The Spectrum Of Off In Parkinsons Disease
Hubert FernandezCleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH, USA
Despite the common nature of wearing-off and the substantial burden it exerts on both the patient and the healthcare system, it remains an under-recognised problem. Potential reasons for this include limited evaluation time for physicians, miscommunication between patients and caregivers, particularly with regard to the reporting of NMS such as cognitive dysfunction and urinary problems, and the lack of an established definition for wearing-off. Current definitions put a heavy emphasis on motor symptoms, potentially missing transition states between ON and OFF periods. This lack of an established definition is reflected in the results of a study by Stacy et al., where clinicians were shown to identify wearing-off in only 29.4% of cases, fewer than specific questionnaires such as the Unified Parkinsons Disease Rating Scale Part IV, Question 36 or the wearing-off patient questionnaire .1 However, even the gold-standard questionnaires are reliant on patient recall and only usually assess symptoms across a single day. It is hoped that with the advent of new mobile technologies it will be possible to assess patients more closely and for longer periods of time.9
How To Help Reduce Episodes
Off times become more common after people with PD have been taking medication for a longer time and as their disease progresses. While the presence of off times happens as a normal progression of PD, there are things that can help manage or reduce these episodes:
Treating Fatigue In Parkinsons Disease
There are currently few treatments available that directly alleviate fatigue, which can make it difficult to treat. However, people with PD who experience fatigue should talk to their doctor as changes in their current medications may help relieve fatigue. Complementary therapies, such as acupuncture or massage, may help improve symptoms of fatigue. In addition, there are several lifestyle approaches that can help manage fatigue, including:
Read Also: What Are The First Symptoms Of Parkinsons Disease
Recommended Reading: Does Parkinson’s Disease Cause Death
Is There Any Treatment
There is currently no effective treatment for PSP and symptoms usually do not respond to medications.
- Parkinsons disease medications, such as ropinirole, rarely provide additional benefit. In some individuals, other antiparkinsonian medications, such as levodopa, can treat the slowness, stiffness, and balance problems associated with PSP, but the effect is usually minimal and short-lasting.
- Botulinum toxin, which can be injected into muscles around the eyes, can treat excessive eye closing.
- Some antidepressant drugs may offer some benefits beyond treating depression, such as pain relief and decreasing drooling.
Non-drug treatment for PSP can take many forms.
- Weighted walking aids can help individuals avoid falling backward.
- Bifocals or special glasses called prisms are sometimes prescribed for people with PSP to remedy the difficulty of looking down.
- Exercise;supervised by a healthcare professional can keep joints limber but formal physical therapy has no proven benefit in PSP.
A gastrostomy may be necessary when there are swallowing disturbances or the definite risk of severe choking.
Deep brain stimulationwhich uses surgically implanted electrodes and a pacemaker-like medical device to deliver electrical stimulation to specific areas in the brain ;to block signals that cause the motor symptoms of several neurological disordersand other surgical procedures commonly used in individuals with Parkinsons disease have not
Motor Fluctuations Occur Early In Parkinsons Disease Progression
Fabrizio Stocchi presented a patient case, including the patient describing her symptoms during a routine clinical evaluation. Wearing-off was characterised by non-motor symptoms and motor symptoms , despite the early disease stage .
Table 1: Case study of wearing-off in early Parkinsons disease.PD: Parkinsons disease; TID: three times daily.
Wearing-off is investigated during a clinical evaluation in a number of ways. DEEP, a multicentre, observational study in 617 patients with PD, showed that wearing-off during the first years of PD was identified through a neurologist evaluation in 36.2% of patients and in 54.6% of patients using the Wearing-Off Questionnaire .4 A recent market research survey of 420 European healthcare professionals found that MF were most frequently identified by asking the patient or hearing directly from the patient about their wearing-off symptoms . Only 4% of those interviewed used the WOQ-19 tool, despite one-third of healthcare professionals recognising that MF are underdiagnosed, and one-quarter feeling that MF can be hard to diagnose during a routine neurological clinical evaluation . These data highlight the importance of assessment techniques in the recognition of early MF during a routine neurological clinical evaluation.
Don’t Miss: Parkinson’s Ribbon Color
Treatment Depends On Properly Identifying The Type
If pain is bilateral always assume it is central pain; pain due to PD. In my experience Azilect works great for this type of pain. Other medications which can be employed for this pain as well.
