What Is Lewy Body Dementia And Why Is It So Hard To Diagnose
TW: This article contains mention of suicide. Please proceed thoughtfully.
Today marks the eighth anniversary of Robin Williamss death. The legendary comedian and actor committed suicide in 2014 at age 63. Williams suffered from depression and was misdiagnosed with Parkinsons disease, which played a role in the frustration and discomfort Williams experienced in life, according to his son Zak Williams who spoke last year on The Genius Life podcast about the misdiagnosis. It was later discovered after the comedians death that he actually had Lewy body dementia.
The brain disease impacted Williams thinking, memory, and movement control which got in the way of both his career and family life, his son said on the podcast. There was a focus issue that frustrated him, there were issues associated with how he felt and also from a neurological perspective he didnt feel great, he says.
Dad, on the eighth anniversary of your passing, Im remembering how incredibly kind and joyful you were. I deeply miss you you wonderful, hairy man and will be celebrating your life today. Love you so so much!
â Zak Williams
What he was going through didnt match one to one many Parkinsons patients experience, Zak said. So, I think that was hard for him.
So why was Williams misdiagnosed? According to experts, there are many similarities between Parkinsons disease and Lewy body dementia. Keep reading to learn more about Lewy body dementia, including causes, symptoms, and treatment.
How Is Lewy Body Dementia Different From Alzheimers
Alzheimers disease is the most common type of dementia, and LBD is the second most common. Because of the overlap in symptoms, it can be difficult to diagnose one or the other initially.
Both diseases are caused by sticky protein buildups in the brain. However, with Alzheimers disease, these protein build ups cause amyloid plaques, caused by the amyloid protein, and neurofibrillary tangles caused by the tau protein.
When these proteins accumulate, they interfere with the brain and bodys sense of communication, affecting cognition, movement, and behavior.
One of the key differences between the two diseases is hallucinations.
Hallucinations are common early on in people with LBD, but take a long time to develop for people with Alzheimers disease.
The other key indicators somebody has LBD rather than Alzheimers is developing Parkinsons-like tremors and muscle rigidity, and difficulty sleeping.
Pathogenic Mechanisms Beyond Lbs Or Lbs As An Indirect Indicator Of This Disease Spectrum
As follows from the previous consideration, the current concept behind classification within this disease spectrum is still based on retrospective clinicopathological studies, which focused exclusively on the presence of LBs and their clinicopathological relevance. However, since the initial description of LBs as a pathological hallmark of PD and the formulation of Braaks concept of the specific spread of LB pathology, evidence has been accumulating that not only LBs are key players in this group of diseases. So, what is the true significance of LBs in the pathogenesis of this disease spectrum, and what are the other biological relationships between the entities for which LBs are a common link?
Don’t Miss: How Does Parkinson’s Disease Affect Homeostasis
Find Time To Care For Yourself
As a caregiver, it is critical for you to take care of to maintain your own health and well-being. You may be at increased risk for poor sleep, depression, or illness as a result of your responsibilities. Watch for signs of physical or emotional fatigue such as irritability, withdrawal from friends and family, and changes in appetite or weight.
All caregivers need time away from caregiving responsibilities to maintain their well-being. Learn to accept help when it’s offered, and learn to ask family and friends for support. One option is professional respite care, which can be obtained through home care agencies and adult day programs. Similarly, friends or family can come to the home or take the person with LBD on an outing to give you a break.
Genetic Study Of Lewy Body Dementia Supports Ties To Alzheimers And Parkinsons Diseases
NIH-led study locates five genes that may play a critical role in Lewy body dementia.
