A Special Suit That Helps Patients With Parkinsons
Exopulse Mollii can improve mobility in people with brain or Parkinsons disease. The suit is equipped with 58 built-in electrodes, which are adapted by a technician to the individual needs of the user. Low-frequency electrical stimulation improves blood circulation and restores previously disturbed balance between muscle pairs. If for example the biceps are tense, the suit stimulates the triceps muscles, which in turn cause the biceps to relax.
Who Is The Best Candidate For Dbs Surgery
The best candidate for DBS surgery is someone:
- Who has had a Parkinson’s diagnosis for at least four years
- Who benefits from Parkinsons medication but has motor complications such as significant “off periods when motor symptoms return because the medication is not effective
- Who has motor fluctuations and/or dyskinesias or refractory tremors that are not adequately controlled with PD medications
- Who has minimal PD symptoms like instability, gait difficulties, and speech problems during the on periods, indicating an excellent response to levodopa
- Who has normal or minimally affected cognitive, psychiatric, and behavioral functions
- Who has no serious medical comorbidities.
It is worth noting that most patients who undergo DBS surgery have Parkinson’s disease onset at a relatively young age and are less than 70 years of age at the time of the procedure. However, the ultimate decision about patient management is based on each individuals medical history and disease progression.
The key to the success of deep brain stimulation is the proper selection of ideal patients for this procedure. The selection of patients for deep brain stimulation is based on a detailed evaluation by a team of multidisciplinary experts in neurological disorders, including a movement disorders neurologist, neuropsychologist, psychiatrist, and neurosurgeon.
Discover Other Projects Like Exopulse
Since 2015, Maker Faire Rome has been running a contest dedicated to advanced tech-enabled healthcare solution: Make to Care.
Make to Care is promoted by Sanofi Genzyme, Specialty Care division of Sanofi. Sanofi Genzyme is specifically providing solutions for rare diseases, multiple sclerosis, oncology and immunology. MaketoCare wants to celebrate and support initiatives and projects arising from the cleverness and passion of the Maker community.
Make to Care is aimed at bringing out and facilitating the creation and growth of innovative and useful solutions to meet the real needs of people with any form of disability, meant as any marked decrease in quality of life due to pathologies and / or traumatic events.
The participation to the contest is open to all those who have been able to grasp a concrete need, directing their talent and proposing an innovative solution.
Maker Faire Rome The European Edition has been committed since eight editions to make innovation accessible and usable to all, with the aim of not leaving anyone behind. Its blog is always updated and full of opportunities and inspiration for makers, makers, startups, SMEs and all the curious ones who wish to enrich their knowledge and expand their business, in Italy and abroad.
Follow us, subscribe to our newsletter: we promise to let just the right content for you to reach your inbox
Dont Miss: What Age Is Parkinsons Disease Diagnosed
Don’t Miss: Can Stress Cause Parkinson’s Disease
Evaluation Of The Application Of The Exopulse Mollii Method Every Second Day
The analysis of the potential fluctuations in spasticity over time did not show any statistically significant difference in NC and NeuroFlexor total resistance before stimulation between day 1, 2, and 3, neither in the upper or lower extremity. These results suggest stable spasticity over days and the lack of any carry-over effect of EXOPULSE Mollii stimulation between time points, a prerequisite for the study of changes in spasticity during and after each session of treatment. These results are in agreement with the short-lasting duration of the effects of a standardized application of EXOPULSE Mollii of up to 48 h, as stated by the company and similarly to the transitory effects of TENS .
Outlook For Closed Loop Transcranial Electrical Stimulation
Although closed-loop tES studies toward PD are few, adaptive stimulation schemes have gained vast attention since they can deliver individual- or circumstance-specific modulation. Self-adaptive individualized closed-loop scheme can achieve higher efficacy and closed-loop tES schemes in the future might also be able to automatically switch on when symptoms occur, like closed-loop DBS.
Another serious technical problem for closed loop tES is the time delay between detection of changes in brain conditions and the response to stimulus. For symptoms with a short provoking duration, the time delay in response might just miss the period of symptoms and become ineffective. Future studies might employ machine learning to predict the occurrence of symptoms so that more precise stimulation could be provided. In addition, using a brain machine interface can provide a quicker stimulation response. For example, in a chronic pain study that used BMI in mice to monitor and stimulate the brain, the time delay between characteristics detected and stimulation response was minimized thus, the pain could be released even when recognizing acute pain signals .
Many studies have proposed numerous novel adaptive tACS and tDCS systems that proved to be safe and tolerable in healthy people . Building on these results, investigators could adopt those technologies in future closed loop tES studies in clinical PD populations.
