Improvement In Severe Orthostatic Hypotension Following Carbidopa Dose Reduction
Published online by Cambridge University Press: 21 December 2017
- Pharmacist Department of Pharmacy Surrey Memorial Hospital Fraser Health Authority Surrey, BC, Canada
- John L. Diggle
- Affiliation:Neurologist and Regional Medical Director and Head Regional Department of Medicine Fraser Health Authority Surrey, BC, CanadaClinical Assitant Professor Faculty of Medicine University of British Columbia Vancouver, BC, Canada
- Penny P. Bring
- Affiliation:Clinical Pharmacy Specialist Neurology Department of Pharmacy Surrey Memorial Hospital Fraser Health Authority Surrey, BC, CanadaClinical Instructor Faculty of Pharmaceutical Sciences University of British Columbia Vancouver, BC, Canada
- *
- Correspondence to: A.C.W. Lau, BSc , Pharmacist, Surrey Memorial Hospital Pharmacy Department, Fraser Health Authority, 13750 96 Avenue, Surrey, BC, Canada V3V 1Z2. Email:
About Katherine Longardner Md
Katherine Longardner, MD, earned her medical degree at Florida State University College of Medicine. She completed her internship, neurology residency, and two-year movement disorder fellowship at University of California San Diego Health. Dr. Longardner is a board-certified neurologist and movement disorder specialist who diagnoses and treats a variety of adult movement disorders, including Parkinson’s disease, atypical parkinsonism, as well as tremor, myoclonus, dystonia, tics, and other hyperkinetic movement disorders. Her research focuses on parkinsonian non-motor symptoms, especially the relationship between orthostatic hypotension and cognition Parkinson’s disease and related disorders. She developed an interest in orthostatic hypotension when she realized that this is an under-recognized yet treatable non-motor symptom that can be debilitating. She is currently collaborating with Dr. Sheng Xu’s research team from the UCSD Dept. of Bioengineering to validate a non-invasive ultrasonic blood pressure monitor for continuous monitoring in orthostatic hypotension. Another research interest is utilizing non-invasive electrophysiological techniques to study movement disorders such as tremor.
The Effect Of The Anti
One of the initial steps required when assessing a patient who is going to receive any anti-parkinsonian medication/treatment or who needs a dose adjustment is to anticipate the potential effect on his blood pressure, as it is one of the commonly related factors to the appearance of OH .
Several actions could help to improve the detection of this complication, either by the physician or the subject. It seems reasonable to instruct the patient about OH symptoms , although many cases go unnoticed . An initial pressor response assessment could be valuable to have a simple measurement to monitor future changes, as this measurement is one of the easiest ways to appraise OH in various healthcare settings.
Many caveats should be considered prior to establishing the real influence of PD medications on OH. First, there are different diagnostic criteria for defining OH. Additionally, much evidence is based on cross-sectional analyses and other confounding effects, as disease duration or previous autonomous nervous system damage , have not always been considered.
We present the current evidence to estimate the potential role of current PD treatments on OH. The influence of other drugs, such as antidepressants, diuretics, and antihypertensives, is not reviewed here. Nevertheless, they should be considered when dealing with this complication and decreasing the dose or stopping the responsible medication might be advisable.
Also Check: What Are Off Periods In Parkinson’s
Clinical Events Related To Orthostatic Hypotension
In the group of patients without manometric orthostatic hypotension , only four reported one symptom during the standing procedure. Fifteen different clinical events occurred during the standing procedure in the 18 patients with symptomatic orthostatic hypotension. Among these, only six symptoms were significantly related to the manometric criteria chosen for orthostatic hypotension . By contrast, fainting and asthenia as well as the need for standing test abortion were not related to the presence of manometric orthostatic hypotension. This was probably due to the limited number of symptomatic patients included in this series. The frequencies for repetitive symptoms included in the questionnaire to test its internal validity were not significantly different. This indicates that patients were consistent in answering the questionnaire as patients reporting asthenia or dysequilibrium also reported unusual fainting and postural instability respectively 81.1-98.3) and 91.3% of concordance respectively). Furthermore, as hypothetised, only one patient with and one without orthostatic hypotension complained of a decrease in hearing suggesting that the questionnaire was able to discriminate events related or not related to orthostatic hypotension.
Number of patients with and without orthostatic hypotension presenting at least one symptom related to orthostatism or needing standing test abortion
What Is Neurogenic Orthostatic Hypotension
OH is a sustained fall in blood pressure that happens within 3 minutes of standing. OH can reduce blood flow to organs above the heart, most notably the brain, and its symptoms can have a profound impact on your quality of life. OH is more common in the elderly, and certain medications, dehydration, varicose veins, severe anemia and conditions such as heart disease can lead to OH. OH can also be related to the nervous system. Parkinsons, pure autonomic failure, multiple system atrophy and other types of autonomic dysfunction can all cause OH.