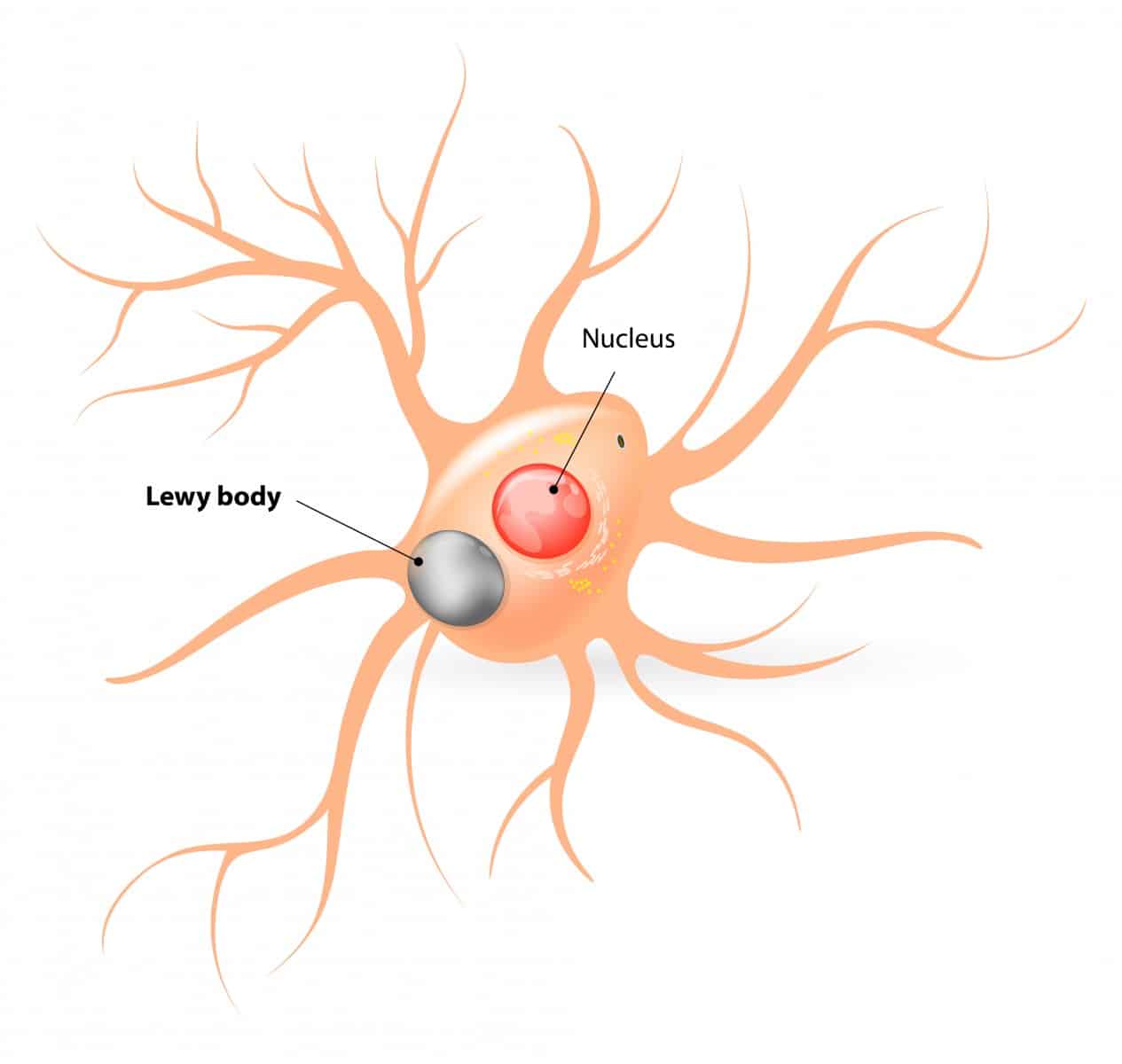
In a study led by National Institutes of Health researchers, scientists found that five genes may play a critical role in determining whether a person will suffer from Lewy body dementia, a devastating disorder that riddles the brain with clumps of abnormal protein deposits called Lewy bodies. Lewy bodies are also a hallmark of Parkinsons disease. The results, published in Nature Genetics, not only supported the diseases ties to Parkinsons disease but also suggested that people who have Lewy body dementia may share similar genetic profiles to those who have Alzheimers disease.
Lewy body dementia is a devastating brain disorder for which we have no effective treatments. Patients often appear to suffer the worst of both Alzheimers and Parkinsons diseases. Our results support the idea that this may be because Lewy body dementia is caused by a spectrum of problems that can be seen in both disorders, said Sonja Scholz, M.D., Ph.D., investigator at the NIHs National Institute of Neurological Disorders and Stroke and the senior author of the study. We hope that these results will act as a blueprint for understanding the disease and developing new treatments.
The study was led by Dr. Scholzs team and researchers in the lab of Bryan J. Traynor, M.D., Ph.D., senior investigator at the NIHs National Institute on Aging .
