchers are able to continue to refine their test so that it can one day be part of clinical practice.’
We think that our MRI test will be relevant for diagnosis of Parkinson’s
Dr Michele Hu
Recommended Reading: Prodromal Dementia
The Role Of Magnetic Resonance Imaging For The Diagnosis Of Atypical Parkinsonism
- 1Institut du Cerveau et de la Moelle épinièreICM, INSERM U 1127, CNRS UMR 7225, Sorbonne Université, UPMC Univ Paris 06, UMRS 1127, CNRS UMR 7225, Paris, France
- 2ICM, Movement Investigations and Therapeutics Team , Paris, France
- 3ICM, Centre de NeuroImagerie de RechercheCENIR, Paris, France
- 4Service de Neuroradiologie, Hôpital Pitié-Salpêtrière, APHP, Paris, France
- 5Dynamics and Pathophysiology of Neuronal Networks Team, Center for Interdisciplinary Research in Biology, Collège de France, CNRS UMR7241/INSERM U1050, MemoLife Labex, Paris, France
- 6Department of Neurology, Avicenne University Hospital, Sorbonne Paris Nord University, Bobigny, France
- 7Département des Maladies du Système Nerveux, Hôpital Pitié-Salpêtrière, APHP, Paris, France
Imaging Biomarkers In Parkinsonism
DaTscan: dopamine-active transporter scans showing binding of 123I-fluoropropyl to DaT protein in the nigrostriatal nerve endings of the striatum. Normal: symmetrical normal specific binding of FPCIT in striatum. Parkinson’s disease: reduced specific binding of FPCIT in the posterior striatum, particularly on the left .
Further imaging approaches are in development on a research basis. 7-T MR scanning can detect structural nigral abnormalities. Diffusion-tensor MRI and diffusion-weighted imaging have shown some promise in diagnosing PD and its mimics. Transcranial sonography can detect hyperechogenicity in the midbrain of patients with PD. Although this is not specific, it may be a marker of susceptibility to PD.,,
Also Check: Journal Of Parkinson’s Disease Impact Factor
Development Of An Mri
Objective/Rationale: Parkinsons disease is associated with accumulation of the protein -synuclein in the brain, however, it is not currently possible to detect -synuclein in the brain of Parkinsons disease patients. This project is aimed at developing a biomarker for the detection of -synuclein, which will provide early non-invasive diagnosis of Parkinsons disease and would greatly improve the clinical development of drugs to treat the disease.
Project Description: In order to be effective for detection of -synuclein, the biomarker must be able to be imaged on MRI and must pass into the brain after injection into the patient. To accomplish both these goals, a fragment from an antibody that detects alpha-synuclein will be linked to a short protein. This short protein will both facilitate passage of the molecule through the blood-brain-barrier into the brain and will also generate a signal on MRI. To test this new molecule, the antibody-short protein complex, or biomarker, will be injected into pre-clinical models that overexpress alpha-synuclein in the brain. After sacrifice, the brains of these pre-clinical models will be sliced and probed for the presence of the biomarker to show that the biomarker crossed through the blood-brain-barrier.
This project was supported with a 2014 supplemental grant to continue work outlined above.
Testing For Parkinsons Disease
There is no lab or imaging test that is recommended or definitive for Parkinsons disease. However, in 2011, the U.S. Food and Drug Administration approved an imaging scan called the DaTscan. This technique allows doctors to see detailed pictures of the brains dopamine system.
A DaTscan involves an injection of a small amount of a radioactive drug and a machine called a single-photon emission computed tomography scanner, similar to an MRI.
The drug binds to dopamine transmitters in the brain, showing where in the brain dopaminergic neurons are.
The results of a DaTscan cant show that you have Parkinsons, but they can help your doctor confirm a diagnosis or rule out a Parkinsons mimic.
Also Check: Is Parkinson Disease Genetic
What Is Parkinson’s Disease
Parkinson’s disease is a disorder that affects the nervous system and movement.2,3 The symptoms typically begin gradually, and it may take a while for patients to notice them. These symptoms may include tremors, slow movement, rigid muscles as well as speech and writing changes. Patients may also experience impaired posture and balance or loss of automatic movements, such as blinking, smiling or swinging their arms.
