My Parkinson’s Story: Pain
This 10-minute video alternates between an interview with a man and and doctors. The man shares his experience with pain as a symptom of Parkinson’s disease. The doctors explain that pain is common in Parkinson’s disease, often due to rigidity or dystonia, which can be exacerbated by “off” periods. Pain caused by Parkinson’s symptoms can be relieved by Parkinson’s medications, exercise, DBS and botox injections. Pain is an invisible symptom that should be mentioned to your neurologist.
Pain Is An Unfortunately Common Problem In Parkinsons Disease
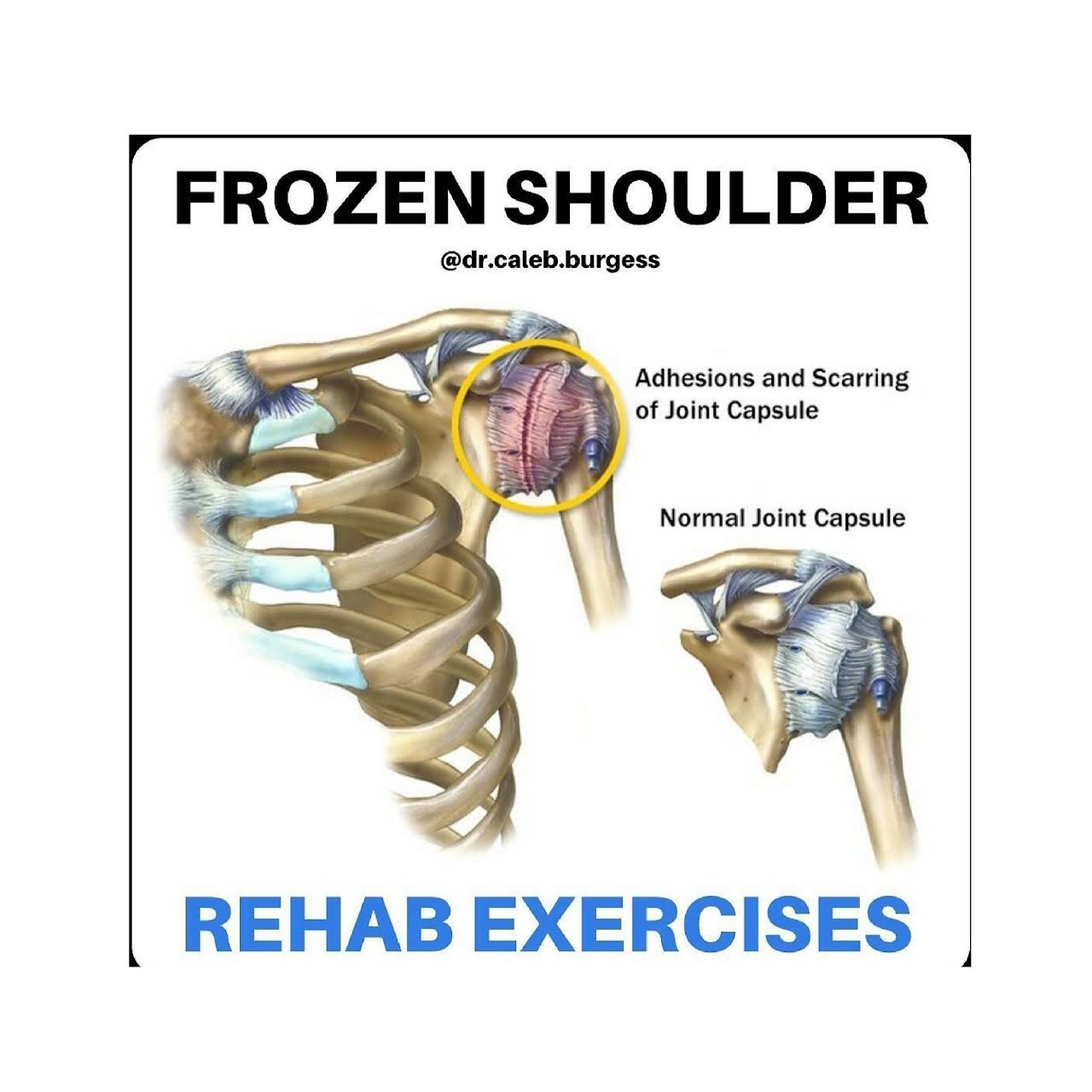
Of course, pain is common in the general population, especially among older people. A recent American study found that pain affected about twice as many people with Parkinsons Disease than those of the same age and gender without PD. About 50% of Parkinsons Disease patients in that study suffered from painful disorders. Men and women seem to be about equally affected. A very well described scenario is the patient who is followed for a painful frozen shoulder for a year or so before a tremor develops leading to a diagnosis of PD. Pain clearly plays a major role in quality of life. Everyone with chronic pain enjoys life less, leading to a vicious cycle in which pain causes depression or isolation which in turn leads to more pain.