Article:
NIHTurning Discovery Into Health®
You May Like: Pilates For Parkinson’s Disease
Caring For Someone With Lewy Body Dementia
Caring for someone with LBD, or any form of dementia, is hugely challenging. Just as LBD can impact every aspect of a person, caring for someone with the disease can impact every aspect of your daily life. Youll likely face tests of stamina, problem solving, and resiliency. However, your caregiving journey can also be an intensely rewarding experience as long as you take care of yourself and get the support that you need.
Pd And Its Heterogeneity
Traditionally, sporadic PD has been recognized as a unique clinical entity, characterized by the presence of classical clinical signs, and by the typical pathology. The pathological hallmark of PD, the presence of LBs, was described by Friedrich Heinrich Lewy in his chapter of Max Lewandovskys neurology textbook, issued in Berlin in 1912. The disease-specific involvement of substantia nigra was then described by Tretiakoff in 1919, who also confirmed the existence of LBs . The fact, that LBs are formed predominantly by pathological alpha-synuclein was revealed by Spillantini and colleagues only 80 years later,. The presence of this alpha-synucleinopathy was listed as the typical pathological feature of PD, either sporadic or hereditary.
Table 1 Genes and cytogenetic locations in hereditary forms of Parkinsons disease their clinical phenotypes and neuropathological findings.
The fact that the same genetic variation may cause disparate clinical manifestations and pathological findings demonstrate a complex interplay of genetic, environment, and exposures. On the other side, there is a broad spectrum of clinical manifestations of typical Lewy-related brain pathology associated with various rare genetic abnormalities,,, where a similar combination of factors can be assumed.
Also Check: What Can You Do For Parkinson’s Disease
Diagnostic Criteria For Parkinson Disease Dementia
Consensus criteria for PDD were developed in 2007 .6,29 These criteria require cognitive impairments across multiple domains but emphasize that noncognitive features such as hallucinations are common. As described previously in the article, the clinical and neuropsychological features of DLB and PDD are similar. Indeed, it is the relative timing of dementia and parkinsonism that defines the clinical distinction between DLB and PDD. Controversy exists over how or whether to distinguish these syndromes.30
The 6 Stages Of Parkinsons And Lewy Body Disease
In 2003, Heiko Braak identified a pattern of Lewy body deposition, in the synucleinopathies , which include Parkinsons Disease , Multiple Systems Atrophy , Progressive Supra-nuclear Palsy and Dementia .
The pattern that he identified has been termed the Braak Staging of Lewy Body inclusions. More current research shows that Lewy Body pathology can spread from one area of the nervous system to another, and its conceivable that this happens in a prion-like fashion. There are also some studies that show alpha-synuclein is not only just an intracellular protein but is extracellular as well, which could explain to some degree, the progression to other areas of the brain.
The first three stages of Braaks staging, are largely asymptomaticto the uninformed individual.
In stage 1, inclusion bodies begin accumulating in the olfactory bulb and a part of our brainstem called the Vagus Nucleus. Symptoms at this point may include a change in the ability to smell and taste, as well as a constellation of symptoms we call autonomic symptoms, which are often casually related to aging. The symptoms may, or may not include: constipation, sexual dysfunction, dry eyes, dry skin, light-headedness, high blood pressure, insulin resistance, swelling of the hands and feet, bladder dysfunction, an increase in heart rate or arrhythmia, dizziness when getting out of a chair or bed, etc.
Stay tuned to the #TalkNeuro Blog!
Further Reading and Reference:
Also Check: Does Parkinson’s Affect Speech
What Is Parkinsons Disease
PD is a chronic, neurodegenerative movement disorder. PD affects 1 out of every 100 individuals over the age of 60, and patients commonly experience muscle rigidity, changes in speech and walking, and tremors.1
Some studies suggest that having PD also increases your risk of developing LBD, but most patients have only one of these conditions.2
Test Results Supporting Diagnosis
Physical and neurological examinations and various tests may help distinguish LBD from other illnesses. Specific tests that may support an LBD diagnosis include:
- A positron emission tomography scan or a single-photon emission computerized tomography scan showing reduced dopamine transporter uptake in the basal ganglia
- Abnormal 123iodine-MIBG myocardial scintigraphy showing reduced communication of cardiac nerves
- Sleep study confirming REM sleep behavior disorder without loss of muscle tone
Read more about diagnosing dementia, including tests and who can make a diagnosis.
There are no tests that can definitively diagnose LBD. Currently, only a brain autopsy after death can confirm a suspected diagnosis. However, researchers are studying ways to diagnose LBD earlier and more accurately during life. The use of certain imaging, blood, cerebrospinal fluid, and genetics tests is being studied.
