What Are The Symptoms
Symptoms of PD vary from person to person, as does the rate of progression. A person who has Parkinson’s may experience some of these more common “hallmark” symptoms:
- Bradykinesia – slowness of movement, impaired dexterity, decreased blinking, drooling, expressionless face.
- Tremor at rest – involuntary shaking that decreases with purposeful movement. Typically starts on one side of the body, usually the hand.
- Rigidity – stiffness caused by involuntary increase in muscle tone.
- Postural instability – sense of imbalance. Patients often compensate by lowering their center of gravity, which results in a stooped posture.
Other symptoms that may or may not occur:
Freezing or being stuck in place Shuffling gait or dragging of one foot Stooped posture Cognitive impairment
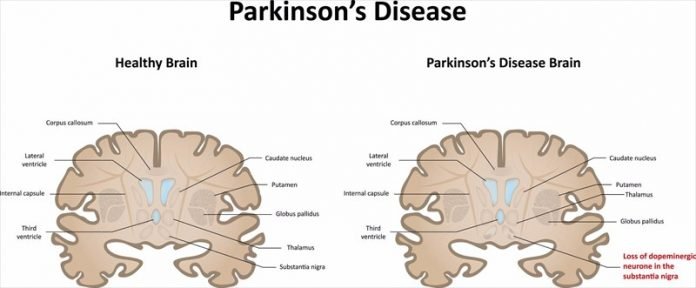
How Parkinsons Disease Affects The Brain
The Parkinson’s disease brain stops producing dopamine cells, which in turn causes problems with movement and coordination known as motor symptoms. We all have a basic understanding of how Parkinson’s disease affects the brain, but what really happens when someone has Parkinson’s disease? Let’s explore the facts surrounding the Parkinson’s disease brain and how it differs from a normal, “healthy” brain.
The Effects Of Parkinsons Disease
* Memories: Brain stores short-term memories of the experience in a part of the brain called the hippocampus, then those memories are later consolidated and transferred to another part of the brain, more precisely in neocortex, for a long-term storage; Memory cells are placed in three parts of the brain, the hippocampus, the prefrontal cortex, and also the basolateral amygdala, which is responsible of emotional associations. In fact these cells are necessary to evoke the emotions linked with
Parkinsons Doesnt Always Cause Dementia
While cognitive decline is common in both Alzheimers and Parkinsons, it is less likely to occur in Parkinsons patients. According to studies, only half of those with Parkinsons develop cognitive difficulties. This can range from mild forgetfulness to full-blown dementia.
When dementia does manifest itself with Parkinson, it occurs in the subcortical area of the brain. Alzheimers dementia occurs in the cortical area of the brain. As a result of this, the clinical symptoms of these two dementias can be somewhat different.
What Treatments Are Available
Many Parkinson’s patients enjoy an active lifestyle and a normal life expectancy. Maintaining a healthy lifestyle by eating a balanced diet and staying physically active contributes to overall health and well-being. Parkinson’s disease can be managed with self-care, medication, and surgery.
Self careExercise is as important as medication in the treatment of PD. It helps maintain flexibility and improves balance and range of motion. Patients may want to join a support group and continue enjoyable activities to improve their quality of life. Equally important is the health and well being of the family and caregivers who are also coping with PD. For additional pointers, see Coping With Parkinsons Disease.
These are some practical tips patients can use:
Medications There are several types of medications used to manage Parkinson’s. These medications may be used alone or in combination with each other, depending if your symptoms are mild or advanced.