OH can be caused by the body not releasing enough of the neurotransmitter, norepinephrine. When your body doesnt release enough norepinephrine, your blood vessels dont constrict when they need to, lowering your blood pressure and causing you to feel faint when you stand or sit up. When OH is caused by problems in the release of norepinephrine, it is referred to as neurogenic orthostatic hypotension .
Read Also: Is Restless Leg Syndrome Related To Parkinsons
Recommended Reading: Does Parkinson’s Affect Eyesight
First Step: Make The Right Diagnosis
Given its unspecific, and sometimes asymptomatic, presentation, OH should be actively screened at bedside by measuring the BP and heart rate supine and after 3 minutes upon standing . OH is diagnosed in case of a systolic BP fall 20mmHg and/or diastolic 10mmHg with respect to baseline . Standing systolic BP values < 90mmHg are also highly suggestive of OH and often predict symptoms of orthostatic intolerance . In case of milder BP falls at the 3rd minute upon standing, it is recommendable to prolong the orthostatic challenge to 510 minutes, in order to screen for delayed OH, a possible precursor of classic OH .
Once a diagnosis of OH is established, non-neurogenic causes and exacerbating factors, such as dehydration, anemia or infections should be ruled out. The medication schedule should be also reviewed for drugs with BP lowering effect, which may have been recently introduced or increased in dose: not only anti-hypertensive agents, but also dopaminergic drugs, tricyclics, opioids, neuroleptics or -blockers.
Fig.1
Management of orthostatic hypotension and supine hypertension in Parkinsons disease. OH, orthostatic hypotension BP, blood pressure HR, heart rate NSAIDs, non-steroidal anti-inflammatory drugs SNRI, serotonin-noradrenaline reuptake inhibitors. Adapted from Fanciulli et al. 2014 and Fanciulli et al., 2016 with permission from Springer and John Wiley and Sons.
Fig.2
Phenylephrine Therapy To Treat Refractory Orthostatic Hypotension In A Patient With Parkinsons Disease
Jaekyoung A. Hong, MD, Sara E. Williford, MD, and John D. Bisognano, MD, PhD
Background
Orthostatic hypotension is characterized by abnormal decrease in systolic blood pressure greater than 20 mm Hg or diastolic BP greater than 10 mm Hg when standing from a supine or sitting position. The symptoms of OH can include syncope, lightheadedness, clamminess, palpitations, diaphoresis, anxiety, visual changes, and nausea these symptoms are resolved by sitting or lying down. Multiple factors can contribute to OH, and some of the common causes include medications such as antihypertensive and psychotropic drugs, hypovolemia, aging, deconditioning often caused by immobility leading to venous pooling, decreased vasoconstriction, and autonomic nervous system dysfunction.1,2
ANS dysregulation due to Parkinsons disease is one of the four different forms of primary autonomic failure, which include multiple system atrophy, pure autonomic failure, and dopamine beta-hydroxylase deficiency.3 In patients with PD, the prevalence of OH is estimated to be 20%.4 The high prevalence of OH in this particular population is mainly due to dopaminergic drugs worsening or inducing OH, and PD as a cause of OH involving autonomic system and decreased delivery of the neurotransmitter norepinephrine to vascular adrenoreceptors.5
Case Presentation
Also Check: Types Of Parkinsons Disease
Also Check: When Should Parkinson’s Patients Stop Driving
Morning Bradykinesia Common Device
The head-up tilt test is a passive assessment of orthostatic hypotension and does not activate the leg muscles targeted during strength training. More significant differences may have been observed if an active standing test had been used, the team suggested.
The researchers added that it was not determined whether strength training actually improved muscle strength, and a longer training period might be needed to see meaningful gains. Additional effects of co-existing health problems and other medications cannot be ruled out, they also noted.
Secondary endpoints included cognitive function, mobility, and life quality. Since no primary endpoints were met, secondary endpoints were not analyzed, the researchers noted.
Future studies should be powered to explore the effect of strength training on other parameters such as orthostatic complaints and cognitive symptoms associated with , they wrote.
General And Clinical Characteristics Of Patients
The subjects showed mild disease with 1.3 ± 1.1 years of disease duration. Twenty-two patients had comorbid disease, which could affect blood pressure. Hypertension was the most common, followed by diabetes and benign prostatic hyperplasia .