Parkinson patients suffer from the same pain problems that other people have, often amplified by the motor dysfunction, but they also have additional pain problems which are unique to PD.
One recent review classified the types of pain Parkinsons Disease patients have into: musculoskeletal, in which the pain results from problems with the muscles , bones or joints dystonic, which is due to abnormal muscle contractions caused by the Parkinsons Disease or the medications used to treat it radicular pain, which is feels like the pain caused by pinched nerves central pain, which is presumed due to abnormalities in the brain, and is a continuously present pain that cannot be explained otherwise and discomfort related to an unpleasant urge to move.
> > > Best Joint Pain Treatment Available
Osteoarthritis affects the entire joint and causes inflammation and changes in the bone and connective tissues. Symptoms vary according to the severity of the condition. If you have this disorder, you might be experiencing pain in any joint. Its common to experience symptoms in the knee and hips. You may also develop bone spurs around the affected joint. Its important to consult with your doctor if you have these symptoms.
Symptoms of osteoarthritis include swelling and bone spurs around the affected joint. You may also experience soft tissue inflammation around the joint. Your doctor may prescribe pain relievers and suggest a program of physical activity. For those with severe osteoarthritis, surgery may be the best option. The best course of treatment depends on the severity of the condition and the symptoms youre experiencing. Ultimately, the best way to manage your osteoarthritis symptoms is to find a solution that works for you. Joint And Muscle Pain With ParkinsonS
Although osteoarthritis affects the entire joint, it tends to be more common in older people. It also affects women, who are more prone to developing this condition. Being overweight increases the risk of getting osteoarthritis, as fat tissue produces proteins that trigger inflammation. Therefore, obesity can increase the chances of developing this condition. This is because the underlying cause of this condition is genetics. It can result in certain bone deformities, including osteoarthritis.
Don’t Miss: What Is The Latest Treatment For Parkinson’s Disease
Other Symptoms: Aging Or Pd
Because the biggest risk factor for developing PD is age , skeletal problems associated with aging are often experienced by people with PD. While it is not clear that PD increases the risk or even the severity of these other skeletal conditions, the problems of PD can make the symptoms of these conditions more prominent.
- Osteoarthritis, the joint damage associated with general wear and tear on the joints, is nearly universal in aging. Osteoarthritis tends to affect larger joints such as the hip and knee.
- Arthritis of the spine is also very common. This may contribute to the development of spinal stenosis, narrowing of the canal in the spine that houses the spinal cord. In severe cases, spinal stenosis causes damage to the nerves as they exit the spine or even to the spinal cord itself.
- Disorders of the fibrous discs between the bones of the spine can also cause pain, or limb numbness or weakness.
Since A Back Injury In 1985 John Has Experienced Multiple Types Of Pain Some Of Which Have Been Triggered By His Parkinson’s He Was Diagnosed With The Condition In 2016
Ive been experiencing varying degrees of pain since injuring my back, which caused me to have lower-back pain, which continues to this day. Since then, I have also developed pain in other parts of my body due to Parkinsons, including my hands, ribs, upper back and shoulder.
The pain in my ribs is deep, aching and constant, and I get internal tremors in this area. However, the pains in my legs are sharp, intermittent and become very rigid, especially in my calves.
When I walk, the pain can get so bad that I end up having to stop and rest. On really bad days, I use a wheelchair. When Im in a lot of pain, it affects my Parkinsons symptoms even more, and also my spatial awareness, that I tend to lose my balance and fall or freeze.
I was referred to a pain specialist…who enrolled me on an 8-week pain management course led by a Parkinson’s-trained physiotherapist. Now I do an hour of gentle movements and stretching every morning.
I cant stand for long enough to wash and have a shave, or to wash the dishes, so I use a perching stool. I can no longer carry out my hobby of canoeing to the same degree. While I use to be able to do it all day, I’m now lucky if I can do it for an hour.
I was referred to a pain specialist, who prescribed me medication, and advised on workable changes to my lifestyle and diet. They also enrolled me on an 8-week pain management course led by a Parkinson’s-trained physiotherapist. Now I do an hour of gentle movements and stretching every morning.