Don’t Miss: Is There Pain Associated With Parkinson’s Disease
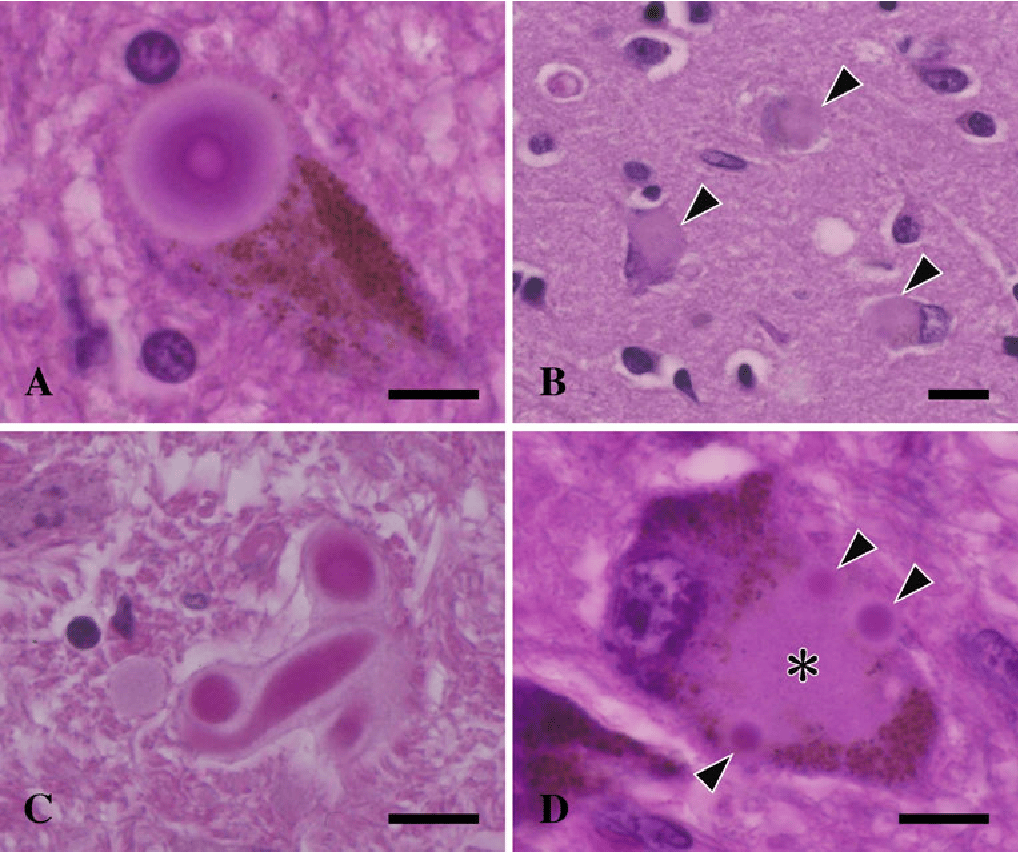
Enrichment Of Lewy Bodies From Postmortem Brains
Lewy bodies were purified from brain tissues of patients diagnosed with Lewy body variant of Alzheimers disease, whereas cases without LB pathology were used as negative controls, according to a previously reported protocol . Cortical tissues from both cases were dissected to remove white matter and then homogenized in a lysis buffer . The lysates were then centrifuged at 100,000 ×g for 30 min, and the pellets were resuspended in the lysis buffer and loaded on a sucrose gradient composed of three layers . After 200,000 ×g centrifugation for 2.5 hours, all interfaces were collected. An aliquot of each collected sample was smeared onto a glass slide and examined by immunostaining with -synuclein antibodies. In the LB cases, the fractions expected to contain LBs were enriched for round, -synuclein-immunoreactive structures ranging in diameter from 5 m to 30 m these structures were absent in the corresponding fractions from the control cases.
The Last Version Of Dlb Criteria Suggests The Use Of The General Term Lbd
The next subtype of LBD is the DLB phenotype. In contrast to PDD, this phenotype is a bit better bordered, its definition is more intelligible and the pathological finding is unique. This is characterized by diffuse alpha-synucleinopathy, accompanied in most cases by Alzheimers changes, especially senile plaques.