After a time on medication, patients may notice that each dose wears off before the next dose can be taken or erratic fluctuations in dose effect . Anti-Parkinsons drugs can cause dyskinesia, which are involuntary jerking or swaying movements that typically occur at peak dosage and are caused by an overload of dopamine medication. Sometimes dyskinesia can be more troublesome than the Parkinsons symptoms.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Causes Parkinsons Disease
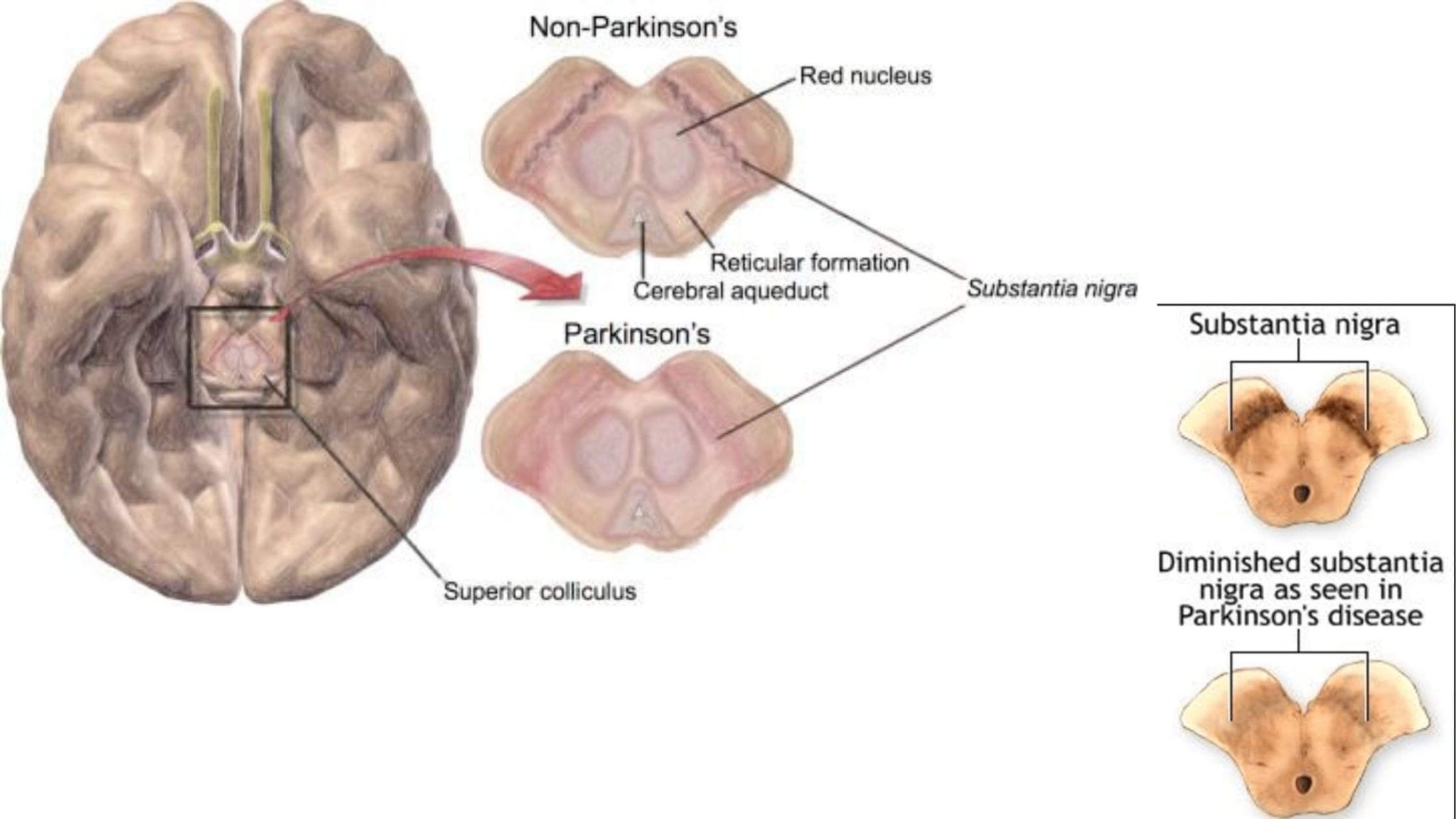
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Language Dysfunction In Parkinsons
There are several functions within language, including naming objects, generating words, comprehension, and verbal concepts. PD most often affects a persons ability to find a word, although as PD progresses, additional language difficulties may develop, including difficulty naming, difficulty comprehending information, and the use of more simplified and less spontaneous speech.3,4
What Causes Parkinson’s Disease
Parkinson’s disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
What Exactly Are Lewy Bodies
Lewy bodies are “clumps” of protein that accumulate in the outer layers of the brain, also known as the cortex. In addition to Parkinson’s, they are also a feature of dementia. Although we don’t know precisely what part Lewy bodies play in Parkinson’s disease or dementia, we do know that they are not the sole cause of Parkinson’s disease and its various symptoms. Some studies indicate that dopamine cells die before they even reach this part of the brain, but this is unconfirmed.