Read Also: When Is Parkinson’s Awareness Month
Fluctuations Of Pain Experiences In Pd
Patterns of NMS fluctuations are heterogeneous and complex. Psychic NMS seem to fluctuate more frequently and severely than nonpsychic symptoms. A recent study of ten frequent NMS in advanced PD using VAS rating scales in motor-defined on- and off-states, as well as self-ratings at home, confirmed previous suspicions that increased pain in off-states and pain fluctuations correlate with a low health-related quality of life. Pain as NMS was more frequent in the off-state more precisely, it was three to four times more common during the off-state than during the on-state.
Hand And Finger Stimulation Exercises
I have done a lot of hand/finger stimulation and experimented to optimize such exercises, in the spirit of Curiosity and Play. I’ve personally found significant benefit in pursuing this line of research. Indeed, I have managed to recover a lot of my independence and quality of life through hand and finger therapy, and I know just how much of a major part it has played in my own progressive symptom reduction.
I therefore encourage everyone with PD to do as much hand and finger stimulation as possible, through games and play and self-discovery. By doing nothing, the only thing that will happen is that out situation will rapidly become worse, because we will lose the use of our hands quicker and consign ourselves to increased suffering. By applying neuroplasticity techniques , we can delay the worse ravishes of the disease or even, like in my own case, continuously push the symptoms back and recover some independence. I feel this is an important message for those newly diagnosed, in particular.
Here are some suggestions of the type of stimulatory exercises and games which can help, more ideas which I have personally found beneficial will be provided in forthcoming articles.
You May Like: Parkinson’s Association Of The Rockies
Variables Associated With Msp
Figure 2 shows the results of the logistic regression analysis of variables identified as potential risk factors of MSP. The candidate variables entered into the logistic regression model were female sex, PD durations, MDS-UPRDS I, and LEDDs. As the MDS-UPRDS I includes a pain-related item , we exclude this item from MDS-UPDRS I score and analyze it without this item. The variables that achieved statistical significance as associated factors of MSP were female sex and LEDDs . PD duration, MDS-UPDRS part III score in the OFF state and MDS-UPDRS part IV, PDSS , HAMD , and HAMA scores were not significantly associated with MSP.
Figure 2. Risk Factors associated with MSP in patients with Parkinson’s disease by binary logistic regression analysis. MSP, musculoskeletal pain PD, Parkinson’s disease OR, odds ratio CI, confidence interval LEDD, Levodopa-equivalent daily dose.
Pain Sites And Assessments
All patients were asked to indicate the distribution of pain sites, duration of pain, and rate average pain intensity over the past 3 months on an 11-point numeric rating scale , with 0 indicating the absence of pain and ten indicating the most intense pain imaginable. The patients reported NRS scores in both the ON and OFF states of motor function on the same day. NRS scores were then transformed into WHO severity stages of mild , moderate , and severe , respectively . MSP responsiveness to Levodopa was defined as a 30% reduction in NRS scores from baseline, 2 h after taking the medication . Data regarding multiple types of pain were also recorded. The ID-pain scale detected central parkinsonian pain.
Don’t Miss: What Causes Parkinson’s Symptoms
What Does Parkinsons Rigidity Feel Like
Rigidity, while seldom the main symptom early in Parkinsons, is experienced as a stiffness of the arms or legs beyond what would result from normal aging or arthritis. Some people call it tightness in their limbs. Stiffness can occur on one or both sides of the body and contribute to a decreased range of motion.
Not Your Usual Neck And Back Pain
There are many ways to get a backache. This is new for me lower back pain that leads to spasms and literally drives me to my knees.
It doesnt feel like the pain from overdoing it in the garden. Every gardener knows that exquisite twinge from too much lifting or shoveling. After all the years I have gardened, I know that pain well. This is not my usual lower back pain.
An article published in 2018 in the European Spine Journal found significantly more cases of low back pain, with longer durations, in patients with Parkinsons disease than in healthy controls. Parkinsons patients also experience more frequent and intense lumbar pain. Researchers concluded that Parkinsons progression can lead to degeneration of the lumbar spine, and this leads to low back pain for about 88% of this population.
Also Check: Why Is It Important To Take Parkinsons Medication On Time
You May Like: What Are The Non Motor Symptoms Of Parkinson’s Disease
Multiple Regression Analysis Of Qol Improvements
Multivariate regression analysis was used to adjust for confounding factors between the two groups, and absolute changes in QOL were taken as results . Preoperative EQ-5D and PD were important independent predictors of EQ-5D changes. After adjusting for confounding demographic, comorbid, and unilateral or bilateral TKA, PD predicted a decrease in EQ-5D improvement at the LFU .