Eighteen patients showed OH and twenty-seven patients did not. Patients without OH were older and showed shorter duration of education, but those demographic characteristics were not significantly different between groups . Parkinsonian symptoms and daily activities of the patients also showed no significant difference between groups .
You May Like: What Does Parkinson’s Do To You
The Management Of Orthostatic Hypotension In Parkinsons Disease
1Department of Neurology, University Hospital 12 de Octubre,, Madrid, Spain
2Department of Medicine, Faculty of Medicine, Complutense University, Madrid, Spain
3Centro de Investigación Biomédica en Red sobre Enfermedades Neurodegenerativas, Madrid, Spain
4Instituto de Salud Carlos III, Madrid, Spain
You May Like: Parkinsons Hallucinations Commercial
Episode : Understanding Neurogenic Orthostatic Hypotension
Among the many non-motor symptoms of Parkinsons disease are blood pressure changes. One manifestation is neurogenic orthostatic hypotension, a condition in which blood pressure drops sharply when one moves from a reclining to a more upright position, such as standing up when getting out of bed or rising from a chair. The person may feel lightheaded, dizzy, lose balance, or, rarely, even lose consciousness. Besides being uncomfortable, the condition can be dangerous if it leads to a fall and subsequent injury. Orthostatic hypotension is common in mid- and late-stage PD, but it may also be an early sign of the disease.
Fortunately, there are strategies and other measures people can do for themselves to lessen the problem, and a variety of medications may help. Other conditions and medications can also lead to the condition, and they should be investigated in addition to a connection with PD. In this podcast, neurologist Dr. Katie Longardner of the University of California San Diego discusses the problem, how it is diagnosed, what people can do to alleviate it, and some of the research she and others are conducting.
Released: December 1, 2020
Don’t Miss: How Long Can A Person Live With Stage 5 Parkinson
Orthostatic Hypotension: Causes And Treatment
Do you face a blackout when you stand up after sitting or lying down? This could result from orthostatic hypotension.
It is technically low blood pressure that you face after staying put for a while.
It is also known as postural hypotension and can go beyond the blackout making you dizzy or even faint.
If your blood vessels are unable to constrict while standing up, you end up feeling the symptoms.
However, they can improve with medication and by taking an upright position.
This article discusses how you can treat this condition and reduce the symptoms that come along.
Keep reading to know.
Also Check: How Long Can I Live With Parkinsons Disease
How Is Blood Pressure Measured
Blood pressure is measured by listening to your pulse in your arm, using a stethoscope with an inflated arm cuff. Two readings are taken from each beat.
The first reading is a measure of the highest pressure when your heart pumps blood around your body . The second is a measure of the lowest pressure when your heart is resting between beats . By taking the two readings, you are getting a maximum and minimum blood pressure.
The readings are given as two numbers, both measures of pressure called mm Hg. For example, if your systolic pressure is 120mm Hg and your diastolic pressure is 70mm Hg, your blood pressure is written as 120/70. Blood pressure will vary throughout the day and from person to person but a normal blood pressure reading is generally considered to be between 90/60 and 140/90. Any readings outside of this range are classed as low or high.
Also Check: Parkinson’s Disease Muscle Cramps
Effects Of Parkinsons Disease On Blood Pressure
This short web page explains the physical operation of blood pressure in the body, symptoms of low blood pressure and when they are most likely to occur, why low blood pressure is dangerous, medical treatments and lifestyle strategies to cope with low blood pressure, and a reminder that low blood pressure can affect the ability to drive safely.