Despite the enigma of the Parkinson’s brain, many scientists have identified Lewy bodies as a potential target for new treatments. These treatments for Parkinson’s disease could be available in a matter of years, not decades.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Causes Of Parkinsons Disease
At present, we do not know the cause of Parkinsons disease. In most people there is no family history of Parkinsons Researchers worldwide are investigating possible causes, including:
- environmental triggers, pesticides, toxins, chemicals
- genetic factors
- combinations of environment and genetic factors
- head trauma.
How Is Parkinson’s Disease Managed
Your doctors will tailor your treatment based on your individual circumstances. You will manage your condition best if you have the support of a team, which may include a general practitioner, neurologist, physiotherapist, occupational therapist, psychologist, specialist nurse and dietitian.
While there is no cure for Parkinson’s disease, symptoms can be treated with a combination of the following.
Related Diagnosis: Lewy Body Dementia
Current research is helping to differentiate dementia related conditions in relationship to Parkinsonâs disease. Doctorâs use a 12-month arbitrary rule to aid in diagnosis. When dementia is present before or within 1 year of Parkinsonâs motor symptoms developing, an individual is diagnosed with DLB. Those who have an existing diagnosis of Parkinsonâs for more than a year, and later develop dementia, are diagnosed with PDD.
In the simplest terms, Lewy bodies are abnormal clumps of proteins that develop in nerve cells. Cholinesterase inhibitors, medications originally developed for Alzheimerâs disease, are the standard treatment today for cognitive DLB and PDD symptoms. Early diagnosis is important, as DLB patients may respond differently than Alzheimerâs disease patients to certain drug, behavioral, and dementia care treatments.
This challenging, multi-system disorder involving movement, cognition, behavior, sleep, and autonomic function requires a comprehensive treatment approach to maximize the quality of life for both the care recipient and their caregiver. It is very important to pay attention to symptoms of dementia and to search for an expert clinician who can diagnose the condition accurately.
The Substantia Nigra And Movement
The reason that Parkinsons causes movement symptoms is that the substantia nigra makes up part of the circuitry, called the basal ganglia, that the brain uses to turn thought about movement into action.
The structures of the basal ganglia.
The substantia nigra is the master regulator of the circuit, it mainly communicates using the chemical dopamine, but other chemical transmitters are also used to communicate between other areas of the basal ganglia.
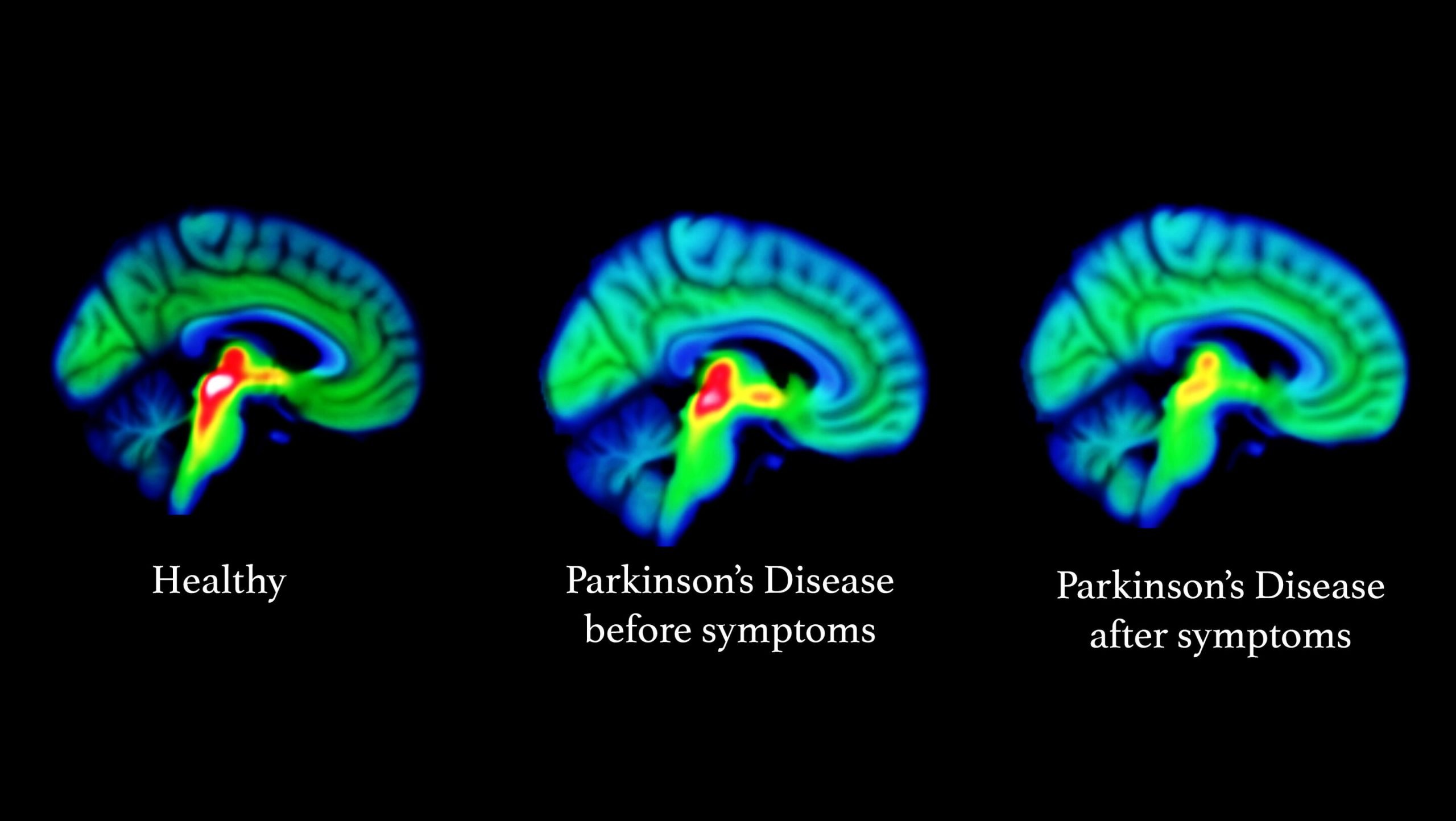