Table 3 Multiple regression model for improvement of QOL
The data confirmed that PD was not an important independent predictor of changes in PDQ, while preoperative PDQ and unilateral or bilateral TKA were proved to be important independent predictors of changes in PDQ. Bilateral TKA indicated a decrease in postoperative PDQ improvement. Similarly, PD was not a significant independent predictor of changes in PHQ-9. Multivariate regression analysis found that prior depression and anxiety and longer preoperative duration of symptoms were predictors of diminished improvement in PHQ-9.
Q Are There Any Alternative Therapies That Are Effective For Pain In Pd
Dr. Fleisher: Although alternative therapies may be helpful, there is little evidence-based research to support their use. Certainly massage therapy, anecdotally, seems to be helpful for managing pain. Small studies suggest that acupuncture might improve sleep in patients with PD, but data on the effects on pain in PD is lacking. Larger, more well-controlled and reproducible studies of these therapies are needed.
Patients frequently ask about the effects of medical marijuana in managing PD, including pain symptoms. Several studies have looked at efficacy of marijuana in PD and have found that it probably is ineffective for most PD symptoms.11 However, we just dont have enough evidence to know for sure. The most rigorous study of medical marijuana in PD showed a trend toward worsening tremor.11,12
For most people, stress and anxiety worsen tremor, and anything that relieves anxiety will improve tremor. Thus, modalities such as yoga, meditation, and mindfulness training will improve tremor. Similarly, medical marijuana may improve tremor in certain people by temporarily reducing anxiety and stress, but the evidence has not borne this out yet.
Don’t Miss: How Is Parkinson’s Caused
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Dont Miss: Plan Of Care For Parkinsons Disease
How To Exercise With Parkinsons
Whether youre a first-time exerciser or a lifelong athlete, the key to working out with Parkinsons is to safely and regularly move your body in a variety of ways. Your fitness regimen should include these four main categories of exercise:
- Aerobic activity
- Balance, agility, and multi-task exercises
People with Parkinsons should strive to perform aerobic activity at least three times weekly and to complete exercises from the other categories two to three times each week.
In total, the Parkinsons Foundation suggests performing 150 minutes of moderate tovigorous exercise weekly.
To help you achieve this goal, try these helpful tips:
- Invest in a treadmill, elliptical, or exercise bike. This will make it convenient to perform aerobic exercise from your home, regardless of the weather.
- Obtain a set of light hand weights from a local exercise shop or thrift store. These can be used for a wide variety of strength training exercises.
- Follow along with one of the many online exercise classes on YouTube that are tailored to people with Parkinsons disease. The Parkinsons Foundation and the Davis Phinney Foundation offer many great online exercise videos.
- Connect with a workout buddy by finding a local Parkinsons support group associated with the American Parkinson Disease Association
Read Also: Parkinsons Hallucinations Commercial
Read Also: How Early Can Parkinson’s Disease Be Detected
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsons. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Opening The Medicine Box In The Mind: The Psychology Of Pain
In this 50-minute lecture, Beth Darnall, PhD explains how our experience of pain goes beyond the physical sensation of pain. It has emotional and psychological components that affect our ability to treat pain. She cites research to demonstrate that and shares 13 specific tips to reduce the experience of pain and increase treatment effectiveness. Audience questions follow the lecture.
Don’t Miss: What Does Parkinson’s Disease
If You Experience Stiffness In Your Shoulder It May Be Due To Parkinsons
While those with Parkinsons may experience stiffness in several body parts, experts say that having frozen shoulder, also known as adhesive capsulitis or periarthritis, is particularly linked with PD. Shoulder stiffness is, in fact, one of the conditions associated with Parkinsons disease, a neurodegenerative disorder caused by a lack of dopamine in the brain, explains Very Well Health.
When a patient develops frozen shoulder, the connective tissues that encase the bones, ligaments, and tendons in that area thicken and tighten around the shoulder joint. When this happens, movement becomes restricted, causing pain and stiffness.
According to the Mayo Clinic, symptoms of frozen shouldertypically begin gradually, worsen over time and then resolve, usually within one to three years. The health authority says this often occurs in three distinct stages: the freezing stage, the frozen stage, and the thawing stage. In the freezing stage, the patient typically experiences reduced range of motion along with joint pain in one shoulder. The frozen stage is typically less painful, but as the shoulder becomes stiffer, many people lose most or all function in the affected shoulder. In the thawing stage, the patient begins to regain range of motion.
Dont Miss: Diseases Similar To Parkinsons