Parkinson’s has a variety of risk factors that should be considered. In many cases, Parkinson’s usually affects people who are 50 years of age or older.2,3 However, some patients may experience young onset Parkinson’s disease, also called early-onset Parkinson’s disease, which affects roughly 2-10% of the population with Parkinson’s in the United States.3 Men may be more likely to develop Parkinson’s disease than women.2 If a close relative has Parkinson’s disease, a patient may be more likely to develop the disorder. The risk may still be small unless there are a large number of relatives with Parkinson’s disease. Finally, long-term exposure to herbicides and pesticides may slightly increase a patient’s risk.2
Once the disease has begun to progress, there are five stages that patients may experience.
Brain Imaging In Parkinsons Disease
Traditional brain imaging with CT and MRI scans do not show changes in the brain when someone has Parkinsons disease and are generally not helpful in diagnosis. A new kind of brain scan, called a DaT scan, does show changes in persons with Parkinsons disease and may someday become an important tool in diagnosing Parkinsons.
The dopamine transporter, or DaT, scan uses a chemical that labels the dopamine transporter in the area of the brain known as the striatum. Dopamine is a neurochemical that is decreased in persons with Parkinsons disease.
The dopamine transporter, which moves dopamine in and out of cells, is also decreased in the striatum in persons with Parkinsons disease and related disorders. The chemical that labels the transporter is injected into the vein and can be imaged by using something called single photon emission computerized tomography, or SPECT scanning. This technique has been registered in the European Union since 2000 for differentiating a diagnosis of essential tremor and a parkinsonian syndrome. It was approved by the Food and Drug Administration in 2011 for this same indication and recently became available at the OHSU Brain Institute.
Also Check: Frequency Of Parkinsonian Tremor
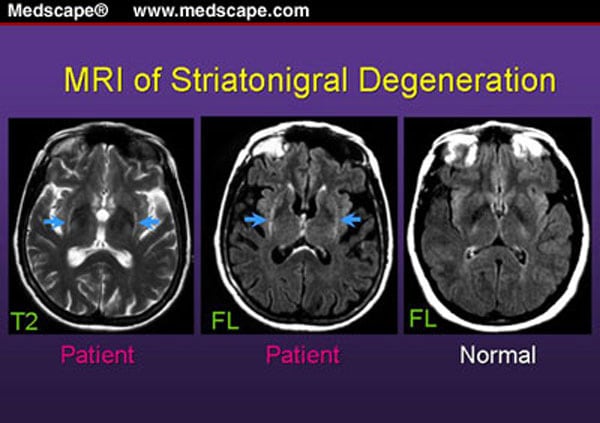
Exclusion Of Symptomatic Parkinsonism
Structural brain imaging using cMRI with visual assessment of T2- and T1-weighted sequences including contrast-enhanced T1 imaging is usually normal in patients with early PD thus, its traditional role is the detection/exclusion of other underlying basal ganglia or brainstem pathologies . These include vascular, space-occupying or demyelinating lesions within the basal ganglia or brainstem, drug- or toxic-induced parkinsonism, e.g. due to manganism, or neurodegeneration with brain iron accumulation , normal pressure hydrocephalus, or infectious causes . Typical MR findings in patients with symptomatic parkinsonism are summarized in Table .
Referral To A Specialist
If your GP suspects Parkinson’s disease, you’ll be referred to a specialist.
This will usually be:
- a neurologist, a specialist in conditions affecting the brain and nervous system
- a geriatrician, a specialist in problems affecting elderly people
The specialist will most likely ask you to perform a number of physical exercises so they can assess whether you have any problems with movement.
A diagnosis of Parkinson’s disease is likely if you have at least 2 of the 3 following symptoms:
- shaking or tremor in a part of your body that usually only occurs at rest
- slowness of movement
- muscle stiffness
If your symptoms improve after taking a medication called levodopa, it’s more likely you have Parkinson’s disease.
Special brain scans, such as a single photon emission computed tomography scan, may also be carried out in some cases to try to rule out other causes of your symptoms.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Casefinding And Diagnostic Procedures
The patients were recruited from an ongoing epidemiological study . In addition, consecutive patients referred to outpatient clinics of the Department of Neurology or the Department of Geriatric Psychiatry, Stavanger University Hospital, Stavanger, Norway, were included . A diagnosis of Parkinson’s disease was made by a neurologist, according to explicit criteria. The minimum requirement for a diagnosis of Parkinson’s disease was at least two of the cardinal signs and a moderate response to a dopaminergic agent. Staging of Parkinson’s disease was carried out according to the Hoehn and Yahr scale. Sample 1 has been followed up prospectively with a 4year interval in 1993, 1997 and 2001 and then assessed annually. The autopsy diagnosis in the first 22 patients, 2 of whom participated in the current MRI study, was consistent with a diagnosis of Lewybody Parkinson’s disease.