The balance of signals being sent between these structures allows us to control movement. But as Parkinsons progresses, and the dopamine-producing brain cells in the substantia nigra are lost, movement symptoms appear. Without enough dopamine, it becomes harder to start and maintain movements, which leads to symptoms such as slowness of movement, rigidity and freezing. And an imbalance of signals in the basal ganglia means people with Parkinsons can experience what is known as a resting tremor.
But while this is the description of Parkinsons you may find in most textbooks, it is now recognised that changes are not limited to the substantia nigra and basal ganglia.
What Does Parkinson’s Do To The Brain
Deep down in your brain, there’s an area called the substantia nigra, which is in the basal ganglia. Some of its cells make dopamine, a chemical that carries messages around your brain. When you need to scratch an itch or kick a ball, dopamine quickly carries a message to the nerve cell that controls that movement.
When that system is working well, your body moves smoothly and evenly. But when you have Parkinson’s, the cells of your substantia nigra start to die. There’s no replacing them, so your dopamine levels drop and you can’t fire off as many messages to control smooth body movements.
Early on, you won’t notice anything different. But as more and more cells die, you reach a tipping point where you start to have symptoms.
That may not be until 80% of the cells are gone, which is why you can have Parkinson’s for quite a while before you realize it.
Medications For People With Parkinsons Disease
Symptoms of Parkinsons disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinsons medications fit into one of the following broad categories:
- levodopa dopamine replacement therapy
- dopamine agonists mimic the action of dopamine
- COMT inhibitors used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors prevent the metabolism of dopamine within the brain.
Researchers Examine How Parkinsons Disease Alters Brain Activity Over Time
Tracking neural changes could help researchers test therapies that slow disease progression.
Neuroscientists peered into the brains of patients with Parkinsons disease and two similar conditions to see how their neural responses changed over time. The study, funded by the NIHs Parkinsons Disease Biomarkers Program and published in Neurology, may provide a new tool for testing experimental medications aimed at alleviating symptoms and slowing the rate at which the diseases damage the brain.
If you know that in Parkinsons disease the activity in a specific brain region is decreasing over the course of a year, it opens the door to evaluating a therapeutic to see if it can slow that reduction, said senior author David Vaillancourt, Ph.D., a professor in the University of Floridas Department of Applied Physiology and Kinesiology. It provides a marker for evaluating how treatments alter the chronic changes in brain physiology caused by Parkinsons.