Massage therapy works for all types of leg pain-my favorite therapy but can be costly. Water therapy may also work for all types except central pain. Physical therapy can alleviate dystonia pain, as well as musculoskeletal and radicular pain.
If pain is due to dystonia related to levodopa intake, find out when it occursend of dose or at peak dose. Typically adjusting medication doses will resolve problem. However, if dystonia is an initial symptom of PD, initiating treatment with levodopa will resolve. If medication adjustment does not work well for levodopa induced dystonia, another treatment option is DBS . Pain due to dystonia independent of cause can also respond well to Botox injections, as well as centrally acting muscle relaxants. To avoid and alleviate pain caused by stiff muscles, a great treatment option is activity in the form of stretching exercisesany number of activities will do such as tai-chi or yoga. For me when I start having radicular pain shooting down my leg it is time to up my levodopa dosage.
If you are having leg pain make sure to discuss it with your physician.
Recommended Reading: How Does Parkinsons Disease Affect Mobility
How Is Wpw Syndrome Diagnosed
People experiencing a fluttering or racing heartbeat usually tell their doctors. The same applies to those experiencing chest pain of difficulty breathing. However, if you dont have symptoms, the condition may go unnoticed for years.
If you have a racing heartbeat, your doctor will likely perform a physical exam and conduct tests that measure your heart rate over time to check for tachycardia and diagnose WPW syndrome. These heart tests may include:
Also Check: Is Parkinson’s A Neuromuscular Disease
Types Of Motor Fluctuations
Motor fluctuations take a variety of forms:
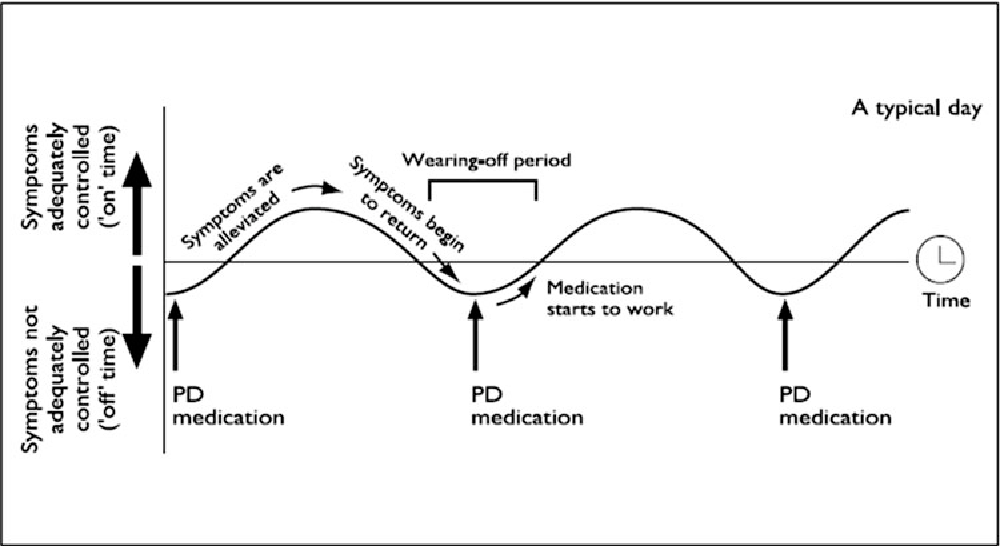
“On-off” phenomenon. You cycle between good control and periods of symptoms. During the “on” times, your symptoms are well managed. In “off” periods, the problems come back.
Some people only get “off” periods when their levodopa starts to wear off. Others get symptoms at random times that aren’t related to their medicine. Your doctor may prescribe add-on medications which can lessen the “off” times.
Wearing off. The effect of your levodopa starts to fade before it’s time to take the next dose. You might be tempted to take your medicine earlier than usual to prevent symptoms.
Delayed “on.” You have to wait longer than usual after you take levodopa for your symptoms to improve. This delay can happen when you take your first dose in the morning. It’s also common after meals, because the protein in your food can cause the medicine to get absorbed more slowly.
Delayed “on” is more common with time-release versions of levodopa. These drugs take a while to get from your stomach into your bloodstream and then travel to your brain.
Partial “on” or dose failure. Partial “on” means that your symptoms don’t fully improve after you take a dose of levodopa. A dose failure is when you don’t feel any better after taking your medicine.