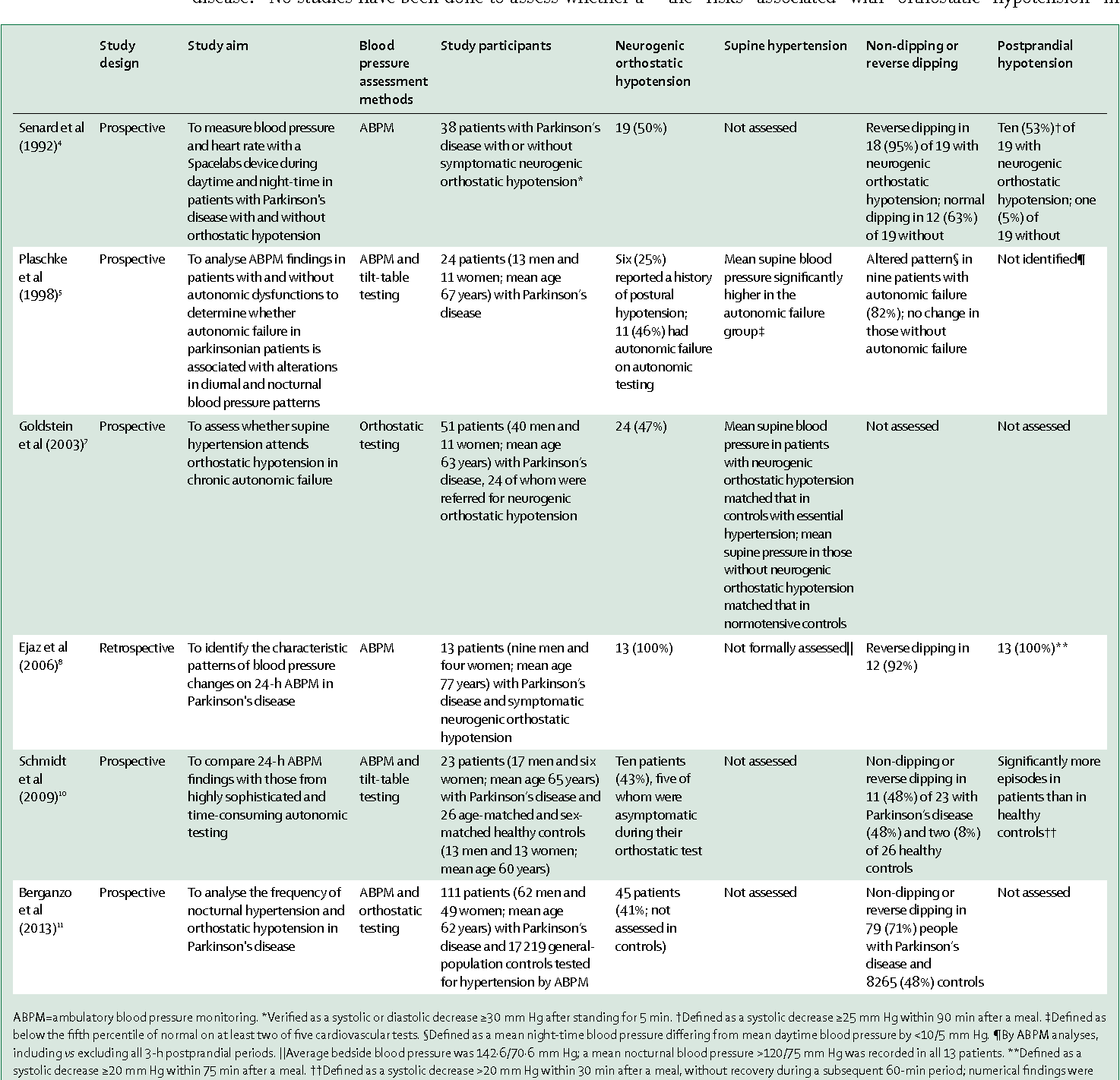
Orthostatic Hypotension In Patients With Parkinsons Disease And Atypical Parkinsonism
This article outlines a study which reviewed current evidences on epidemiology, diagnosis, treatment, and prognosis of orthostatic hypotension in patients with idiopathic Parkinsons disease and atypical parkinsonism. Conclusions include recommendation for further study of OH and routine screening for timely diagnosis and further assessments beyond the recommended 3 minute postural challenge currently used.
Read Also: On-off Phenomenon
Recommended Reading: Nyu Parkinson’s And Movement Disorders Center
Orthostatic Hypotension And Neurogenic Orthostatic Hypotension
The symptoms of nOH/OH result from inadequate perfusion of targetorgans upon standing and are similar regardless of the underlying etiology. The most frequent symptoms of thecondition include postural lightheadedness or dizziness, presyncope, and falls . Lesscommon symptoms include visual disturbances, fatigue, generalized weakness,cognitive dysfunction, neck pain or discomfort , andorthostatic dyspnea .
The prevalence of nOH in patients with PD reported in studies thatdefined nOH by BP reduction criteria ranges widely in individual studies from 10to 65% ), and ameta-analysis of 25 studies identified an estimated point prevalence of 30%. Similarly, the prevalenceestimates of symptomatic nOH in patients with PD are diverse, with reportedrates ranging from 16 to 89% in individual studies . However,not all patients who have an orthostatic BP drop meeting the criteria for nOHwill report orthostatic symptoms. Results from studies in PD populations havesuggested that a substantial portion of patients meet the BP criteria for OH butare asymptomaticthat is, they report no symptoms typical of cerebralhypoperfusion .
