How Does Parkinsons Disease Cause Sleep Problems
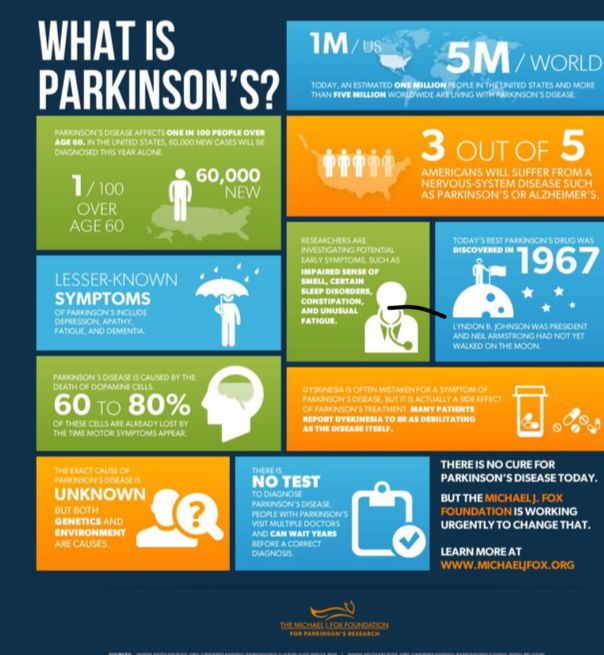
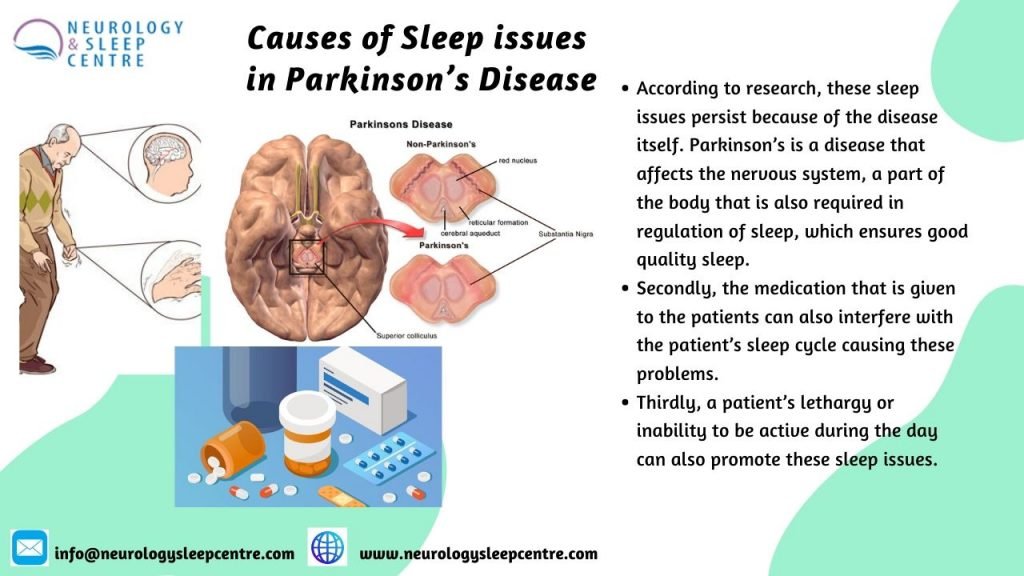
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Deep Brain Stimulation In The Treatment Of Sleep Disorders In Pd
Studies investigating the effect of DBS in the treatment of sleep disorders in PD patients showed that DBS improved the sleep scales and quality . Baumann-Vogel et;al. found that subthalamic nucleus DBS-enhanced subjective sleep quality, reduced sleepiness measured by the Epworth sleepiness scale, and reduced sleep fragmentation shown by actigraphy recordings. However, the authors observed that subthalamic DBS was not improved REM sleep features . Similarly, Cicolin et;al. reported that RBD symptoms did not benefit from STN DBS.;On the other hand, Chahine et;al. reported that STN DBS improved significantly symptoms of RLS in PD patients. The effect of PPN DBS on sleep disorders in PD has been investigated in several studies . One study showed that PPN DBS improved sleep quality and reduced EDS; however, it caused a reduction in REM latency and a relevant increase in REM sleep . In another study, it has been reported that PPN DBS improved the total duration and rate of REM sleep . As a result, DBS seems to be beneficial in the treatment of sleep disorders in PD because it seems to be useful in improving sleep quality. However, large-scale prospective studies are needed to understand the benefits of DBS in the treatment of sleep disorders in PD.