Recommended Reading: What’s Parkinson’s Disease
When Should I See My Healthcare Provider
Your healthcare provider will schedule visits to see you after your procedures. Programming visits occur with your neurologist, and youll need to make appointments to see them. The goal of those visits is to find the settings that work best and don’t cause side effects that disrupt your life.
Regular visits with your healthcare provider are also common to monitor your condition, symptoms and to adjust medications or other treatments as needed. The schedule for these visits is something that your provider will discuss with you.
Will Insurance Cover Wearable Devices For Parkinsons Tremor
Most devices mentioned in this post are unfortunately not covered by insurance. These devices typically will cost in the hundreds of dollars out of pocket. Some of the manufacturers will offer financial assistance and/or payment plans.
Many manufacturers will allow you to try out their devices and return them for a refund if you are not satisfied with the results.
Read Also: What Effect Does R Dopa Have On Parkinson’s Disease
See The Difference Sixty Minutes Can Make*
Designed to be worn just an hour every other day, the Suit provides an easy, on-demand way to restore mobility and relieve spasticity-related pain. For users like Louisa, Max, and David, that hour makes all the difference in their day.
Just an hour of near full-body stimulation improves her balance, gait, and stability, and helps make everyday tasks easier for her.
Wearing the Suit helps keep him safer and more stable and gives him the control and confidence he needs when walking.
After an hour in his Suit, Davids hand, arm, and leg movements are already easier and more coordinated.
Special Suit Shows How Parkinsons Disease Feels
If you read about Parkinsons disease , you will quickly hear about typical symptom such as muscle stiffness and tremor. But how does that feel?
For a healthy person it is very difficult to imagine who it feels to have PD. Dr Roland Schöffel from SD& C has therefore built the Parkinsons Suit, with which one can simulate PD. The NCER-PD Team has tested the suit at the Annual Conference 2015 of the young patient organisation in Saarlouis, Germany.
At first sight the suits resembles a racing outfit. A young man helps interested people into the red overall. But after the comfortable suit follows quickly the mobility-restricting measures: cuffs on knees and elbows hinder the flexion of these joints. Next follow heavy weights on arms, legs and trunk. The SD& C employee loads a total of 10 kilos onto the participants body and explains that the cuffs and weights should simulate how heavy and inflexible the muscles of patients can feel. The suit focuses only on the motor symptoms and simulates an average person as the severity and type of symptoms can vary from patient to patient. In the practical test, NCER-PD employee Dr Sabine Mosch is clearly walking slower. She clearly has a hard time pursuing movements that require lifting of arms or legs.
Deprecated/var/www/html/joomla/modules/mod_sp_simple_gallery/helper.php38
Read Also: Famous Actors With Parkinson’s
What Happens After Deep Brain Stimulation
Your healthcare provider will schedule a follow-up appointment that will take place within a few weeks of the pulse generator implantation procedure. At this appointment, they’ll start programming the pulse generator.
All pulse generators now in use have a wireless antenna built-in. That allows your healthcare provider to access and program the device from outside your body. Finding the right settings for the pulse generator may take some time and additional visits for adjustments.
Most pulse generators have special batteries that have long lifespans. Standard batteries for these devices last about three to five years. Some devices use rechargeable batteries, which can last about nine years. Replacing the battery also takes a surgery procedure, but this is usually shorter and quicker than the original surgery to implant the pulse generator. You’ll still go home the same day for battery replacements.
How Can An Electrode Suit Treat Nerve Disorders
More than 5 million Americans suffer traumatic brain injury and its side effects every year side effects that often include neuromuscular problems. More than 760,000 additional Americans are affected by a neuromuscular condition caused by stroke or spinal cord injury every year. And when you add in the number of people living with cerebral palsy and Parkinsons disease the numbers just keep climbing its estimated that movement disorders affect about one out of seven Americans .
Movement disorders are characterized by a problem with you guessed it movement. These conditions impair voluntary and involuntary muscle movements, which translates into problems with things you may take for granted, such as walking and speech. In addition, they may also cause pain, jerky movements and abnormal postures and conditions that impair people in this way can make living our daily lives difficult.
Treatments often include physical, occupational and other rehabilitative therapies, pharmacotherapy including immunosuppressive drugs, chemodenervation and neurolysis , and sometimes neurosurgery and other therapeutic options. Sometimes patients are treated with electrical stimulation therapy techniques.
EMS works because your body is electric this type of electrical pulse stands in for how the bodys central nervous system would act if it were properly functioning.
Read Also: Treating Hallucinations In Parkinsons Disease
Read Also: Does Parkinson’s Kill You
Why A Doctor May Choose Deep Brain Stimulation
According to the National Parkinson Foundation, the ideal Parkinsons disease candidate for DBS surgery has:
-
PD symptoms that interfere with activities of daily living.