You’re more likely to have freezing during an “off” period.
Dyskinesia. This is uncontrolled twitching, jerking, or other movements. It can affect one limb, such as an arm or leg, or your whole body.
Presynaptic Mechanisms In Wearing
The finding that motor improvement following acute intravenous levodopa challenge lasts longer in de novo and stable patients than in those who are already suffering motor fluctuations was key to the development of the storage hypothesis, which implies that loss of presynaptic dopaminergic terminals reduces the capacity of the striatum to store dopamine and buffer the oscillations in plasma levodopa levels . Certainly, the pharmacokinetics of levodopa-dopamine in the brain is drastically changed after dopaminergic denervation of the striatum. In the rat with a 6-hydroxydopamine lesion of the nigrostriatal pathway, peak striatal dopamine levels and the area under the curve for synaptic dopamine availability are significantly lower in animals with larger lesions , which correlates with a shorter duration motor response . In patients, the availability of dopamine in the synapse has been measured by PET using the D-2 receptor antagonist raclopride as the radioligand. Raclopride was administered before and after levodopa intake in patients with and without motor fluctuations, with the result that patients with motor fluctuations demonstrated a greater decrease in raclopride binding than stable patients. Because raclopride competes with dopamine for binding to D2 receptors, reduced raclopride uptake is an index of higher synaptic dopamine levels and, therefore, reduced numbers of dopaminergic terminals .
Recommended Reading: Does Alcohol Make Parkinson’s Symptoms Worse
What Causes Fatigue In Parkinsons
The precise mechanisms that cause fatigue are unclear but research suggests that any neurological disorder which involves the basal ganglia area of the brain is likely to be associated with significant fatigue. This includes Parkinsons.
In some cases Parkinsons medication may be a factor, for example dopaminergic medications may affect sleep and so add to fatigue. Dosage and timing of medication may also affect energy levels.
Fatigue may be linked to other Parkinsons symptoms, for example depression. With depression there is usually also fatigue, as well as loss of motivation, a general lack of interest and difficulty in sleeping. It is important that these symptoms are recognised as they are very treatable, and overcoming them can reduce fatigue.
If you experience tremor, rigidity or dyskinesia your muscles will have to work harder in order to carry out simple movements or tasks which can mean muscles fatigue more quickly and easily. Slowness of movement may also increase fatigue by making activities and tasks more prolonged and effortful.
You may have sleep;problems and poor quality sleep tends to lead to excessive day-time sleepiness and a tendency to nap. Although sleepiness is a separate symptom to fatigue, it clearly adds to the problem and fatigue is hard to overcome if you are sleepy.
Opicapone As An Early Treatment Option For Motor Fluctuations
The clinical efficacy and safety of opicapone as an adjunct therapy to levodopa has been demonstrated in two large, Phase III, multinational, randomised, double-blind studies with open-label extension periods. BIPARK-I was an active comparator and placebo-controlled study , and BIPARK-II was a placebo-controlled study .16-18 In both trials, the primary endpoint was change from baseline to end of study treatment in absolute OFF-time.16,18 In BIPARK-I, treatment with opicapone 50 mg was superior to placebo , and non-inferior to entacapone .16 In BIPARK-II, the adjusted treatment difference versus placebo was significant for opicapone 50 mg .18 Opicapone was generally well tolerated, with the most common adverse events associated with opicapone treatment including dyskinesia, insomnia, constipation, and dry mouth.16,18
Read Also: How To Treat Parkinson’s
What Causes Wpw Syndrome
Doctors arent sure what causes WPW syndrome. The extra electrical pathway in the heart is present at birth, so its likely caused by some abnormality that occurs during fetal development. A small percentage of people with WPW syndrome have been found to have a gene mutation that is thought to be responsible for the disorder.
In a normal heart, the heartbeat is initiated by the sinus node in the upper right section of the heart muscle. This is where the electrical impulses that start each heartbeat begin. Those impulses then travel to the atria, or upper heart chambers, where the initiation of contraction occurs. Another node called the atrioventricular node, or AV node, then sends the impulse to the lower heart chambers called the ventricles where ventricular contraction occurs and the blood is pumped out of your heart. Ventricular contraction is much stronger than atrial contraction. The coordination of these events is essential for maintaining a normal, regular heartbeat and rhythm.