Insomnia In Multiple Sclerosis
Multiple sclerosis is frequently associated with sleep disorders: Insomnia , RLS and sleep related breathing disorder . The causes for insomnia are manifold, and include primary insomnia, pain, nocturia, spasticity and obesity. Some specific MS drug regimens can contribute to insomnia. Insomnia is associated with physical and functional impairment and depression. Depending on criteria and type of assessment 2554% of MS patients suffer from non-restorative sleep .
At MS onset sleep quality in younger adults is mainly normal . The risk to develop insomnia is associated with increased fatigue scores . A prospective multicenter study in Portugal including 206 MS patients, detected chronic insomnia in 22,6%, frequently associated to female sex, anxiety disorder, fatigue and presence of other comorbidities . Others described a prevalence of insomnia varying between 13,2% of MS patients with relapsing and remitting MS and 12,5% with about half of them suffering from RRMS . In 10,000 MS patients and 40,000 matched controls from a database insomnia was identified as a prodromal symptom of MS occurring up to 10years prior to disease onset . MS patients with insomnia showed a higher arousal level than patients with insomnia only or patients with other neurological disorders . A Dutch study showed that in MS patients with sleep disturbances cognitive impairment was pronounced and thalamic functional connectivity was impaired .
Recommendations
Read Also: Life Expectancy Of Parkinson’s Patients
Diagnosis Of Rbd In Pd
The diagnosis of RBD can be based on a questionnaire or clinical manifestations without confirmation by polysomnography .Therefore, a detailed history of complex motor behaviors and vocalizations during REM sleep is very important for a clinical diagnosis of RBD.;However, for the objective diagnosis of RBD, complex motor behaviors during REM sleep and the presence of REM sleep without atonia should be confirmed by PSG . Additionally, this sleep disturbance should not be better explained by another disorder . PSG can detect increased chin muscle tone by the submental EMG or increased phasic muscle activity by the limb EMG during REM sleep . Thus, PSG is not required for the clinical diagnosis of RBD . It has been reported that a total score of 6 or higher obtained from the RBD screening questionnaire used for the clinical diagnosis of RBD may strongly support the diagnosis .
Rem Sleep Parasomnia In Parkinson’s Disease And Dementia With Lewy Bodies

REM sleep behavior disorder was first described by Schenck et al. and is characterized by a loss of normal muscle atonia during REM sleep associated with coordinated limb movements that mirror dream content. The actions made during REM sleep can be quite vigorous and themes often include defending oneself or others , though not exclusively , and may be associated with injuries. There seems to be far greater male representation in RBD, though it is unclear whether this reflects a referral bias, hormonal effects or a genetic relationship to the underlying pathology. The treatments of choice are clonazepam and more recently, melatonin .
It is important to distinguish RBD from other parasomnias or sleep disorders through polysomnography for proper intervention and to ensure that other sleep conditions are not present that may mimic RBD or that may be exacerbated with the use of clonazepam. For example, severe OSA may include flailing of the limbs and hollering, and nocturnal wandering, confusional arousals and sleep walking , may also be hard to distinguish from RBD without polysomnography. Patients are often unaware of their sleep behavior, and it is crucial to obtain information from a bed partner or somebody who has witnessed the patient’s sleep.
RBD in PD has been associated with orthostatism and non-tremor predominant parkinsonism . Those with PD and RBD are more likely to have cognitive impairment and an earlier onset of dementia than PD patients without RBD .
Also Check: Parkinson’s Life Expectancy After Diagnosis
Pathophysiology Of Rbd In Pd
REM sleep is regulated by the brain stem, hypothalamus, thalamus, substantia nigra, basal forebrain, and frontal cortex . The brain stem structures involved in REM sleep include the pedunculopontine nucleus , retro-rubral nucleus, subcoeruleus/sublateral dorsal nucleus, and medullary magnocellular reticular formation . These brain stem structures provide REM atonia by inhibiting the spinal motor neurons through direct and indirect pathways . Thus, these two inhibitory pathways play a role in skeletal muscle atonia during REM sleep . The PPN and the retro-rubral nucleus also act as a phasic generator circuitry . It is well known that the PPN/laterodorsal tegmental nuclei have both cholinergic activity and non-cholinergic activity. So the PPN/LDN also contains glutamatergic and GABAergic neurons . On the other hand, the cholinergic neurons in the PPN/LDN innervate the pontine reticular formation , MRF, and thalamus . Thus, descending projections of the PPN stimulate the inhibitory interneurons via the reticulospinal neurons and inhibit directly the motor neurons in the spinal cord and modulate the activations of the mesencephalic locomotor region . It has been reported that inhibition of GABA activity in the PPN, an important part of locomotion, results in explosive motor behavior . In addition, the ascending projections to the thalamus from the PPN modulate the sleep
19 ].