-
Fluctuations in mobility due to PD medications with or without dyskinesia .
-
Continued good response to PD medications, even if the medication effects may wear off sooner than they have in the past.
-
A history of several different combinations of PD medications while under the supervision of a neurologist specializing in movement disorders.
These factors* may make a person a less than ideal candidate for DBS surgery:
-
Difficulty with balance, walking, or freezing as the main disabling symptom.
-
A primary symptom of speech difficulty.
-
Continuous confusion and problems with memory and thinking.
-
A psychiatric condition such as depression or anxiety that has not improved or stabilized with other treatment.
-
Another condition that increases the risk for surgery complications.
*Some of these factors may be treatable. Having one or more does not disqualify a person for future DBS surgery, but the doctor may recommend more aggressive therapy focused on these issues before surgery takes place.
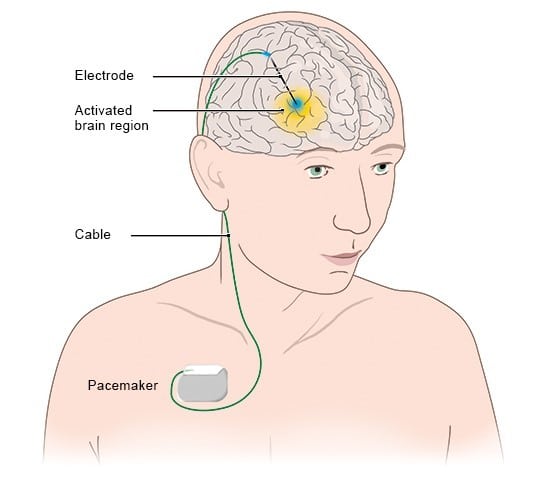
Like A Pacemaker For The Brain
Deep brain stimulation is a surgical treatment sometimes used in Parkinsons and other conditions. In this treatment, small pulses of electrical current are applied to specific locations in the brain through implanted electrodes. These electrodes are connected by wires that run under the skin to a programmable internal pulse generator, which is usually implanted just under the collarbone . It contains a battery and some electronics to generate the pulses, similar to a heart pacemaker. The device delivers electrical stimulation to specific brain areas that are involved in movement control. Electrical stimulation at precise locations in the brain is thought to restore the balance of the circuits that are disrupted in Parkinsons disease.
DBS can alleviate tremor, reduce stiffness, and lessen dyskinesias. It can very effectively smooth out on/off fluctuations.
Prior to the introduction of DBS in the 1990s, the main surgical treatment for Parkinsons disease involved inserting a probe into the brain and heating the tip of the probe to burn a very small region of brain tissue. The burn, known as a lesion, was made at the same targets that we now stimulate. Lesional surgery is still a useful option in some cases where DBS is not possible. Recently it has become possible to create lesions noninvasively using focused ultrasound.
Also Check: Parkinsons Disease And Eating Problems
Also Check: Can Parkinson’s Cause Pain
Watch How The Suit Puts Lives Back In Motion*
With a simple, non-invasive, drug-free way to manage their spasticity, Louisa and Michele are rediscovering lifes possibilities. See how the Suit turns the bodys natural signals into bodies that move more freely.
Its like I can breathe again.
With the help of her Exopulse Mollii Suit Louisa was finally able to break free from her MS-related spasticity symptoms. Her new superpower: Feeling like everythings possible again.
Conflict Of Interest Statement
UCSF has submitted two pending/provisional patents related to use of particular brain signals for closed loop DBS. Drs. NS and CH are included as co-inventors on these patents.
References
Little, S., Brown, P. 2014. The functional role of beta oscillations in Parkinsons disease. Parkinsonism Relat. Disord. 20:S44S48. doi:10.1016/S1353-802070013-0
de Hemptinne, C., Swann, N. C., Ostrem, J. L., Ryapolova-Webb, E. S., San Luciano, M., Galifianakis, N. B., et al. 2015. Therapeutic deep brain stimulation reduces cortical phase-amplitude coupling in Parkinsons disease. Nat Neurosci. 18:779786. doi:10.1038/nn.3997
Little, S., Pogosyan, A., Neal, S., Zavala, B., Zrinzo, L., Hariz, M., et al. 2013. Adaptive deep brain stimulation in advanced Parkinson disease. Ann. Neurol. 74:449457. doi:10.1002/ana.23951
Read Also: Does Aspartame Cause Parkinson’s
What Is Deep Brain Stimulation How Does It Work
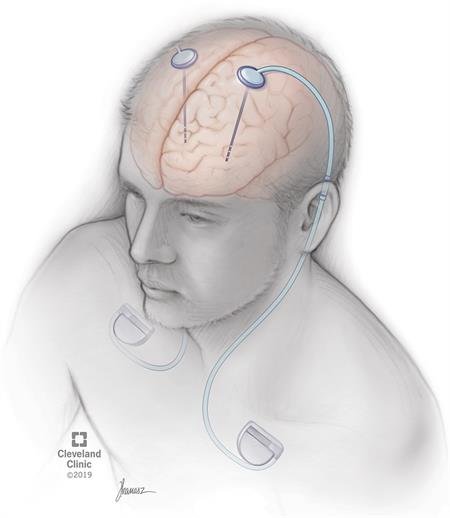
Deep brain stimulation is a surgical procedure that involves the placement of electrodes in certain areas of the brain, such as the subthalamic nucleus or basal ganglia. The electrode placement is done by a surgeon. It helps to deliver electrical stimulation in the form of bilateral deep brain stimulation.