What Can You Detect With A Parkinsons Mri
Generally, you can receive a Parkinsons diagnosis in a clinical setting, but an MRI can help to assess various aspects of the disease and its progress. In particular, a Parkinsons MRI can do the following for patients who have or are suspected to have Parkinsons disease:
- Evaluate tissue loss and how the brain is atrophying
- Check for changes to the basal ganglia region of the brain
- Find out if there are abnormal iron deposits in the basal ganglia or brainstem
- Look at changes to white matter
- Examine the diffusion of restricted tissues in acute infarction and neurodegenerative diseases
- Help to diagnose atypical parkinsonism
- Exclude treatable causes of parkinsonism such as normal pressure hydrocephalus
Recommended Reading: Difference Between Parkinson And Parkinsonism
Regional Differences In Gmd Slope Directionality
To further test differences in disease progression between early and PD groups, a comparison of the directionality of the early and PD slope parameters for the age and sex adjusted relationships between duration of disease and GMD was performed. For subcortical regions in early PD, one region had a positive slope, compared to 12 regions which had a negative slope. For subcortical regions in advanced PD patients, all 13 regions had a negative slope. For cortical regions in early PD, 13 regions had a positive slope, compared to one region which had a negative slope. For cortical regions in advanced PD patients, all 14 regions had a negative slope. The difference in the distribution of positive and negative slopes for subcortical and cortical regions in early PD is significant . Additionally, the difference in the distribution of positive and negative slopes for cortical regions between early PD and advanced PD is significant .
How Is A Pet Scan Conducted
A PET scan usually lasts 45-60 minutes. You will first be given the tracer through an IV. After that, the PET scanner, a doughnut-shaped instrument, will move in circles around you. As this is happening, a special camera will take pictures of patterns left by the tracer chemical inside your body.
After the PET scan is finished, you will likely be asked to drink a lot of water or liquids during the next day in order to get rid of or flush the tracer chemical from your system.
Recommended Reading: What Essential Oils Are Good For Parkinson’s Disease
How Is Parkinson’s Diagnosed
Current evidence suggests that Parkinsons tends to develop gradually. It may be many months, even years, before the symptoms become obvious enough for someone to go to the doctor.
This information looks at what parkinsonism is, how Parkinsons and other similar conditions may be diagnosed, and explains some of the tests that may be involved in the process.
Parkinsonism is a term used to describe symptoms or signs that are found in Parkinsons, but which can also be found in other conditions that cause slowness of movement, stiffness and tremor.
Most people with a form of parkinsonism have idiopathic Parkinsons disease, also known as Parkinsons. Idiopathic means the cause is unknown.
Other less common forms of parkinsonism include multiple system atrophy , progressive supranuclear palsy , drug-induced parkinsonism and vascular Parkinsons.
If youre concerned about symptoms youve been experiencing, you should visit your GP. If your GP suspects you have Parkinsons, clinical guidelines recommend they should refer you quickly to a specialist with experience in diagnosing the condition .
Its not always easy to diagnose the condition. So its important that you see a Parkinsons specialist to get an accurate diagnosis and to consider the best treatment options.
Diagnosing Parkinsons can take some time as there are other conditions, such as essential tremor , with similar symptoms. There is also currently no definitive test for diagnosing Parkinsons.
The First Full Body Mri Conditional Portfolio3
Medtronic offers the world’s first full-body MRI capable DBS device portfolio. People with Parkinsons with implanted DBS systems feel reassured knowing that with proper safeguards, MRI is an option for them.
PerceptTM PC neurostimulator is the first and only device to have full-body MR Conditional4 access anywhere on the body for both 1.5T and 3T MRI scans.
You May Like: What Are Early Warning Signs Of Parkinson’s Disease
Determining Diagnosis Through Response To Parkinsons Medication
If a persons symptoms and neurologic examination are only suggestive of Parkinsons disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinsons disease to provide additional information. In the case of idiopathic Parkinsons, there is typically a positive, predictable response to Parkinsons disease medication in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