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
Recommended Reading: Life Expectancy Of Someone With Parkinson’s
When Should I Call My Healthcare Provider
Reach out to your provider if trouble sleeping harms your quality of life. Always call your healthcare provider if you experience symptoms that worry you, especially if they could put you or those around you in danger.
Sometimes, a sleep disturbance could be a sign of depression related to Parkinson’s disease. If youve lost interest in activities you once loved or feel numb to whats going on in your life, reach out to a provider you trust. Some people feel better after starting a new medication or talking to someone about what theyre feeling. You dont have to feel like this.
A note from Cleveland Clinic
Researchers continue to study the sleep-Parkinsons disease relationship. Understanding more about how Parkinsons affects sleep may lead to earlier detection of Parkinsons disease and more effective treatments. Even now, you have plenty of options to treat sleep problems. Be open with your provider about any sleep issues youre having. Together, you can find a plan that improves your sleep as well as any other challenges Parkinsons disease may create in your life.
Natural Course Of And Risk Factors For Eds In Pd
In a multicenter study, EDS was found in 165 of 436 PD patients, and logistic regression analysis revealed that male sex, Movement Disorder Society -sponsored revision of the Unified Parkinsons Disease Rating Scale III scores , hallucinations, and MDS-UPDRS II scores were associated with EDS . In the analysis by clinical subtype, ESS scores were significantly higher in the patients with the postural instability and gait disturbance type than in those with the tremor-dominant type. The prevalence of EDS increases after the onset of PD motor symptoms. In an 8-year follow-up study of 232 PD patients, the proportion of patients with EDS increased from 5.6%at the beginning of the study to 22.5%at 4 years and 40.8%at 8 years . Logistic regression analysis showed that factors contributing to EDS were older age, male sex, and dopamine agonist use, but in a subanalysis of the patients who were never treated with dopamine agonists, the predictor of EDS was Hoehn-Yahr stage alone. This result indicates that EDS is related to disease severity, independent of the effects of dopamine agonists.
Don’t Miss: Does Parkinson’s Affect Vision
Restless Sleep May Be An Early Sign Of Parkinson’s Disease
- Date:
- Aarhus University
- Summary:
- Patients with the RBD sleep behavior disorder lack dopamine and have a form of inflammation of the brain, researchers have found. This means that they are at risk of developing Parkinson’s disease or dementia when they grow older.
Researchers from Aarhus University have discovered that patients with the RBD sleep behaviour disorder lack dopamine and have a form of inflammation of the brain. This means that they are at risk of developing Parkinson’s disease or dementia when they grow older.
Do you sleep restlessly and hit out and kick in your sleep? This could be a sign of a disorder associated with diseases of the brain. Researchers from Aarhus University have studied the condition of the dopamine producing nerve cells in the brain and cells that participate in the brain’s immune system in people suffering from the sleep disorder Rapid eye movement sleep behaviour disorder, RBD.
The study shows that patients suffering from RBD have a risk of developing Parkinson’s disease or dementia in the future, because they already suffer from a lack of dopamine in the brain. Parkinson’s disease occurs precisely because the group of nerve cells in the brain that produce dopamine stop working.
“These patients have an inflammation of the brain in the area where the dopamine-producing nerve cells are found,” says one of the researchers behind the study, Morten Gersel Stokholm from Aarhus University and the PET Centre at Aarhus University Hospital.
Changes In Sleep With Aging
As people age, they experience a number of changes in their circadian rhythms, and among the most noticeable are the changes in the sleep-wake cycle.; Older people tend to wake up earlier and go to bed earlier than they did when they were younger. ;They wake up more often during the night and have more difficulty going back to sleep than younger people.; They also tend to sleep more during the daytime hours.; Therefore, if one looks at total sleep time over the 24-hour day, the total time spent sleeping changes very little but the distribution of sleep may be quite different.; Younger people experience a consolidated nighttime episode with little or no daytime sleep, whereas older individuals experience sleep episodes throughout the 24-hour day.; Daytime sleepiness is affected by two major factors:; the amount and quality of nighttime sleep, and the strength of the circadian rhythm.; In addition, older people tend to have a reduced amount of N3 or deep slow wave sleep.
Also Check: Does Parkinson’s Run In Families
Sleep Disorders In Parkinsons Disease
In this 17-minute lecture Dr Gary Leo discuses sleep challenges caused by the neurochemical changes, medications and mood disturbances of Parkinsons disease, and normal changes of aging. ;He discusses possible causes and treatment options of sleep maintenance insomnia, REM Sleep Behavior Disorder, daytime sleepiness, sleep apnea, and restless leg syndrome, ending with some tips for good sleep.
Beating The Lockdown Blues
Did you knowBodily functions are heavily influenced by biological clocks which are distributed throughout your body . Your clocks primary role is timing and orchestrating your bodys everyday vital functions and aligning these to geophysical and social schedules. Disruptions to your daily routine derail your clock which reflects negatively on your mood, energy, sleep, digestion, heart and immune system, just to name a few!