The birth of the DLB as a nosological entity was complicated and took many years of scientific debates, consensus meetings, publications, which ran continuously for almost the last decade of the 20th century. Finally, the existence of pathological co-habitation of Alzheimers pathological changes together with the diffuse appearance of LBs led the expert panel to the opinion, that the former attempts to name this disease were always the attempts to describe the findings typical for DLB.
The first clinical diagnostic criteria were published by McKeith et al. in 1996 the revised version came in 2005 and the last revision is from 2017,,. In the last revision, the nosological entity DLB has been classified rather as one of the phenotypes in the broader spectrum of LBD.
Read Also: Medications To Treat Parkinson’s
How Is Lewy Body Disease Treated
There is no cure for Lewy body disease, but a doctor may treat the symptoms with:
- Alzheimers disease medications to reduce hallucinations and behavioural problems
- Parkinsons disease medications to improve rigid muscles and slow movement
- antidepressants
- sleep medicines
Some medicines, such as antipsychotics, can make symptoms worse and may be dangerous. There are, however, other ways of dealing with symptoms, including:
- learning to manage a persons behaviour
- learning how to calm the person down
- changing their environment to help them function
- creating daily routines
- using therapies, such as physiotherapy, occupational therapy and speech and language therapy
- providing cognitive stimulation
People with Lewy body disease usually need help at home and eventually care in a nursing home. The disease progresses differently in different people. After they develop symptoms, people live on average for another 6 to 12 years, although some live much longer.
Understand Behavioral Changes In Lewy Body Dementia
Behavioral and mood problems in people with LBD can arise from hallucinations, delusions, pain, illness, stress, or anxiety. They may also be the result of frustration, fear, or feeling overwhelmed. The person may resist care or lash out verbally or physically.
Hallucinations and delusions are among the biggest challenges for LBD caregivers. The person with LBD may not understand or accept that the hallucinations are not real and may become agitated or anxious. Instead of arguing, caregivers can help by responding to the fears expressed. By tuning in to the person’s emotions, caregivers can offer empathy and concern, maintain the person’s dignity, and limit further tension.
Caregivers can try a variety of strategies to handle such challenging behaviors. Some behavioral problems can be managed by making changes in the person’s environment and/or treating medical conditions. Other problems may require medication.
Itâs also common for people with LBD to have difficulty falling asleep. Certain sleep problems can be addressed without medications. Increasing daytime exercise or activities and avoiding lengthy or frequent naps can promote better sleep. Avoiding alcohol, caffeine, or chocolate late in the day can help, too. Some over-the-counter medications can also affect sleep, so review all medications and supplements with a physician.
Read Also: What Is Parkinson’s Like
Lewy Body Dementia Research
Many avenues of research are being explored to improve our understanding of LBD. Some researchers are working to identify the specific differences in the brain between the two types of LBD. Others are looking at the disease’s underlying biology, genetics, and environmental risk factors. Still other scientists are trying to identify biomarkers , improve screening tests to aid diagnosis, and research new treatments.
Scientists hope that new knowledge about LBD will one day lead to more effective treatments and even ways to cure and prevent the disorder. Until then, researchers need volunteers with and without LBD for clinical studies.
NIH and other groups help people learn about clinical trials and studies and find research opportunities near them. Visit the following websites for details:
Whats The Difference Between Lewy Body Dementia Parkinsons Disease And Alzheimers Disease
Lewy body dementia is an umbrella term for two related clinical diagnoses: dementia with Lewy bodies and Parkinsons disease dementia. These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending on where the Lewy bodies first form.
Dementia with Lewy bodies is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a persons ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first in DLB. The motor symptoms of Parkinsons such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
Finally, Alzheimers is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
Also Check: How To Prevent Parkinson’s Disease
Behavioral And Mood Symptoms Of Lewy Body Dementia
Changes in behavior and mood are possible in LBD and may worsen as the persons thinking abilities decline. These changes may include:
- Apathy, or a lack of interest in normal daily activities or events and less social interaction
- Anxiety and related behaviors, such as asking the same questions over and over or being angry or fearful when a loved one is not present
- Agitation, or restlessness, and related behaviors, such as pacing, hand wringing, an inability to get settled, constant repeating of words or phrases, or irritability
- Delusions, or strongly held false beliefs or opinions not based on evidence. For example, a person may think his or her spouse is having an affair or that relatives long dead are still living.
- Paranoia, or an extreme, irrational distrust of others, such as suspicion that people are taking or hiding things