In a heart affected by WPW syndrome, however, an extra electrical pathway can interfere with the normal heartbeat. This extra pathway creates a shortcut for the electrical impulses. As a result, these impulses may activate the heartbeats too early or at the wrong time.
If its left untreated, the abnormal heartbeat, arrhythmia, or tachycardia, can cause blood pressure, heart failure, and even death.
Pathophysiological Mechanisms In Wearing
A wearing-off effect is the normal and predictable response of any sensitive pharmacological system when activated with a potent but short-acting agent. There are numerous and well-accepted examples in general pharmacology and clinical practice. For example, an SDR is expected for morphine analgesia; pilocarpine drops for mydriasis or adrenaline subcutaneous administration to increase blood pressure and heart rate. Similarly, levodopa has a plasma half-life of 6090 min and possesses a very powerful antiparkinsonian effect. So, it is not surprising that such stimulation of the dopaminergic system in PD leads to a change in response that manifests as wearing-off and other motor complications. In this section, we review the main pathophysiological mechanisms implicated in the origin of motor fluctuations in PD.
You May Like: How Is The Brain Affected By Parkinson’s Disease
Fabrizio Stocchi Mnica Kurtis And Francesca Morgante
Levodopa remains the gold standard of symptomatic efficacy for the treatment of motor symptoms in patients with PD;1 however, as the disease progresses, patients develop motor response oscillations such as end-of-dose wearing-off and levodopa-induced dyskinesias.2,3 Wearing-off, a result of decreased therapeutic effect of levodopa/DDCI, represents a major source of disability for patients with PD, impacting on quality of life.4 Wearing-off also presents a considerable problem in the overall management of PD. Key to the timely detection and management of wearing-off is the ability to recognise that it can be present in the early stages of this disease.
Tips For Coping With Fatigue
- Eat well.
- Stay hydrated.
- Exercise: walk, do tai chi, dance, cycle, swim, do yoga or chair yoga whatever you enjoy. Fatigue may make it hard to start exercising, but many people say it makes them feel more energetic afterward. If you find it difficult to get going, consider exercising with another person or a group.
- Keep a regular sleep schedule. If you have difficulty sleeping because of tremor or stiffness, trouble rolling over, or needing to use the bathroom, talk to your doctor about these issues.
- Take a short nap after lunch. But avoid frequent naps throughout the day, or napping after 3:00 PM.
- Stay socially connected.
- Pace yourself: plan your day so that you are active at times when you feel most energetic and have a chance to rest when you need to.
- Do something fun: visit with an upbeat friend, or pursue a hobby.
- At work, take regular short breaks.
Note:;Fatigue has been identified by the Parkinsons community as an unmet need through the PDF Community Choice Research Awards. In response, PDF is investing in research to understand and solve fatigue in Parkinsons.
Content for this article was derived from Fatigue, and Fighting Fatigue on PDF.com
Recommended Reading: How Does Parkinson’s Disease Affect The Mitochondria
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
What You Can Do
As of 2021, there is no definite cure for Parkinsons disease. There is also no definite known cause. Its likely due to a combination of an individuals susceptibility and environmental factors. Most cases of Parkinsons disease happen without a genetic link.
According to research published in 2012, only report having a family member with the disease. Many toxins are suspected and have been studied, but no single substance can be reliably linked to Parkinsons.
However, research is ongoing. Its estimated that
Dont Miss: What Gene Mutation Causes Parkinsons Disease
Also Check: What Is Dbs Surgery For Parkinson’s Disease
Characteristics Of Patients With Wo
According to clinician assessments, patients were divided into the WO group and Non-WO group. Compared with the Non-WO group, the WO group showed younger age at onset , lower weight , longer disease duration , higher H&Y staging , higher daily levodopa dose and daily levodopa equivalent dose , and longer duration of antiparkinsonian medical treatment and levodopa treatment . In terms of the medication types, the WO group used levodopa/benserazide , levodopa/cabidopa , pramipexole , and amantadine more frequently than the Non-WO group. In addition, the WO group was much frequently treated with polytherapy of levodopa and other medications compared to the Non-WO group . No difference was found in the gender ratio or age between the two groups. In order to identify the WO-associated factors, we included all factors that showed significant differences into the multivariate logistic regression model. It showed that disease duration , H&Y staging , and the LED were associated with the occurrence of WO.