The amount of stimulation the DBS electrodes provide is controlled by a cardiac pacemaker-like device placed in the upper chest. The DBS system also includes an extension wire or wires connecting the implant device in the chest to the DBS lead or electrodes in the brain.
As mentioned above, abnormal electrical impulses from nerve cells cause severe motor fluctuations in Parkinsons patients. DBS electrodes deliver continuous electrical pulses to regulate these abnormal electrical signals generated by the brain cells, thus providing relief from motor symptoms to Parkinsons patients.
Living With A Stimulator
Once the DBS has been programmed, you are sent home with instructions for adjusting your own stimulation. The handheld controller allows you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most patients keep their DBS system turned on 24 hours day and night. Some patients with essential tremor can use it during the day and turn off the system before bedtime. Your doctor may alter the settings on follow-up visits if necessary.
If your DBS has a rechargeable battery, you will need to use a charging unit. On average charging time is 1 to 2 hours per week. You will have a choice of either a primary cell battery or a rechargeable unit and you should discuss this with you surgeon prior to surgery.
Just like a cardiac pacemaker, other devices such as cellular phones, pagers, microwaves, security doors, and anti theft sensors will not affect your stimulator. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates.
Don’t Miss: Is There A Medical Test For Parkinson’s
What Is Deep Brain Stimulation For Parkinsons Disease
Deep brain stimulation is a surgical procedure used to treat a variety of disabling neurological symptomsmost commonly the debilitating symptoms of Parkinsons disease , such as tremor, rigidity, stiffness, slowed movement, and walking problems. The procedure is also used to treat essential tremor, a common neurological movement disorder. At present, the procedure is used only for patients whose symptoms cannot be adequately controlled with medications.
DBS uses a surgically implanted, battery-operated medical device called a neurostimulatorsimilar to a heart pacemaker and approximately the size of a stopwatchto deliver electrical stimulation to targeted areas in the brain that control movement, blocking the abnormal nerve signals that cause tremor and PD symptoms.Before the procedure, a neurosurgeon uses magnetic resonance imaging or computed tomography scanning to identify and locate the exact target within the brain where electrical nerve signals generate the PD symptoms.
Some surgeons may use microelectrode recordingwhich involves a small wire that monitors the activity of nerve cells in the target areato more specifically identify the precise brain target that will be stimulated. Generally, these targets are the thalamus, subthalamic nucleus, and globus pallidus.The DBS system consists of three components: the lead, the extension, and the neurostimulator.
Deep Brain Stimulation Surgery And Implantation
DBS consists of two surgeries, spaced approximately three to six weeks apart to ensure the patient has adequate time to recover. Throughout your experience, you will be attended to by a top team of physicians and other medical experts including a neurosurgeon, an electrophysiologist, and an anesthesiologist.
It should be noted that DBS offers many benefits. The generator can be programmed by a neurologist, and customized to each individual patient. The procedure is also reversible. Most patients experience a significant improvement of symptoms. However, as with any brain surgery, there are risks. With DBS, the risk of stroke is 1 in 100 and infection is 1 in 50.
Today, many more patients could be helped by DBS than are currently benefiting from the procedure. Statistics show only 7 percent of Parkinsons disease and 1 percent of tremor patients in Michigan who would benefit from the procedure have undergone DBS. At U-M, we are proud to have one of the superior DBS programs in the country. We have developed a wide array of ways to improve DBS, including special imaging tools that help doctors more accurately place the electrodes, and lead intraoperative motor and speech testing that result in fewer side effects for the patient.
U-M is also home to an active research program, where our team of experts is always working on ways to make DBS faster and more accurate. We also regularly have clinical trials available for patients interested in participating.
You May Like: What Are The Final Stages Of Parkinson’s Disease