For decades, the field has been searching for an effective biomarker for Parkinsons disease, said Debra Babcock, M.D., Ph.D., program director at the NIHs National Institute of Neurological Disorders and Stroke . This study is an example of how brain imaging biomarkers can be used to monitor the progression of Parkinsons disease and other neurological disorders.
The study was supported by the NIH .
NIHTurning Discovery Into Health®
Further Information And Support
- Building 21, Macquarie Hospital, 120 Coxs Road , North Ryde NSW 2133Freecall 1800 644 189
- 20 Kingston Road, Cheltenham VIC 3192Ph 9551 1122
- PO Box 1684, Springwood QLD 4127Ph 3209 1588
- 23A King William Road, Unley SA 5061Ph 8357 8909
- Centre for Neurological Support, The Niche Suite B, 11 Aberdare Road, Nedlands WA 6009Ph 9346 7373
- PO Box 222, Calwell ACT 2905Ph 6278 8916
- Locked bag 4, Sandy Bay TAS 7005Ph 6229 2509
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Living With Parkinson’s Disease

Coming to terms with a diagnosis of Parkinson’s and living with the disease is challenging and will take a lot of adjustment. There are still things you can do that can help you to feel more in control of your situation and to stay positive. Some things that might help could include:
- choosing to lead a healthy lifestyle
- making informed decisions related to your treatment
- keeping a diary of your symptoms in preparation for meetings with health and social care professionals
- attending a self-management course
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinsons. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinsons may take some time.
No two people with Parkinsons disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinsons disease symptoms through:
- seeing a Doctor who specialises in Parkinsons
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Research Is Underway To Further Understand The Cardiac Effects Of Parkinsons
It is possible to image the sympathetic nervous system of the human heart by injecting a radioactive tracer, meta-iodo-benzyl-guanidine, . Development of this technique, known as MIBG cardiac imaging, holds much promise as a test to confirm the diagnosis of PD , to identify those who are at risk of developing PD in the future, and to distinguish PD from related disorders. MIBG cardiac imaging is still considered an experimental procedure for detection of PD and is not yet in use as a clinical tool for this purpose.
A recent research was conducted in monkeys in which the destruction of the sympathetic nerves of the heart was chemically induced to mimic the changes that are seen in PD. The cardiac system was then imaged using a number of new-generation radioactive tracers, which bind to markers of inflammation and oxidative stress. This model system may help to shed light on the molecular changes that accompany the loss of the sympathetic nerves of the heart and can also be used to track the response of the cardiac system to therapeutic agents.
Parkinsons & Other Brain Areas
After the substantia nigra changes and dopamine levels drop, the effects of Parkinsonâs may eventually spread to other areas of the brain. In later stages of Parkinsonâs, Lewy bodies â abnormal buildups of protein â may accumulate in the cerebral cortex, which regulates memory and cognition, and the limbic system, which regulates pain and overall mood. These accumulations cause non-motor symptoms, including fatigue, anxiety, and memory issues. In some cases, these bodies will gradually cause dementia. It typically takes years of living with Parkinsonâs before these symptoms occur, and not all Parkinsonâs patients will develop dementia. Researchers are attempting to develop a way to predict which patients will experience Parkinsonâs disease dementia.Â
Drug Therapy And Research
If the disease progresses beyond minor symptoms, drug treatment may be indicated. Drug therapy for Parkinsonâs typically provides relief for 10â15 years or more. The most commonly prescribed medication is L-dopa , and this helps replenish some of the depleted dopamine in the brain. Sinemet, a combination of levodopa and carbidopa, is the drug most doctors use to treat Parkinsonâs disease. Recent clinical studies have suggested, in the younger person, the class of drugs called âdopamine agonistsâ should be used prior to levodopa-carpidopa except in patients with cognitive problems or hallucinations. In those older than 75, dopamine agonists should be used cautiously because of an added risk of hallucinations.
Other drugs are also used, and new drugs are continually being tested. It is common for multiple drugs to be prescribed because many of them work well together to control symptoms and reduce side effects. Contrary to past beliefs, starting Sinemet in newly diagnosed people does not lead to early symptoms of dyskinesia . Current knowledge is that the disease progression causes dyskinesias, not a âresistanceâ to the drug.
Quality of life studies show that early treatment with dopaminergic medications improves daily functioning, prevents falls, and improves a personâs sense of well-being.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsons. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.