Low Blood Pressure In Parkinsons Disease
This 2-page article discusses the frequency of orthostatic hypotension in those with PD, the cause, symptoms and several simple measures that can be used to restore normal blood pressure regulation, including medication evaluation, increase of fluids and salty foods, caffeine, frequent small meals, environment, clothing, slow position change, bed position and medication options.
Also Check: How Do Neurologists Treat Parkinson’s
Continuous Dopaminergic Stimulation Therapies
Deep brain stimulation
Cross-sectional studies have suggested a positive effect of subthalamic Deep Brain Stimulation on autonomous responses of PD subjects . In one of this analysis, including 14 patients, there was a mean general decrease on blood pressure in on and off stimulation status ,1), but the baroreflex responses were preserved only when the stimulation was on, suggesting, therefore, a positive influence of the DBS in BP mediated by its influence on central autonomous nervous system pathways . In another study comparing subthalamic DBS with a pharmacotherapy-only group, no positive correlation was found between the on-stimulation state and the decrease in blood pressure but this occurred in the only medicated group. Based on this finding it was suggested that subthalamic DBS did not affect cardiovascular autonomous responses . Noteworthy, in a previous longitudinal study, the initial differences of blood pressure were not found after 1years follow-up, with a similar mean blood-pressure decrease for the subthalamic DBS and the only medicated groups . Additionally, two other studies could not find differences in the cardiovascular responses of the treated subjects .
Apomorphine pump/apomorphine injections
Manage Neurogenic Orthostatic Hypotension
Neurogenic orthostatic hypotension is a condition that is part of a larger category called orthostatic hypotension , which is also known as postural hypotension. nOH is caused by dysfunction in the autonomic nervous system and causes people to feel faint when they stand or sit up. Learn more about nOH in the first part of our article.
The good news is that there is treatment for neurogenic orthostatic hypotension. The goal of treatment is not to achieve normal blood pressure values, but rather, to reduce symptoms of nOH and improve your quality of life.
Read Also: How To Use Melatonin With Parkinson’s
Low Blood Pressure In Parkinson’s Disease
This 2-page article discusses the frequency of orthostatic hypotension in those with PD, the cause, symptoms and several simple measures that can be used to restore normal blood pressure regulation, including medication evaluation, increase of fluids and salty foods, caffeine, frequent small meals, environment, clothing, slow position change, bed position and medication options.
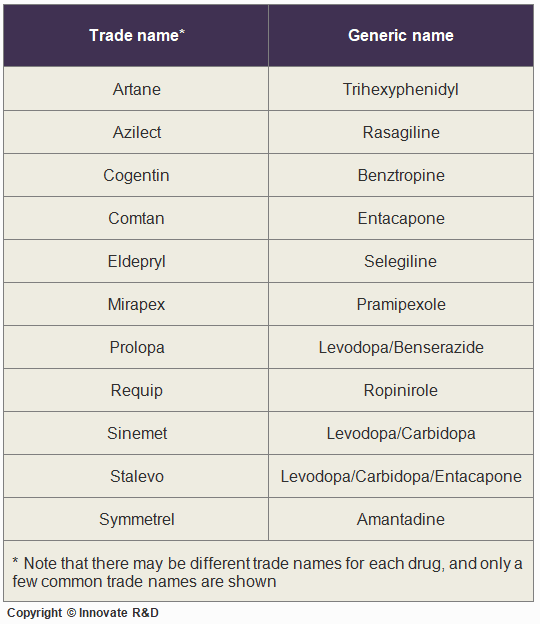
How Is Orthostatic Hypotension Treated
Droxidopa . fludrocortisone , or midodrine capsules are approved for the treatment of orthostatic hypotension. Common side effects include headache, dizziness, nausea, high blood pressure, and fatigue.
Another approach in treating orthostatic hypotension is to decrease the pooling of blood in the legs with the use of special stockings called compression stockings. These tight stockings compress the veins in the legs, helping to reduce swelling and increase blood flow. There are a number of companies that make these stockings in a wide variety of sizes, and they usually can be found at stores that sell medical supplies, as well as at some pharmacies.
You should wear these stockings when you are up and about. You do not need to wear them when you are in bed. Further, it is recommended that you put the stockings on first thing in the morning while in bed and before getting up for your daily activities. It is important that you do not let the stockings bunch, gather, or roll, since this can compress the veins too much and could harm circulation. You should always watch for signs of decreased circulation, which could include discoloration of the skin, as well as pain or cramping, and numbness of the lower legs and feet.
Show Sources
Also Check: Weighted Silverware
Don’t Miss: Does Parkinson’s Cause Low Blood Pressure