With COVID-19-related lockdowns causing unanticipated disruptions to our routine,;Researchers at the University of Queensland have developed some guidelines to stay on a schedule to improve sleep and support;your health and wellbeing.
Also Check: Parkinsons Double Vision
Parkinson’s Disease And Insomnia
LTK: What factors contribute to insomnia in patients with Parkinson’s disease?
RG: We’re all familiar with the motor symptoms of Parkinson’s Disease….the tremors, slow shuffling walking, masked face and hunched posture, but the non-motor symptoms are equally problematic for the patients. These include low, or fluctuating blood pressure, problems with bowel elimination, sexual dysfunction, excessive urination, and disruption of the sleep/wake cycle. Many Parkinson’s patients only sleep for a few hours at night, and then struggle with sleepiness all day.
LTK: Is there a connection between rapid eye movement disorder and Parkinson’s disease?
RG: Certainly, they are intimately connected. People experiencing rapid eye disorder will often have vivid, frightening dreams or hallucinations, or even night terrors, which can be very distressing to the patient. These kinds of episodes should be reported to the patient’s neurologists. Treatment is essentially the same as for PD , but a mild mood stabilizer may be added for additional relief.
Lifestyle Causes Of Insomnia
Lifestyle Habits. Lifestyle habits that can contribute to insomnia are not having a regular bedtime routine, not having a comfortable or safe sleep environment, and using technology before bedtime are all examples of things that can give you sleep problems.
Lifestyle habits, such as consumption of nicotine, caffeine, and alcohol can also lead to insomnia.
If you have insomnia, its important to take a look at what may be causing your sleeplessness.
Insomnia can lead to a number of problems including daytime fatigue, poor job performance, worsening symptoms of anxiety or mental illness, or accidents while driving. If left untreated it can lead to more serious health conditions.
Fortunately, whatever it is thats causing your anxiety can likely be corrected, and many times without medication.
If youre having trouble sleeping and think you may have insomnia, your doctor can help you figure out the best treatment for you.
Read Also: Life Expectancy After Parkinson’s Diagnosis
Sleep And Parkinsons Disease
The Palo Alto Parkinsons Disease support group February 2020 meeting featured Dr. Emmanuel During, a Stanford sleep medicine neurologist.; During the meeting, Dr. During discusses sleep disturbances that can occur in PD, such as insomnia, restles legs syndrome, sleep apnea, and REM sleep behavior disorder , along with available treatments.; There’s a question and answer session.
Valerian Root And Other Herbal Supplements
A quick tour in the supplement aisle at a grocery store can give you a dizzying array of herbal supplements advertised to improve sleep. Valerian root is one of the most widely recognized. Although it has the potential for significantly enhancing sleep, people often experience residual sleepiness the next day.
Typically, you will find products combining several different compounds. The ability of these different compounds to induce sleep has;not necessarily been studied, particularly in people living with Parkinsons. If youre interested in trying one of these products, consult your doctor with a list of the ingredients before attempting to incorporate them into your sleep routine.
Also Check: Can Parkinson’s Run In The Family
Evaluation Of Sleep Hygiene Program: Sleep Diary
Monitoring the effectiveness of behavior changes is best done by keeping a diary.; The table below depicts a sample diary that could be kept by the bedside and filled out upon arising by the patient or caregiver.; If daytime sleepiness and napping are problems, items can be added to record the number, time, and duration of napping episode. The diary can be carried with the patient.
Insomnia In Neurodegenerative Movement Disorders
The recommendations are restricted to Parkinsons disease , atypical Parkinson syndromes, and spinocerebellar ataxia .
Sleep disorders in neurodegenerative diseases affect up to 90% of all patients. Sleep disorders in neurodegenerative diseases can precede motor symptoms by years and may exhibit unfavorable impact on quality of life and cognition . Insomnia is the most frequently associated sleep disorder . 3560% fulfill the criteria of chronic insomnia .
To screen for sleep problems and score their severity in PD the task force of the Movement Disorder Society recommends the use of the following scales and questionnaires: Parkinsons disease sleep scale , Pittsburgh sleep quality index and SCOPA-Sleep .
In PD patients the amplitude of the rhythmic expression of clock genes such as per 2 as well as the transcription factor bmal 1 was reduced, supposedly influencing gene transcription and inflammatory processes. These changes of circadian processes might be a consequence of the ongoing neurodegenerative process but may also contribute to disease progression itself . Analyses of a national data banks in Great Britain and Taiwan showed a prodromal incidence risk of insomnia for clinical manifestation of PD of 1,38 .
Recommendations
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease